Urgent message: Eye pain is a common presentation to the urgent care clinic. A provider needs to be able to recognize concerning components of history and physical which require further emergent evaluation.
Lindsey E. Fish, MD
CASE PRESENTATION
History
A 19-year-old female with past medical history significant only for scoliosis presents to an urgent care clinic complaining of left eye pain for the last 3 days. She reports that the pain feels like it is in the eyeball itself and the back of the eye. Pain is worse when she moves the eye, specifically upwards or laterally. She states that today she noticed a little bit of redness in the inside corner of the eye. She denies any trauma, change in vision, eye discharge, foreign body sensation, or recent cold or allergy like symptoms.
Physical Examination
The patient’s vital signs are all within normal limits. The bilateral pupils are round and reactive to light and extraocular movements are intact. Eyelids and periorbital areas are without erythema or swelling. There is mild conjunctival injection of the medial left eye. Visual acuity is 20/20 in both eyes. Fluorescein is negative on the left eye. Intraocular pressure performed in clinic by an automatic tonometer showed right eye pressure of 20 mmHg and left eye pressure of 18 mmHg.
DIFFERENTIAL DIAGNOSIS
- Orbital cellulitis
- Orbital myositis
- Optic neuritis
- Graves’ disease
Orbital cellulitis is defined as infection involving the ocular muscles and fat; however, it does not include the globe itself. Orbital cellulitis is usually caused by bacteria a majority of the time (Staphylococcus aureus and streptococci). Clinical manifestations include pain with eye movements, proptosis, and diplopia. Orbital cellulitis can be sight- or even life-threatening.1-4 The imaging modality of choice for the evaluation of orbital cellulitis is a CT scan of the orbits.
Orbital myositis is defined as an idiopathic inflammation of an extraocular muscle. This appears to be most common in the distribution of cranial nerve III. Clinical presentation includes orbital pain and usually horizontal diplopia, as well as conjunctival injection, ptosis, and proptosis. This may be unilateral or bilateral.5 The imaging modality of choice for the evaluation of orbital myositis is CT scan of the orbits.
Optic neuritis is a broad term to describe disease of the optic nerve, usually resulting in acute vision loss. While it may refer to various rare inflammatory or infectious etiologies, it generally refers to a demyelinating condition, most commonly associated with multiple sclerosis. Besides vision loss, clinical presentation also frequently includes subclinical visual deficits and eye pain associated with eye movement.6,7 The imaging modality of choice for the evaluation of optic neuritis is MRI of the brain and orbits with gadolinium.
Graves’ disease is an overproduction of the thyroid hormone as a result of autoantibodies that bind to the thyrotropin receptor. Clinical presentation includes ophthalmopathy (inflammation of extraocular muscle and orbital fat and connective tissue) which may cause proptosis, impairment of eye muscle function, and periorbital edema. Patients may also complain of diplopia or gritty feeling or pain in the eyes.7,8 Diagnostic workup includes serum thyroid function tests, as imaging is only occasionally helpful.
PATIENT OUTCOME
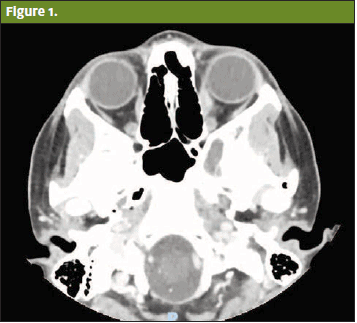
The patient was transported to the emergency department for further evaluation. A CT scan of the orbits was performed and identified asymmetric thickening and mild enhancement of the left medial rectus muscle without significant surrounding fat stranding or fluid collection (Figure 1). Differential for the CT findings include orbital myositis, Graves’-related orbitopathy, orbital pseudotumor, orbital lymphoma, and orbital sarcoidosis. Ophthalmology consult was obtained and the patient was diagnosed with orbital myositis of the left medial rectus muscle. Workup for underlying etiology was negative, including rheumatoid factor, chest x-ray, ANCA, syphilis studies, thyroid studies, and antistreptolysin O (ASO).
