Published on
Download the article PDF: Legal Considerations And Urgent Care Management Of Acute Compartment Syndrome In The Upper Extremity
Urgent Message: Compartment syndrome is a limb-threatening emergency that can present with variable clinical signs and symptoms. When the diagnosis is missed or delayed, poor functional outcomes and subsequent malpractice claims are common. Prevention of negative outcomes relies on early detection and a low-threshold for emergency department referrals.
Josie L. Bunstine, DO; Ariel Cohen, DO
Key words: Compartment Syndrome, Medical Malpractice
Questions for the Clinician at the Bedside
- When should acute compartment syndrome be suspected?
- What should be done in the urgent care setting in the case of suspected acute compartment syndrome?
- Does time to surgical intervention impact functional outcomes in patients with acute compartment syndrome?
- How can clinicians avoid medical malpractice situations in cases of acute compartment syndrome?
Abstract
Acute compartment syndrome is a limb-threatening emergency that can present with variable clinical signs and symptoms in the urgent care (UC) setting. It is important for UC clinicians to recognize injuries that predispose to compartment syndrome as well as concerning, early findings suggestive of the diagnosis. This will allow for expeditious referral to an emergency department (ED) where fasciotomy may be performed. Clinicians can improve patient outcomes and limit their exposure to medical malpractice claims by adopting a liberal referral practice for UC patients with suspected compartment syndrome.
Clinical Scenario
A young man presented to an ED after his left arm was crushed between 2 forklifts at work. On physical exam, he was found to have left arm swelling and tenderness of the proximal forearm. He was neurovascularly intact with sensation, motor function, and capillary refill all documented as “good.” X-ray (XR) imaging of the left forearm showed no fractures.
The patient was subsequently discharged home with his left arm in a splint. The aftercare instructions did direct the patient to return to the ED or contact orthopedics if there was new or worsening paleness or a purple color to the hand, numbness/tingling in the hand, difficulty moving fingers, or increased pain. Prior to discharge, the patient was prescribed pain medication. A follow-up appointment with orthopedics was arranged for the next week.
Later in the day, the patient’s mother called the ED because the patient was experiencing increasing pain. According to the physician (after the final diagnosis was known), the staff stated that the patient did not show signs of compartment syndrome. The opioid pain medication was changed to a different agent, which the patient’s mother acquired for him later that evening.
The following day, the patient was still experiencing significant pain. He returned to the ED with complaints of worsening pain and swelling in the left arm. At the second visit, the patient was diagnosed with acute compartment syndrome.
Epidemiology
Compartment syndrome is defined as “an increase in anatomical pressure within a defined myofascial compartment that exceeds the resting pressure of the capillary system.”[1] Increasing pressure leads to collapse of vascular structures, impairing perfusion to local tissues, including muscles and nerves, which can lead to tissue ischemia and necrosis. The upper extremities account for more than 18% of observed cases.1,[2]
Most frequently, acute compartment syndrome is caused by trauma. Swelling after trauma resulting from fractures, hematomas, and/or edema leads to increased pressure within the compartment or restriction of compartment expansion.1,2 The most common fracture patterns resulting in acute compartment syndrome include tibial plateau fractures (especially fractures to the medial plateau with the fracture line extending laterally) and tibial shaft fractures with fracture to the tibial diaphysis accounting for 36% of fractures resulting in compartment syndrome.2,[3] Other fracture types frequently resulting in acute compartment syndrome include the distal radius and diaphysis of the forearm bones.2 Although compartment syndrome should be considered in these scenarios specifically, it is important to assess for increasing compartmental pressures in any patient with extremity-related musculoskeletal pain and injury to avoid poor functional outcomes or permanent limb ischemia.
