Published on
Urgent message: When a child presents with periorbital cellulitis with no obvious cause, checking for intranasal foreign body, such as a button battery, is of paramount importance. Serious complications can be avoided if the foreign body is removed in a timely manner.
MAY MOHTY, MD, FAAP, FAAUCM, and JACOB ANDERSON, DO
Preseptal cellulitis, also known as periorbital cellulitis, is a relatively common diagnosis in the pediatric population. It is defined as infection of the space anterior to the orbital septum, a fibrous aponeurosis external to the globe, attaching at the periosteum and extending to the eyelids. When a patient presents with signs of facial and periorbital infection, an important initial step is to rule out the more serious condition of orbital cellulitis, which can confidently be done in the absence of diplopia, reduced visual acuity, abnormal light reflexes, proptosis, and ophthalmoplegia.1 Further aiding in the differentiation of the two entities is the preceding course: preseptal infection is typically preceded by trauma or bacteremia, whereas orbital infection is often preceded by sinusitis.2 This is illustrated in a retrospective study that included 262 children with preseptal or orbital cellulitis; trauma (including insect bites) was much more common in patients with preseptal cellulitis than in those with orbital cellulitis (40% vs. 11%).3
Case Presentation
A previously healthy 3-year-old Hispanic boy was brought in by his mother for treatment because he had facial swelling and redness of the left side of his face (Figure 1). The symptoms were first noted when he awakened in the morning on the day of presentation, and they had progressed, with swelling extending to the left eye, prompting the mother to seek care for him.
Findings on a complete review of systems at presentation were negative; the mother reported no fever, cough, change in activity level or appetite, or preceding illness. She further reported no known history of trauma, insect bites, or prior cellulitis. She did note that approximately 4 days prior to presentation, the patient had experienced a bloody nose, but that this was common for him and that the epistaxis had resolved without treatment.
Observation and Findings
On presentation, the child’s vital signs were as follows:
- Oral temperature: 98.6°F
- Blood pressure: 90/67 mm Hg
- Heart rate: 90 beats/min
- Respiratory rate: 20 breaths/min
- Weight: 14.9 kg
He was not in any distress, was breathing comfortably, and was afebrile. Physical examination findings were significant for dried blood at the left naris; externally, he had gross swelling of the left periorbital area, extending to the medial nose and left cheek, with associated mild erythema. His pupils were equal and reactive, and he had full extraocular range of motion bilaterally. No discharge, chemosis, or proptosis was noted. Examination findings, including oropharyngeal and otic, were otherwise unremarkable.

Diagnostic Studies
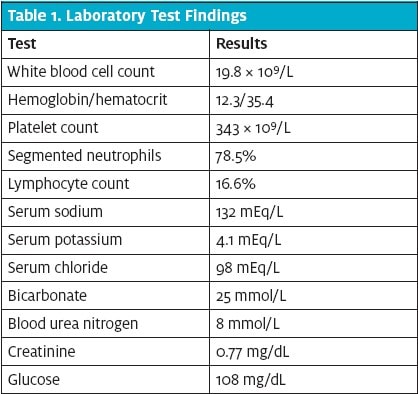
Basic laboratory analysis was performed, including a complete blood cell count with differential and basic metabolic panel, revealing a leukocytosis (Table 1). Because of the leukocytosis, significant amount of facial involvement, and the apparent rapid progression of his condition, he was given intravenous clindamycin and admitted to the general pediatrics floor of the hospital for further evaluation and management of suspected preseptal cellulitis.
When the boy was further examined by the inpatient team, no obvious external causes were found in support of the suspected diagnosis. The patient was noted to have dried blood at the left naris, but the entire nasal vault could not be visualized, so the nose was irrigated and suctioned for improved visualization. Reexamination revealed a metallic foreign body in the posterior vault. The object was controlled and removed with forceps and was identified as an LR44 alkaline battery cell (Figure 2).
The boy showed substantial improvement immediately after removal of the battery. The case was discussed with the on-call otolaryngology team, who recommended no further evaluation or formal consultation because the patient was doing well. The patient was discharged less than 24 hours after original presentation, after being prescribed a 10-day course of oral amoxicillin-clavulanate.
Diagnosis
Intranasal foreign body, button battery, complicated by periorbital cellulitis.

Discussion
Epidemiology
Intranasal foreign bodies are a frequent and often benign cause for presentation to urgent care, as well as in outpatient primary-care settings and emergency departments. Though there are a wide variety of potential household and environmental objects that pose a threat if inserted into the body, the vast majority do not cause significant clinical issues. However, 2 items have the potential for damaging effects: button batteries and magnets. Button batteries, found in many household tools, cause local destruction and alkaline tissue necrosis as a result of their electric charge. Magnets, if paired across tissues, can cause focal pressure and damage.
