Urgent message: Founded by emergency medicine doctors on a mission to keep nonemergent patients out of the ED, urgent care has been forced by changes in reimbursement policies to emphasize high productivity and labor cost savings—ultimately leading to overall fewer procedures and thus a lower acuity level for urgent care centers.
Benjamin Barlow, MD; Monte Sandler; Alan Ayers, MBA, MAcc
The urgent care community has faced many challenges over the past several years. The largest was opening our doors to millions of patients in need of COVID-19 testing when no other options existed. Urgent care centers tackled this challenge by increasing the efficiency and speed of registration, innovating testing access solutions, and developing new workflows to accommodate rapid patient flow and treatment.
We are now facing another challenge.
Degradation in the scope of care provided in urgent care clinics represents a serious threat to the industry. Though the COVID pandemic was a catalyst for this trend, it is not new. It has also refused to disappear as the pandemic’s effects continue to wane.
When urgent care was first popularized by emergency medicine physicians 20 years ago, the focus was on keeping patients out of the emergency room and orthopedic offices. Thanks to the training and skillset of ER physicians, they could perform laceration repairs, casting, EKGs, fluid hydration, and other “complex” procedures.
These services were reimbursed by insurance companies with a fee-for-service (FFS) model, offering urgent care clinics a lucrative payout while still presenting value to consumers versus a trip to the emergency room.
The degradation of urgent care’s scope of practice began as payers shifted away from the FFS model and started using a case rate.
This new form of reimbursement offered a flat fee, based on a weighted average of all services, for each visit. In response, the industry started to focus on cases that could be treated most efficiently. We also saw patients per hour per provider become the main KPI in urgent care.
The COVID pandemic sped these trends up considerably.
As lines of patients seeking COVID testing and care gathered outside our centers during the summer of 2020, urgent care was forced to adapt once again. Suddenly, a patient needing a laceration repaired, an x-ray for an injured ankle, or an abscess drained waited for hours in a sea of COVID patients.
Unfortunately, for many of these non-COVID patients, the ED or the primary care office became a faster and more reliable option. This is a complete reversal of what patients experienced before the pandemic.
Meanwhile, the industry saw a huge influx of advanced practice providers. This trend had also been evident before the pandemic, as EM doctors are both expensive and difficult to recruit. As a result, family medicine providers and APPs became the standard for urgent care. Today, 84% of providers working in urgent care clinics are APPs (Figure 1).
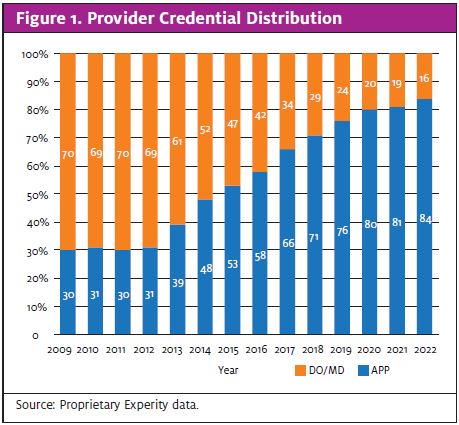
This presents another set of challenges. Nurse practitioners have a narrower skillset than physicians. Thus, extra training and education are required for procedures like laceration repair, reading x-rays, and reading EKGs.
Before the pandemic, newly hired urgent care APPs went through a training period alongside a physician or seasoned APP. They were given time to learn additional procedural skills and how to form and work up a differential diagnosis in the urgent care setting.
The pandemic practically eliminated this ramp-up period for newly hired APPs out of necessity to handle the massive patient volume. Many APPs who started working during the pandemic have only seen COVID patients, many of whom had no or very mild symptoms.
With APPs making up most of the provider base in urgent care and COVID patients flooding waiting rooms, the industry made some tough decisions.
Many centers moved away from x-ray, EKGs, and other high-acuity procedures for which demand was low and fell outside of an NP’s skillset. Instead, they focused on low-acuity head and chest conditions.