The patient was started on prednisone and had resolution of her pain within 5 days. She remained on a prolonged prednisone taper for treatment of her orbital myositis.
DISCUSSION
The diagnosis for this patient was idiopathic orbital myositis, defined as a subtype of nonspecific orbital inflammation which involves the extraocular muscles (specifically the left medial rectus muscle). This presents most frequently in young to middle-aged adults (third decade of life) and affects women twice as often as men.9 This patient had the cardinal clinical feature which included orbital pain made worse by eye movement, specifically in directions mediated by the involved extraocular muscle. It is most often acute and unilateral.10 The patient also had some mild conjunctival injection; however, she did not have other common findings such as diplopia, proptosis, or periorbital edema. Her imaging supported this diagnosis, as her CT scan of the orbits demonstrated an enlarged left medial rectus muscle belly and thickened tendons.
The proposed pathophysiologic mechanism for this disease is unknown; however, it is suspected to be via an immune-mediated pathway. As such, initial therapy is systemic corticosteroid treatment to suppress the presumed immune response. This is usually successful, though there are instances of chronic, refractory, and/or recurrent cases. In one study, there was a 50% recurrence rate.11 In these cases, more aggressive treatment options including immunosuppressant medications or radiation therapy may be indicated.10 There is some indication that rapid diagnosis and treatment may decrease the rate of recurrence and minimize risk for prolonged motility defects and proptosis.12
CONCLUSION
Eye pain is a common presentation to the urgent care clinic. However, eye pain with movement should increase the level of suspicion for orbital etiologies and does warrant consideration of advanced imaging and further evaluation. Etiologies such as orbital myositis, orbital cellulitis, optic neuritis, and Graves’ disease are common with this presentation and may be sight-threatening. As such, the urgent care provider needs to maintain these rarer diagnoses on the differential when evaluating a patient with eye pain.
REFERENCES
- Botting AM, McIntosh D, Mahadevan M. Paediatric pre- and post-septal peri-orbital infections are different diseases. A retrospective review of 262 cases. Int J Pediatr Otorhinolaryngol. 2008;72(3):377-383.
- Seltz LB, Smith J, Durairaj VD, et al. Microbiology and antibiotic management of orbital cellulitis. Pediatrics. 2011;127(3):e566-e572.
- Nageswaran S, Woods CR, Benjamin DK Jr, et al. Orbital cellulitis in children. Pediatr Infect Dis J. 2006;25(8):695-699.
- Sobol SE, Marchand J, Tewfik TL, et al. Orbital complications of sinusitis in children. J Otolaryngol. 2002;31(3):131-136.
- Slavin ML, Glaser JS. Idiopathic orbital myositis: report of six cases. Arch Ophthalmol. 1982;100(8):1261-1265.
- Optic Neuritis Study Group. The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1991;109(12):1673-1678.
- Patel SJ, Lundy DC. Ocular manifestations of autoimmune disease. Am Fam Physician. 2002;66(6):991-998.
- Bahn RS, Heufelder AE. Pathogenesis of Graves’ ophthalmopathy. N Engl J Med. 1993;329:1468-1475.
- Scott IU, Siatkowski RM. Idiopathic orbital myositis. Curr Opin Rheumatol. 1997;9(6):504-512.
- Costa RMS, Dumitrascu OM, Gordon LK. Orbital myositis: diagnosis and management. Curr Allergy Asthma Rep. 2009;9(4):316-323.
- Mombaerts I, Koornneef L. Current status in the treatment of orbital myositis. Ophthalmology. 1997;104(3):402-408.
- Weinstein GS, Dresner SC, Slamovits TL, Kennerdell JS. Acute and subacute orbital myositis. Am J Ophthalmol. 1983;96(2):209-217.

