Urgent message: The capability to identify patients with COVID-19 before they undergo a surgical procedure is essential to the safety of the patient, the surgical team, and postoperative staff. Given the fact that many patients with the virus never exhibit symptoms, proactive preoperative testing in the urgent care center may lower the risk of spread and help quantify the rate of asymptomatic infection.
Sarah Greenwood, PA; Bronson Elizabeth Delasobera, MD; Amanda Joy, PA; Rita Malley, MS; Anisha Patel, MS; and Eshetu Tefera, MS
Citation: Greenwood S, Delasobera BE, Joy A, Malley R, Patel A, Tefera E. Incidence of SARS-CoV-2 in preoperative Patients tested in an urgent care setting. J Urgent Care Med. 2020;15(4):33-36,
INTRODUCTION
The emergence of SARS-CoV-2 in late 2019 and its rapid spread across the world introduced new challenges to healthcare in the United States. With a predicted high demand in healthcare services due to a basic reproductive number of 2.2-2.7 and a case fatality rate of 1.38%,1,2 hospitals and clinics around the country sought to maximize the availability of healthcare personnel and equipment as well as available beds.
One effort to conserve hospital resources and minimize patient and provider exposure to the novel 2019 coronavirus (COVID-19) was to suspend semi-elective and elective procedures at the onset of the pandemic. According to an article published in the World Journal of Emergency Surgery in early April, “When possible, all surgical procedures on all suspected COVID-19 patients should be postponed until confirmed infection clearance.”3 As operating rooms have reopened for nonemergent cases, healthcare systems have adopted various guidelines with respect to preoperative COVID-19 testing to ensure safety for the patients and providers.
As part of the preoperative assessment, most patients are required to undergo COVID-19 testing prior to their procedure. This protocol was put in place, in part, in response to emerging studies that revealed a significant portion of the population may in fact have the virus without displaying symptoms. In fact, one study showed as many as 30% of exposed patients may remain asymptomatic but infected.2
When a nonemergent surgery candidate tests positive for the coronavirus, the surgeon has the opportunity to postpone the procedure depending on the urgency of the surgery. This mitigates unnecessary exposure of the surgical team to the virus and allows for the best postsurgical recovery for the patient. Without question, surgical trauma compromises immune function in the postoperative period. A retrospective study of patients in Wuhan, China revealed postoperative patients positive for COVID-19 received ICU care 44.1% of the time, while nonsurgical patients with the virus required intensive care at a much lower rate of 26.1%. This study suggests surgeries may magnify and exacerbate disease progression in COVID-19 patients.1
In this study, MedStar Health Urgent Care, a large urgent care system spanning Washington, DC, Northern Virginia, and Maryland sought to determine what percentage of preoperative asymptomatic patients tested positive for COVID-19 on a hospital-based PCR testing platform. A secondary objective was to determine if there were certain demographics (ie, gender, age) which led to a higher pretest probability of an asymptomatic positive test. This information can be used to guide best practices for surgical procedures during the SARS-CoV-2 pandemic. Additionally, it can provide insight into larger trends in the population regarding asymptomatic positive prevalence and direct clinical decision-making and use of personal protective equipment in an urgent care setting.
METHODS
Patients scheduled to undergo surgery presented to a MedStar Health Urgent Care facility or urgent care testing tent for a nasopharyngeal (NP) PCR test 1–5 days prior to their scheduled surgery. Prior to testing, all patients had completed a simple set of vital signs and screening questions to ensure they were not displaying any signs or symptoms of COVID-19. Standardized collection procedures were outlined, and the staff was trained by nurse educators to ensure uniform and precise sampling techniques. After testing, all patients were advised to quarantine at home until their surgical date to minimize any new exposures to the COVID-19 virus.
The NP specimen was processed at either Georgetown University Hospital or LabCorp, both doing traditional, open PCR testing on similar platforms. Patients with a surgery scheduled within 72 hours had testing sent to Georgetown Hospital for expedited results, while preoperative candidates due for a procedure in a 3- to 5-day period had testing sent to LabCorp.