Clinical Presentation
In up to 88% of cases, patients present with a known foreign-body insertion into the nose without symptoms. In symptomatic patients, clinical findings can include mucopurulent nasal discharge, foul odor, epistaxis, nasal obstruction, and mouth breathing.4 Direct visualization of the foreign body is often readily accomplished without assistance; a nasal speculum or otoscope can be used if the foreign body is suspected to be further posterior or above the superior nasal turbinate.
A high index of suspicion for intranasal foreign bodies is appropriate when assessing toddlers with unexplained nosebleed and signs of soft-tissue infection. When direct visualization is impossible or insufficient, x-rays should be obtained, because unwitnessed foreign-body insertion is common in this age group and has potentially serious consequences. Button batteries and magnet batteries are corrosive to surrounding tissues and are of the great concern in this age group. Complications include nasal septum perforation, which leads to significant cosmetic deformity, and invasive infection of the central nervous system. Although many foreign bodies are not radiopaque, button and magnet batteries are, so x-rays are useful in ruling out these high-risk items.
A Waters view plain film, also known as an occipitomental view, is the radiograph of choice and involves an anteroinferior-to-posterosuperior view at an angle of 45° to the orbitomeatal line.
Specialty consultation is rarely needed, because the majority of foreign bodies can be removed by an experienced health-care provider. However, consultation should be sought in cases of penetrating foreign bodies, septal perforation due to corrosion, posterior foreign bodies that cannot be visualized for removal, or in cases of chronic foreign bodies, which are associated with significant inflammation.5
A further important complication to consider is the risk of cavernous sinus septic thrombosis in any presentation of cellulitis involving the so-called danger triangle of the face, or the medial one-third of the face.
Treatment
Treatment for intranasal foreign bodies consists of removal, which can be performed either through a positive-pressure technique in a cooperative patient with a smooth or soft foreign body, or through direct instrumentation. Positive pressure is accomplished by having the patient blow their nose while occluding the contralateral naris. Direct instrumentation is aided through the use of a topical anesthetic and topical vasoconstrictor. A solution of 1 part 4% plain lidocaine with 1 part oxymetazoline nasal spray is recommended.6 Often, objects can be removed with small forceps; with smooth objects (beads, pebbles) that are not easily grasped, unsuccessful removal attempts can push the object further back. If this occurs, a blunt right-angle hook, a balloon catheter, or a Katz Extractor oto-rhino foreign-body remover can be used. Both a balloon catheter and Katz Extractor work by passing the device beyond the foreign body and inflating the balloon deep to the foreign body, allowing for the removal of the foreign body.
For uncomplicated nasal foreign bodies, antibiotics are not routinely indicated. In cases of suspected infection or, as in this case, complicating periorbital cellulitis, antibiotics should be tailored to the apparent infection. For periorbital cellulitis, therapy is often empiric and based on likely organisms (Staphylococcus, Streptococcus, anaerobes). Recommended regimens include 7- to 10-day courses of amoxicillin-clavulanate plus, if methicillin-resistant S. aureus is suspected, trimethoprim-sulfamethoxazole or monotherapy with clindamycin.7
Conclusion
An urgent care physician should maintain a high index of suspicion for an intranasal foreign body when a child presents with periorbital cellulitis and unexplained nosebleed. If no foreign body is apparent on direct visualization, then occipitomental x-rays can detect batteries or magnets. Early detection and removal can prevent further serious complications.
References
- Howe L, Jones NS. Guidelines for the management of periorbital 1. cellulitis/abscess. Clin Otolaryngol Allied Sci. 2004;29:725–728.
- Givner LB. Periorbital versus orbital cellulitis. Pediatr Infect Dis J. 2002;21:1157–1158.
- Botting AM, McIntosh D, Mahadevan M. Paediatric pre- and post-septal peri-orbital infections are different diseases. A retrospective review of 262 cases. Int J Pediatr Otorhinolaryngol. 2008;72:377–383.
- Claudet I, Salanne S, Debuisson C, et al. [Nasal foreign body in infants]. [Article in French.] Arch Pediatr. 2009;16:1245–1251.
- Mackle T, Conlon B. Foreign bodies of the nose and ears in children. Should these be managed in the accident and emergency setting? Int J Pediatr Otorhinolaryngol. 2006;70:425–428.
- Isaacson GC, Aderonke O. Diagnosis and management of intranasal foreign bodies. Waltham (MA): Wolters Kluwer Health, UpToDate. © 2015 [updated 2014 August 19; cited 2015 May 14]. Available from: http://www.uptodate.com/contents/diagnosis-and-management-of-intranasal-foreign-bodies
- Gappy C, Archer SM, Barza M. Preseptal cellulitis. Waltham (MA): Wolters Kluwer Health, UpToDate. © 2015 [updated 2014 March 10; cited 2015 May 14]. Available from:
- http://www.uptodate.com/contents/preseptal-cellulitis