Relevant Anatomy
The upper extremity contains 15 compartments:2,[4]
- Upper arm flexors
- Upper arm extensors
- Forearm volar (further broken down into superficial and deep layers)
- Forearm dorsal
- Forearm lateral (mobile wad)
- Hand hypothenar
- Hand thenar
- Hand adductor pollicis
- Hand dorsal interosseous (4)
- Hand volar interosseous (3)
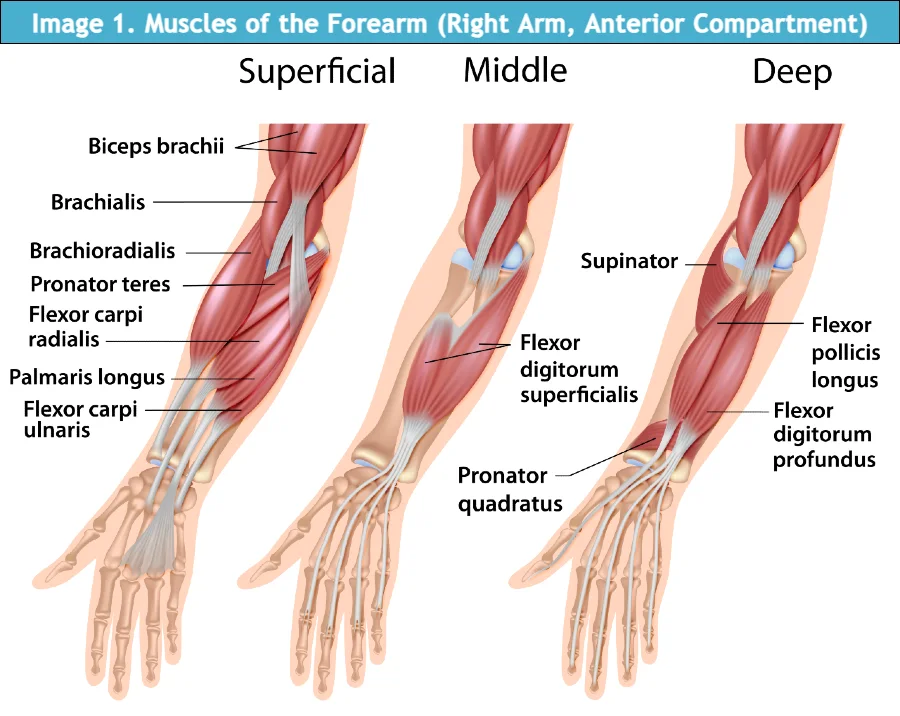
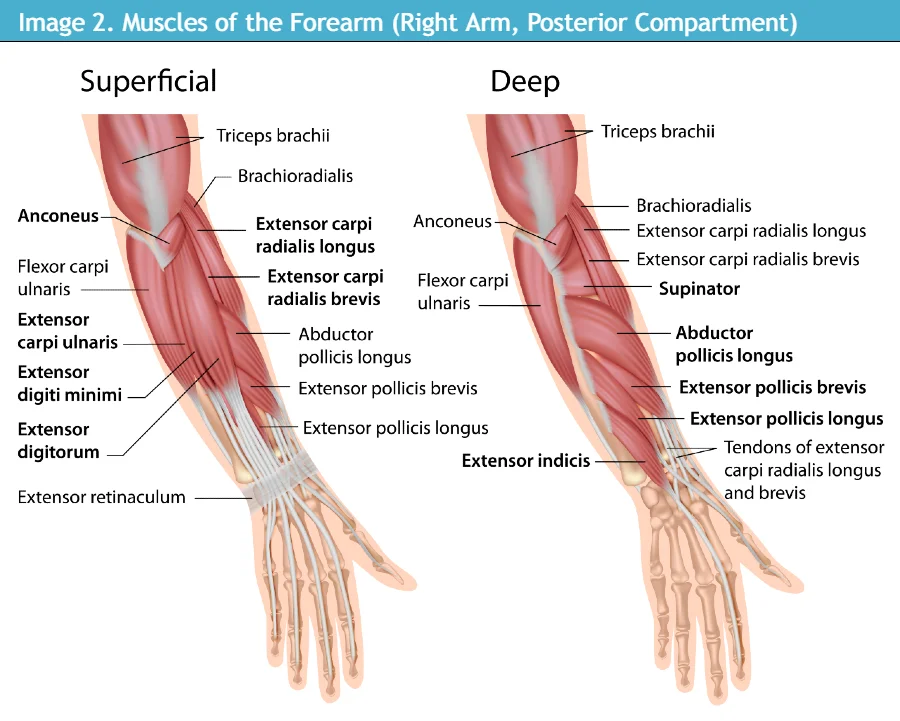
The volar forearm is the most commonly affected compartment in the upper extremity with the deep volar muscles (flexor digitorum profundus, flexor pollicis longus, and pronator quadratus) most commonly damaged (Images 1-2).2 The volar forearm compartment, along with the other compartments in the forearm, are enveloped in antebrachial fascia, which is a continuation of the brachial fascia in the upper arm.2
The more superficial volar muscles are less prone to ischemia.2 The median, anterior interosseous, and ulnar nerve run within the volar compartment; the median nerve is the most commonly affected nerve in cases of forearm compartment syndrome due to its deeper course in the forearm.4
History
History of present illness is an important component of initial evaluation for suspected compartment syndrome. Clinicians should be sure to ask patients about timing and mechanism of injury, any recent causes of external compression (tight casts or bandages, circumferential burns, recent tourniquet use), any recent causes of tissue infiltration (recent IV infusions, infections), as well as any analgesic measures used prior to seeking treatment.1,2 Patients should also be asked about additional locations of pain and other injuries in addition to the chief complaint, as well as new or worsening symptoms including pain, numbness, tingling, change of color of the extremity, swelling, and change in temperature of the affected area.1,2
Reviewing and confirming patients’ past medical history, past surgical history, current prescription medication use and non-prescription medication use (with special attention on medications that impair coagulation), time of most recent medication use, and social history is also important when assessing for possible compartment syndrome.
