Urgent message: Lingering warm weather and postpandemic euphoria continue to have patients eager to pursue outdoor activities, including swimming in pools, freshwater lakes, and oceans. Those who have suffered a drowning episode and whose symptoms have resolved may seek care or reassurance at the local urgent care center.
Citation: Davidoff TQ. Evaluation of nonfatal drowning in urgent care. J Urgent Care Med. 2021;15(11):11-14.
Case Presentation
A 4-year-old Hispanic male without significant past medical history is found by his mother flailing in the pool, coughing and choking for an unknown period of time. He is removed from the pool and does not seem to be struggling to breathe but continues to cough periodically. He has no apparent injuries. He presents to urgent care with isolated coughing. He vomits once, mostly water. He is acting appropriately for an active 4-year-old boy playing and interacting with family.
Vital signs are as follows: HR 120, RR 18, BP 90/65, POx 95% on room air. There are no outward signs of trauma. There is no dyspnea, retractions, or accessory muscle use for breathing. His lung exam reveals faint crackles in the midlung zone but good inspiratory effort, no wheezing, and no rhonchi. He coughs once during the exam. The heart and abdomen exams are normal.
What would be your next step in evaluating this patient?
- Reassure the mother that the child is fine and no further workup is required
- Send the patient to the emergency department immediately by EMS
- Observe the patient for an hour. If there is no change, he may be discharged
- Start the patient on steroids immediately to prevent ARDS
- Order a chest x-ray. If normal, discharge; if abnormal, send to the hospital
Discussion
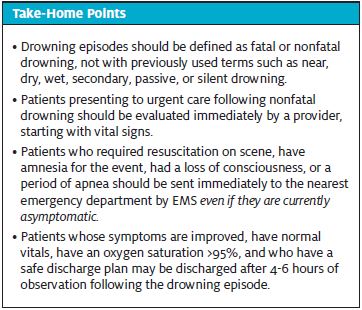
The World Health Organization defines drowning as “the process of experiencing respiratory impairment from submersion or immersion in liquid.” Other terms include near drowning, as well as wet, dry, passive, secondary, and silent drowning; these are no longer recommended as they are confusing and make research and statistic tracking difficult.2 More recent terminology endorses the use of “fatal drowning” and “nonfatal drowning” as defined as death or survival following the episode. This terminology was developed by the World Health Organization and accepted by the American Heart Association to improve consistency in reporting and research.1,2
Drowning accounts for approximately one half million deaths annually worldwide, with likely several hundred times that many for nonfatal drowning episodes.3 Low- and middle-income countries account for more than 90% of these deaths.4
The U.S. reports approximately 4,000 drowning deaths per year. Drowning has surpassed motor vehicle crashes as the most common injury-related cause of death in children.4 About 20,000 children seek medical attention for drowning in U.S. emergency departments annually.5 As many cases of nonfatal drowning go unreported, it is likely that the true scope of the problem is vastly under-estimated.
In the U.S., bathtubs account for 55% of drowning deaths in children less than 1 year of age, with large household buckets accounting for 16%. In children between 1 and 4 years of age, swimming pools are the most likely site of drowning; in children aged 4-20, natural bodies of water are most common. In older populations, natural disasters such as hurricanes or tsunamis are more common causes of drowning.5
The following increase the risk for drowning:
- Inadequate adult supervision, intentional or unintentional, abuse
- Risk-taking behavior
- Use of drugs and alcohol
- Hypothermia
- Concomitant stroke, MI, or trauma
- Seizure disorder, developmental or behavioral disorders, dementia
- Undetected primary cardiac arrhythmia, including familial polymorphic VT, congenital long QT syndrome, Brugada syndrome
- Hyperventilation prior to a shallow dive
Drowning begins with a sensation of panic followed by loss of the normal breathing pattern, breath-holding, air hunger, and struggle by the victim to keep their head above water level. The reflex to inspire eventually occurs, and hypoxemia ensues either by aspiration of liquid or reflex laryngospasm when liquid contacts the lower respiratory tract. Hypoxemia will sequentially affect every organ system, with eventual cerebral hypoxia and death.