Some operators took things further, opening “pop-up” or “limited urgent care” centers. These facilities were designed without x-ray capabilities or procedure rooms despite payer contracts that define urgent care as offering extended/night/weekend hours, x-ray, rapid lab tests, and procedures.
As a result, many urgent cares now refer higher-acuity cases out to the ED and orthopedic offices rather than treating them internally. Incentivized by hospital ownership searching for downstream revenue, these referrals go against the very nature of urgent care’s original purpose.
Moving away from high-acuity cases has combined with the case rate reimbursement model to create a troubling downward spiral. Thanks to the use of weighted averages, the increase in low-acuity cases over time significantly lowers reimbursement case rates. As urgent care clinics try to recover lost revenue by increasing their efficiency, they take on more low-acuity cases, and the cycle continues.
Data from Experity illustrate several ways the industry is experiencing a degradation in the scope of practice.
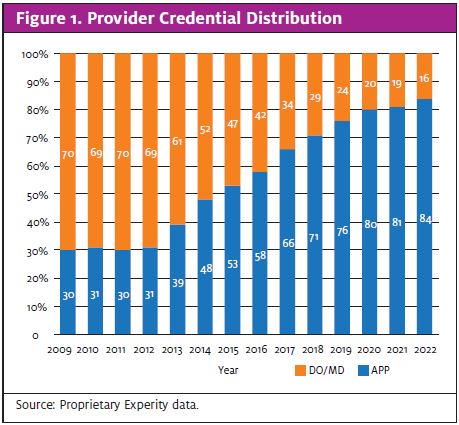
As shown in Figure 2, the average E&M weight and procedure codes for visits is decreasing, down from a high of 3.81 in 2019 to 3.49 in 2022, to date While medicine did go through a coding change, this doesn’t explain the sharp decrease we are observing.
Prior to 2019, the urgent care industry was doing an outstanding job of gradually increasing its scope of practice, as shown by yearly increases in the average E&M code. That is no longer the case.
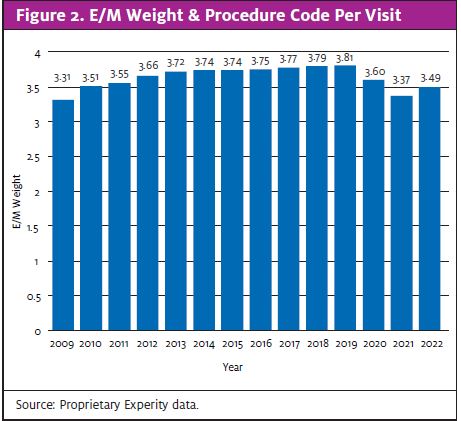
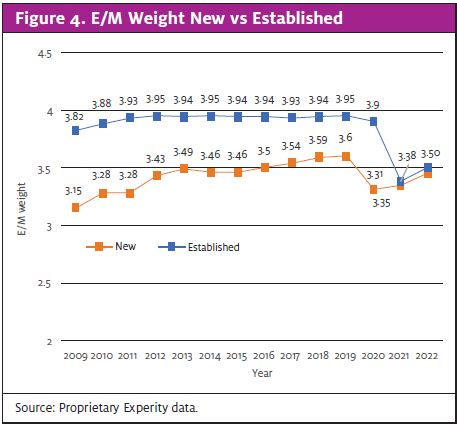
Meanwhile, the percentage of visits with a higher E&M is also decreasing (see Figure 3). This trend is prevalent among new and established patients alike, with both seeing a sharp decrease in E&M weight since the pandemic (Figure 4).