Physical Exam
The presentation of compartment syndrome can vary widely between patients and is a clinical diagnosis that can be confirmed by objective diagnostic testing. Physical exam of the extremity should include visual inspection (which may involve removal of splints or casts), palpation, active and passive range of motion assessment, and relevant tests depending on the joint(s) related to injury. Thorough assessment of neurovascular function is also critical.
The classic clinical hallmarks associated with compartment syndrome are the “6 Ps.”2,4,[5],[6]
- Pain characteristically out of proportion to the injury (typically the first finding)
- Paresthesia
- Pallor
- Paralysis
- Pulselessness (typically the last finding)
- Poikilothermia (ie, coolness of the extremity, especially distal to the site of injury)
These clinical symptoms importantly rely on a normally conscious and undistracted patient.3 Other features suggestive of possible compartment syndrome include pain with passive stretch of the muscles contained within the compartment of concern and unexpected firmness of compartments on palpation.1 Presence of skin manifestations—such as epidermolysis (loosening of the epidermal layer of skin), cutaneous bullae, and blistering—as well as the hand resting in the intrinsic-position (“claw hand” with extension at the metacarpophalangeal joint and flexion at the interphalangeal joints) may be helpful indicators in these scenarios.5 By the time patients have these symptoms, they have likely already started to experience irreversible sequelae of increased compartmental pressures such as necrosis.3
Imaging and Diagnostic Testing
While compartment syndrome is a clinical diagnosis, certain imaging and testing modalities can be useful for confirmation of suspected compartment syndrome in cases of ambiguity.
- Radiography: XR imaging is useful in screening for bony injury after trauma. Comminuted fracture patterns may suggest higher risk for compartment syndrome.
- Ultrasound: Doppler ultrasound can be helpful in ruling out a vascular occlusion causing pain and swelling to the extremity.9 While ultrasound does not support or rule out compartment syndrome, it is a relatively quick method to exclude venous or arterial thromboses from the differential. Ultrasound may also be used to check for distal peripheral pulses if not felt on palpation.
- Magnetic Resonance Imaging (MRI): While MRI can be used to evaluate further for muscle involvement and ischemic changes in settings of compartment syndrome, it is costly, may not be readily available, and can delay time to treatment.1 Evidence of soft tissue swelling may be present on XR or MRI but is unreliable to support the diagnosis of compartment syndrome alone.1
- Compartment Pressure Measurement: The predominant diagnostic modality for compartment syndrome is intracompartmental pressure measurement, usually with the STIC (solid-state transducer intracompartmental) monitor, colloquially termed the “Stryker needle.”3 This is a portable device that uses a side-ported needle and saline flush with a digital read-out manometer to allow for simple pressure measurements. This should be performed by an experienced operator as measurements can be affected by position, measuring location, and amount of tissue relative to the tip of the needle.3 Pressure may also not be uniform across a compartment. For example, pressure closest to fracture site or site of intracompartmental bleeding may be higher than at sites further from injury.3,[7] These factors make measurement of intracompartmental pressure variable depending on clinician and patient, so they should not be used alone in the diagnosis of compartment syndrome. If using needle measurements to assist in diagnosis, the highest recorded pressure should be used when making decisions about management.7 Some guidelines have suggested that compartment pressures greater than 30 mmHg and/or a difference between diastolic blood pressure and compartmental pressure of less than 20 mmHg is indicative of compartment syndrome, but these thresholds remain controversial.3,5
Urgent Care Management
Acute compartment syndrome is an orthopedic emergency. If suspected in a UC setting, the patient should be immediately referred to an ED for further specialist-level assessment of compartment pressures. In cases of true compartment syndrome, time to fasciotomy heavily impacts likelihood of poor outcomes with muscle necrosis occurring in as little as 3 hours.3 For the forearm specifically, fasciotomy involves releasing the volar, dorsal, and mobile wad compartments.5 Pain medication such as opioids, if available, can be administered prior to ED referral or by paramedics if the patient is transported by ambulance. Any external compression of compartments via cast or splint should be removed as soon as compartment syndrome is suspected.