Summary statistics including means, medians, standard deviations, first quartiles, third quartiles, and proportions (if categorical) on patient characteristics were obtained. Wilcoxon rank sum test was used to examine differences in the averages of continuous variable between the two groups since normality assumption was not satisfied. Shapiro-Wilk test of normality was performed to inspect the distribution of the continuous variable. The test showed that the data were not normally distributed. Accordingly, we used Wilcoxon rank sum test instead of T-test to examine differences in the averages between the two groups. Chi-square and Fisher exact tests as appropriate were used to investigate differences for categorical variables. Logistic regression analysis was used to examine the extent of association between age and COVID-19 positivity. Odds ratios with 95% confidence intervals were calculated. Statistical significance is defined as p-values £0.05. Statistical Analysis System software version 9.4 (SAS Institute Inc., Cary, NC, USA) was used to perform the analysis.
RESULTS
A total of 1,262 patients scheduled to undergo an elective or semi-elective procedure were tested across eight Medstar Urgent Care facilities and three testing tents between April 28, 2020 and May 26, 2020. The age range of the patients was 6 months to 95 years (median: 58 years old). Females made up 52% of the patients.
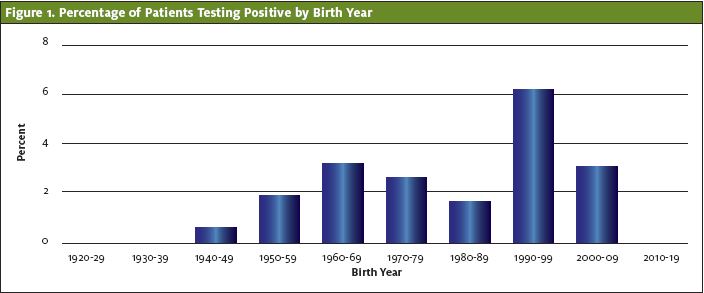
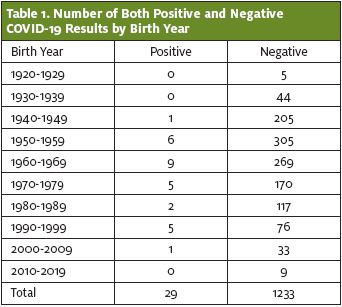
Of this cohort, 29 patients tested positive for SARS-CoV-2 on PCR, and 1,233 patients tested negative. The percentage of patients who tested positive was 2.30%. The 20- to 29-year-old age group had the highest rate of positive cases at 6.2%. Patients over 80 years old or less than 10 years old had no positive cases. (See Figure 1 and Table 1.) However, the difference was not statistically significant (p value=0.24).
Female patients were found to be positive 2.89% of the time, while males were found to be positive 1.65% of the time. However, the difference was not statistically significant (p value=0.14)
Discussion
With a positivity rate of over 2% in asymptomatic patients, the findings from this study support the continued practice of testing for SARS-CoV-2 in all preoperative patients. This enables nonemergent surgeries to be postponed in the event a patient tests positive for COVID-19, thus decreasing unnecessary exposure of preoperative staff, the surgical team, and postoperative personnel to the virus. This testing process also optimizes the chance of a successful recovery for surgical patients, in that nonemergent procedures can be postponed in patients who test positive for SARS-CoV-2.
Due to early limitations in availability, testing in March and April was largely reserved for symptomatic and high-risk individuals. This cohort of asymptomatic preoperative patients was one of the first asymptomatic groups to undergo routine coronavirus testing in the Washington, DC and Baltimore regions. In addition to providing critical information regarding the advisability of surgery in a COVID-19 positive individual, these data can also be utilized to predict current community prevalence of the virus in asymptomatic individuals in the Virginia, Washington, DC, and Maryland region. At the time reflected in the data, Maryland had a 7-day SARS-CoV-2 positivity rate of 13.6%, and Washington, DC had a positivity rate close to 20%; however, these data do not differentiate what percentage of the population was symptomatic.4,5
Previous studies have concluded that a significant proportion, “between 5% and 80%,”6 of patients testing positive are asymptomatic. The CDC estimate is 35%.7 Our study demonstrates the instance of asymptomatic COVID-19 cases may actually be much lower, and asymptomatic spread may be less of a driving force behind the spread of the disease.
Regardless, care must be taken to not minimize risk of exposing surgical staff and patients to the novel coronavirus. However, all healthcare systems need to be aware of the limitations on testing supplies and prolonged turnaround times and should plan their preprocedure COVID testing protocols accordingly.
Our study reveals interesting demographic information on the asymptomatic patient population. Based on these data, even though the 20–29-year-old age group had the highest percentage of asymptomatic positive patients, this percentage was not clinically significant (p=0.24). While disease severity may rise with age in those that display symptoms, our study demonstrates asymptomatic carriers of the disease are equally prevalent in all age groups.