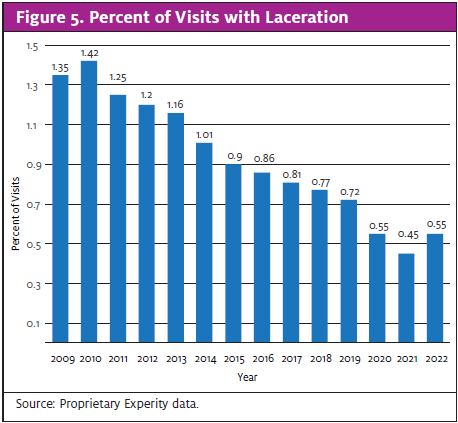
These data correlate with the types of patients we are taking care of in our clinics. Current data show only 0.55% of visits are for laceration repairs (Figure 5). That is a significant decrease from the 0.72% share in 2019 (before the pandemic).
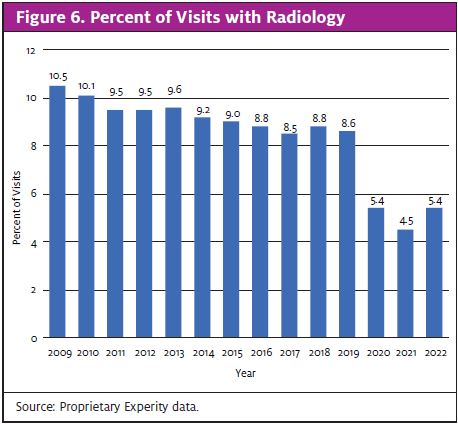
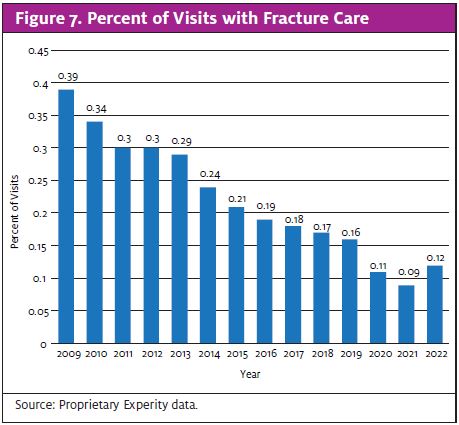
Meanwhile, 5.4% of visits include radiology (Figure 6). This represents nearly a 40% decrease since 2019, when radiology needs accounted for 8.6% of visits. Going hand-in-hand with radiology, 0.12% of current urgent care visits are related to fracture care (Figure 7). That number is also lower than it was in 2019 before the pandemic.
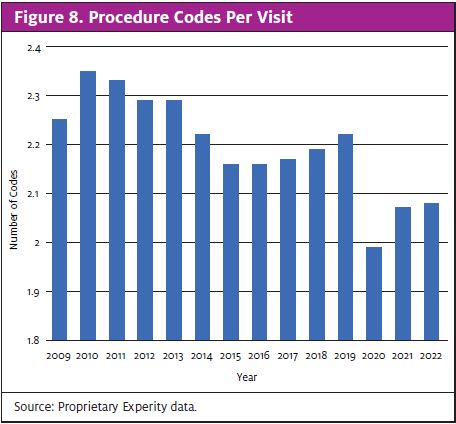
The number of procedure codes per visit has also declined since the pandemic, and failed to recover. It currently sits at 2.08 compared with 2.22 in 2019 (Figure 8).
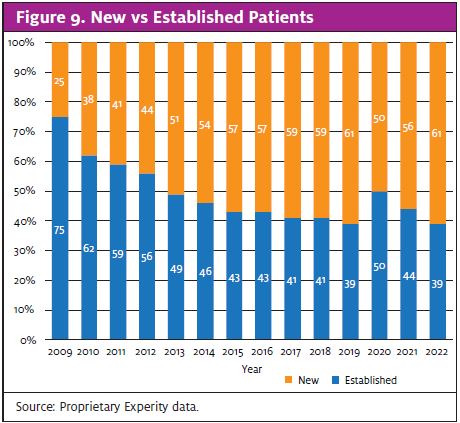
Perhaps one of the more concerning effects of these trends is what the data reveal about new versus established patients. In 2013, new patients accounted for roughly half of all visits. Now, they account for just 39% of visits (Figure 9). Though this change is due to many factors, the degradation of acuity is certainly one of them.