Next Level Urgent Care Pearls
- In cases concerning for compartment syndrome, UC clinicians should facilitate immediate referral to the ED. This should include calling ahead to the ED and giving report, ideally to the clinician who will be taking care of the patient.
- When referring the patient to the ED, be sure to confirm that the proper specialist will be available for potential fasciotomy shortly upon arrival. Needed specialists may include orthopedics, plastics, trauma, and/or hand surgery.
- Consider how the patient should be referred to the ED (ambulance vs private vehicle). It is important to advise patients to not drive if experiencing severe pain or neurologic deficits.
Red Flags and Legal Pitfalls
Studies of malpractice claims show that compartment syndrome is a diagnosis that is often missed or delayed. When analyzing patient perspectives in cases of medical malpractice, Bhattacharyya et al. (2004) noted that patients commonly reported physical exam findings that were subtle but not investigated further by clinicians.[8] Other frequent allegations included delay in diagnosis, misdiagnosis of compartment syndrome, and poor documentation.8 Risk factors associated with a poor legal outcome for clinicians were identified as:8
- Clinician documentation of abnormal findings on neurological examination but no action taken
- Poor clinician communication (defined in this study as disregarded telephone calls, disregarded nursing requests, poor communication among clinicians, or plaintiff testimony that the physician “did not listen”)
- Higher numbers of cardinal signs (pain, pallor, pulselessness, paralysis, pain with passive stretch)
- Increased time to fasciotomy (most prominent risk factor for indemnity payment)
Based on the Bhattacharyya study, when performing a physical exam on patients with possible compartment syndrome, each of these factors may be important to consider and document when looking to minimize medical malpractice risk. In addition, targeting strategies to improve clinician communication may be beneficial.
In the retrospective analysis of acute compartment syndrome cases by Marchesi et al. (2014), the authors found that the main early symptom of acute compartment syndrome was pain, described as intense, progressive, and intolerable, especially at rest.6 When considering analgesia, it is important to gauge patients’ pain at baseline and suspect compartment syndrome when pain worsens over time, especially without touch or movement and despite typical analgesia. Additionally, none of the clinicians in this study had access to a manometer to measure intracompartmental pressures.
Based on the Marchesi study, when unsure if a patient is experiencing acute compartment syndrome, continuous observation and monitoring in a hospital setting is suggested to watch for developing or changing symptoms. This may lead to fewer errors in diagnosis of compartment syndrome and less delay in time to fasciotomy.6
Clinical Scenario Conclusion
At the second ED visit, a diagnosis of compartment syndrome was made, and the patient underwent volar fasciotomy with debridement. Three days later, he had another surgical debridement, followed by additional plastic surgery. Postoperatively, he attended physical therapy. Despite this care, the patient suffered chronic muscle loss, loss of grip strength, and loss of sensation in the left hand.