Contrarily, some previous studies have suggested age is a factor in the instance of asymptomatic cases.8-11 One reason might be that our cohort of preoperative patients had a small sample size of patients under the age of 10 (nine patients) and over the age of 90 (five patients). Importantly, our study demonstrates asymptomatic infection across all age groups.
As with age, our study shows that gender is not a factor in rate of asymptomatic COVID-19 cases. While females had a higher rate of positive asymptomatic tests compared with males, this number is not statistically significant (p=0.14). While other studies have shown males have a more serious disease course and higher fatality rate,10,11 our data suggest gender is not a variable in asymptomatic cases. An early study of patients in Wuhan, China shows demographic results similar to ours. In that study, “Symptoms and comorbidities were comparable between men and women…[and] men and women had the same susceptibility.”12
Our data demonstrating that asymptomatic carriers of COVID-19 are prevalent across all age groups and both genders have important implications. Because asymptomatic transmission is an important factor in the spread of the virus, all individuals, regardless of age and gender, should remain diligent to decrease the potential of asymptomatic transmission of the virus. Urgent care providers should take precautions prior to all patient interactions, not just patients with COVID-19 symptoms. Furthermore, these safeguards should be upheld with all patients regardless of gender or age. Additionally, these data suggest there are variables independent of gender and age that influence expression of symptoms of COVID-19.
Limitations
Our study has several limitations. Our population of preoperative patients was not a random sampling; these patients may have decreased coronavirus exposure due to the nature of their illness or injury requiring surgical intervention. These patients tested were not asked to report if they had symptoms on intake screening on the day of testing. The patients were also not followed to determine if they began to develop symptoms after testing and were actually presymptomatic rather than asymptomatic. Furthermore, it was not ascertained if patients had a history of testing positive for SARS-CoV-2 in the past and remained positive on repeat PCR testing despite being asymptomatic. Lastly, there are false negative and false positive rates of any COVID-19 testing; repeat testing was not performed for any of the negatives or positives and results were deemed to be final.
References
- Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. 2020;20(6):669‐677. [Erratum: Lancet Infect Dis, April 15, 2020 and Lancet Infect Dis, May 4, 2020.]
- Sanche S, Lin YT, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477.
- Coccolini F, Perrone G, Chiarugi M, et al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15(1):25.
- Coronavirus.dc.gov. 2020. COVID-19 Surveillance/Coronavirus. Available at: https://coronavirus.dc.gov/data. Accessed July 10, 2020.
- Coronavirus.maryland.gov. 2020. Coronavirus – Maryland Department Of Health. Available at: https://coronavirus.maryland.gov. Accessed 10 July 2020.
- Heneghan C, Brassey J, Jefferson T. COVID-19: What proportion are asymptomatic? The Centre for Evidence-Based Medicine. April 6, 2020. Available at: https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic. Accessed December 10, 2020.
- COVID-19 Pandemic Planning Scenarios. Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. July 10, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html. Accessed December 10, 2020.
- Davies NG, Klepac P, Liu Y, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26(8):1205–1211.
- Yang R, Gui X, Xiong Y. Comparison of clinical characteristics of patients with asymptomatic vs symptomatic coronavirus disease 2019 in Wuhan, China. JAMA Netw Open. 2020;3(5):e2010182.
- Falahi S, Kenarkoohi A. Sex and gender differences in the outcome of patients with COVID-19. J Med Virol. 2020;10.1002/jmv.26243. Epub ahead of print. June 30, 2020.
- Rabin RC. Why the coronavirus seems to hit men harder than women. The New York Times. March 2, 2020.
- Jin J-M, Bai P, He W, et al. Gender differences in patients with covid-19: focus on severity and mortality. Front Public Health. 2020;8:152.
Author affiliation: Sarah Greenwood, PA, Medstar Health Urgent Care/Medstar Ambulatory Services. Bronson Elizabeth Delasobera, MD, Medstar Health Urgent Care/Medstar Ambulatory Services; Georgetown University, School of Medicine. Amanda Joy, PA, Medstar Health Urgent Care/Medstar Ambulatory Services. Rita Malley, MS, Georgetown University, School of Medicine Georgetown University, School of Medicine. Anisha Patel, MS, Georgetown University, School of Medicine. Eshetu Tefera, MS, MedStar Health Research Institute. The authors have no relevant financial relationships with any commercial interests.