Possible Ways to Reverse the Trends
So, what can we as the urgent care industry do to reverse these trends and recover our advantage in treating high-acuity patients? Let’s take a lesson from the military.
For years, the military has been sending physicians to deployment locations where they handle almost exclusively trauma patients. Before many of these physicians deploy, they receive extensive and renewed trauma training. This prepares them well for the challenges they face during deployment. On returning home, however, many military physicians experience a degradation of their nontrauma medical skills. Procedures like delivering babies, performing lumbar punctures, and managing asthma exacerbations were no longer part of their everyday practice while deployed. There is literature that shows that deployed family physicians gained confidence in trauma skills, but lost confidence in their other medical skills.1
The military’s approach to solving this was to offer postdeployment training for physicians returning home, just as they underwent predeployment training before shipping out. This strategy can be similarly implemented in urgent care.
Providers are now experts in caring for COVID patients. However, responding to the pandemic has come at the cost of losing many essential skills. Procedures that were once an everyday part of urgent care, such as laceration repair and x-ray readings, now fall outside the skillset of many providers.
For urgent care to remain competitive with telemedicine, retail clinics, and on-demand primary care, we must retain our acuity edge. Urgent care offers tremendous value to patients when operating at the top of its scope of practice. This means performing on-site procedures, x-ray services, rapid lab testing, and more—not just referring out to an ER or orthopedic office.
Yet, two problems remain: Providers need to be confident in offering these services, and urgent care centers must find a way to be reimbursed profitably.
One promising solution is education for APPs that serves as an across-the-board refresher and expansion of clinical skills and services. This helps decrease inconsistencies among urgent care clinics and ensures NPs are operating with a consistent skillset.
To develop such a program, urgent care operators must ask themselves tough questions.
- What types of patients did you treat previously that you are no longer taking care of?
- Do your experienced providers agree with the workups and care being provided by your less-experienced providers?
- How do your physicians and APPs feel about their skills and ability to treat lacerations, abscesses, injuries, hypertension, etc.?
- Do your clinics have the necessary supplies to treat higher-acuity patients?
After identifying the deficits, develop a comprehensive plan to help providers and staff gain the knowledge, confidence, and resources they need to provide a higher level of care.
This change doesn’t have to happen all at once.
If you increase your scope of care with the right training and resources, the patients will follow. This process may involve internal training by a knowledgeable provider or staff member, obtaining new supplies, or having providers attend external courses. Ultimately, the approach should be tailored to the unique needs of your operation.
Meanwhile, as the number of high-acuity cases increases, especially among established patients, reimbursement will start to increase once again.
The urgent care industry is comprised of resilient and dedicated people. If COVID has taught us anything, it is that we are highly adaptable. We can recover from the current degradation in the acuity of patients we treat. It will take dedication and a hard look at the data. Yet, with the right training, restocking, and focus, pushing urgent care’s scope of care higher is possible.
REFERENCES
- Reese TR, Deering SH, Kavanagh LB, Maurer DM. Perceived clinical skill degradation of Army family physicians after deployment. Fam Med. 2015 May;47(5):343-348.
Author affiliations: Benjamin Barlow, MD,Experity. Monte Sandler, Experity. Alan Ayers, Experity Consulting;The Journal of Urgent Care Medicine.
Read More
- An Ominous Trend For Urgent Care
- Do You Understand The Three Different Reimbursement Methods For Urgent Care?
- What The #$%^ Is Happening With EM Coding And Reimbursement?! – Part II
- Urgent Care Centers Can Reduce ED Referrals For CT Scans In Mild Head Injury With Integration Of Brain Activity Biomarker