The patient subsequently filed a medical malpractice allegation against the orthopedic surgeon, initial emergency medicine physician, and the hospital system. To establish medical malpractice in the state of Ohio—the state where this clinical scenario took place—“it must be shown by a preponderance of evidence that the injury complained of was caused by the doing of some particular thing or things that a clinician or surgeon of ordinary skill, care and diligence would not have done under like or similar conditions or circumstances, or by the failure or omission to do some particular thing or things that such a clinician or surgeon would have done under like or similar conditions and circumstances, and that the injury complained of was the direct and proximate result of such doing or failing to do some one or more of such particular things.”[9]
At trial, multiple orthopedic surgery and emergency medicine expert witnesses testified, with the outcome ruling in favor of the physician and ED group. A jury decided that the initial ED physician did comply with the accepted standard of care of a reasonably prudent emergency room physician when treating the patient. The case was appealed with the original decision being upheld.[10]
Although the physician was not found liable, there were some instances of opportunities for improvement in care and documentation that emerged from trial proceedings. These include the following:
- Earlier suspicion for compartment syndrome, given the mechanism of injury
- Recognizing the presence of increasing pain over time (that may or may not be in proportion to physical findings), suggesting a developing compartment syndrome
- Obtaining a formal orthopedic consultation as soon as concern for compartment syndrome arose and documenting what was discussed as well as the specific recommendations of the orthopedic surgeon
- Obtaining compartment measures of the injured arm
- Re-evaluating the patient before prescribing an alternative pain medication
- Providing the patient with specific discharge instructions and information about compartment syndrome so that they can monitor for new or worsening symptoms
- Admitting the patient to the hospital for observation if they are unable to monitor for new or worsening symptoms on their own or are unable to return to the UC/ED on their own
Ethics Statement
Attempts to contact the patient for presentation of this case were unsuccessful, and therefore some details of the case were changed to protect patient anonymity and confidentiality.
Takeaway Points
- Acute compartment syndrome is an orthopedic emergency. If suspected, patients should be referred to the ED for immediate orthopedic surgery consultation.
- Patient presentation concerning for acute compartment syndrome can be widely variable in signs and symptoms. Increasing pain, especially without movement, is an early finding, and pulselessness is a late finding.
- Time to fasciotomy is the most important factor in long-term functional outcomes of patients, as well as being the most prominent risk factor for indemnity payment in medical malpractice cases.
Manuscript submitted April 18, 2025; accepted May 6, 2025.
References
- [1]. Miranda-Klein J, Howell CM, Davis-Cheshire M. Recognizing and managing upper extremity compartment syndrome. JAAPA. 2020;33(5):15-20. doi:10.1097/01.JAA.0000660124.51074.e5
- [2]. Prasarn ML, Ouellette EA. Acute compartment syndrome of the upper extremity [published correction appears in J Am Acad Orthop Surg. 2011 May;19(5):50A]. J Am Acad Orthop Surg. 2011;19(1):49-58. doi:10.5435/00124635-201101000-00006
- [3]. Guo J, Yin Y, Jin L, Zhang R, Hou Z, Zhang Y. Acute compartment syndrome: Cause, diagnosis, and new viewpoint. Medicine (Baltimore). 2019;98(27):e16260. doi:10.1097/MD.0000000000016260
- [4]. Kistler JM, Ilyas AM, Thoder JJ. Forearm Compartment Syndrome: Evaluation and Management. Hand Clin. 2018;34(1):53-60. doi:10.1016/j.hcl.2017.09.006
- [5]. Friedrich JB, Shin AY. Management of forearm compartment syndrome. Hand Clin. 2007;23(2):245-vii. doi:10.1016/j.hcl.2007.02.002
- [6]. Marchesi M, Marchesi A, Calori GM, et al. A sneaky surgical emergency: Acute compartment syndrome. Retrospective analysis of 66 closed claims, medico-legal pitfalls and damages evaluation. Injury. 2014;45 Suppl 6:S16-S20. doi:10.1016/j.injury.2014.10.017
- [7]. Heckman MM, Whitesides TE Jr, Grewe SR, Rooks MD. Compartment pressure in association with closed tibial fractures. The relationship between tissue pressure, compartment, and the distance from the site of the fracture. J Bone Joint Surg Am. 1994;76(9):1285-1292.
- [8]. Bhattacharyya T, Vrahas MS. The medical-legal aspects of compartment syndrome. J Bone Joint Surg Am. 2004;86(4):864-868. doi:10.2106/00004623-200404000-00029
- [9]. Bruni v. Tatsumi. Supreme Court of Ohio. 1976.
- [10]. Kendig v. Martin. Ohio Court of Appeals. 2003.
Read More on This Topic
- Acute Compartment Syndrome—An Urgent Care Review
- Chronic Exertional Compartment Syndrome
- Six Tips to Bulletproof Your Chart: Lessons from the Exam Room and the Court Room
