It’s 2021, and the new E/M guidelines for office visit codes are here. Hopefully, providers will feel some relief in the amount they need to document and can spend more time treating their patients. This month I’ll answer some of the questions I’ve received.
Q. Do all three elements of medical decision-making (MDM) need to be at the same level for the code selected?
A. No. Only the two highest elements need to be met for code selection. If the problem addressed is moderate, the data are straightforward, and the risk is also moderate, the level would be moderate or 99204/99214.
Q. If I am billing by time, do I still need to meet that same level for the MDM elements?
A. No. You can select the level of E/M service by MDM or time. If the amount of time meets a level 4 but the MDM only meets a level 2, you would report a level 4. The converse is also true. Which method you use will vary depending on the circumstances of the visit.
Q. For “problems addressed,“ if there is a medical issue that is not evaluated or treated but affects your treatment ( eg, pregnancy), does this count?
A. According to the definition in the guidelines, a problem is considered addressed when it is evaluated or treated at the encounter by the provider reporting the service. Conditions that contribute to the patient’s medical management should be considered as one of the elements when selecting the level of MDM. An underlying disease that has no effect on the data reviewed or risk would not be counted.
Q. Can you clear up the definitions of “acute illness with systemic systems” and “undiagnosed problem with uncertain prognosis”?
A. Both definitions reference the patient having a high risk of morbidity without treatment. Systemic symptoms in a minor illness would be considered self-limited or acute, uncomplicated. “Undiagnosed new problem with uncertain prognosis” is when a differential diagnosis represents a condition likely to result in a high risk of morbidity without treatment.
Q. What is a unique test?
A. Unique tests are a unique CPT code. At the American Medical Association’s CPT® and RBRVS 2021 Annual Symposium, the speakers indicated that a unique CPT would be considered as one point regardless of the number of times it is billed. For example, CPT 87804 is billed twice if both an influenza A and B test are ordered. This would be counted as only one order.
Q. Does ordering a diagnostic test and reviewing that same test count as two points?
A. No. This was clarified in the November 2020 edition of the CPT Assistant. Ordering and reviewing a test are considered a single component for MDM, even if performed on different days. Per the guidelines, ordering a test is included in the category of test result(s) and the review of the test result is part of the encounter.
Q. Can you clarify the difference between review of results and independent interpretation?
A. An independent interpretation is when the provider documents their own interpretation of an image/tracing that was performed elsewhere. It would not be reported if the practice is also billing for the test. “Review of results” is when a provider reviews the test results from another practice. It would not be counted if the billing provider also orders the test.
Q. What is an independent historian?
A. An independent historian is an individual who provides history in addition to a patient who is unable to provide a complete or reliable history or because a confirmatory history is necessary. This may include a parent, spouse, or caregiver. It would not include a translator.
Q. When we send someone to the emergency room, we call the receiving doctor or nurse supervisor to let them know about the patient. Does this count as “appropriate source”?
A. Yes. This would count as discussion of management or test with an external provider. An appropriate source can also be a non-healthcare professional who is involved in the management of the patient.
Q. If a non-physician practitioner discusses the case with a supervising physician that is off-site, does that count for discussion of management with an external physician?
A. No. An external physician cannot be in the same group practice.
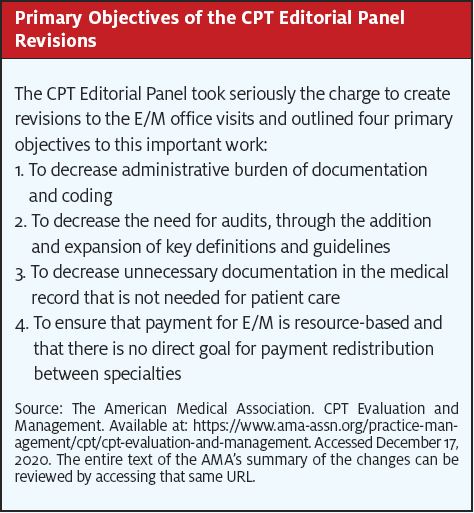
For more information about the new guidelines, including the definitions and the MDM matrix, go to https://www.ama-assn.org/practice-management/cpt/cpt-evaluation-and-management.