Despite earlier beliefs that fresh water and salt-water drownings were physiologically different, researchers have determined that this distinction is no longer important. Both types of drowning result in the same physiologic changes, organ dysfunction, and hypoxia.6 More water than could possibly be aspirated would be necessary for salt water to have any significant difference vs fresh water. Biologic materials such as bacteria, fungus, mud, algae, or chemical contaminants may be of concern and should be considered based on history.
The largest impact on survival of drowning victims is immediate rescue and resuscitation by bystanders at the scene.2 Less than 6% of all rescued persons require medical attention, and <0.5% require CPR.7 Unlike other causes of cardiac arrest where restoring circulation is considered most important, in drowning, ventilation is considered most important and should be initiated as soon as the victim is in shallow water or on a stable surface. If the patient does not respond to two rescue breaths with chest rise, then CPR should be performed with an automated defibrillator, if possible.
Cervical spinal cord injury is uncommon in nonfatal drowning unless there is a mechanism of injury or clinical signs and symptoms consistent with injury. An example of this would be diving or a fall from height. As routine cervical spinal cord immobilization can interfere with airway and respiratory management, this is no longer recommended unless a strong index of suspicion is present for spinal injury.4,6
Hypothermia is a concern in drowning episodes and depends on the temperature of the water and length of time of exposure. This may be less of a concern in patients well enough to present to urgent care, but should still be addressed. Passive warming with blankets for mild hypothermia is recommended.
Risk factors for mortality or significant morbidity following drowning include age <3, submersion for more than 5-10 minutes, and CPR for more than 10 minutes without return of spontaneous circulation.5 If rescue breathing was not required, complete recovery without long term effects regardless of symptoms at presentation usually occurs in 48 hours in all patients.8 The exception to this would be patients that have significant aspiration of chemicals or biologic matter resulting in ARDS, which is fortunately rare.
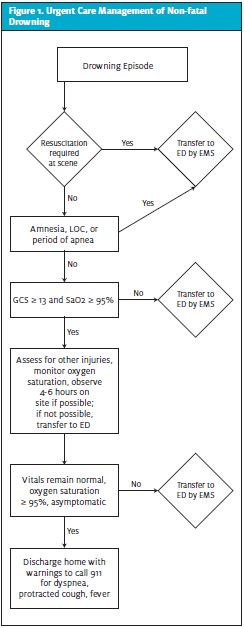
Urgent Care Management (see Table 1)
Most patients who will seek care at an urgent care center following an episode of drowning will arrive in stable condition, awake, alert, and with normal neurologic function. Nearly all of these patients will do well with no decompensation of respiratory function and no permanent neurologic disability.8 Conversely, patients with more severe symptoms, positive physical findings, and abnormal vital signs are at higher risk of morbidity and mortality.
The patient should be evaluated by a provider as soon as possible upon arrival to the urgent care center. Vital signs, including pulse, blood pressure, respiratory rate, temperature, and pulse oximetry should be obtained. Continuous pulse oximetry is recommended. Infrared or tympanic thermometers, commonly used in urgent care, should not be used if hypothermia is suspected as they are less accurate and may not register lower temperatures.
Indications for Transfer
Patients with amnesia for the event, loss of or depressed consciousness at any point, or an observed period of apnea which required artificial ventilation should be transferred by ambulance for evaluation at the emergency department even if they are currently asymptomatic.8 They should be given oxygen if hypoxic or dyspneic and should be warmed if hypothermic.
The majority of patients will have one or more episodes of vomiting due to swallowing water when struggling to breath. This is self-limited, rarely if ever requires treatment, and resolves spontaneously. Patients who have altered mental status and vomiting are at risk for aspiration of gastric contents and advanced airway protection with intubation and mechanical ventilation may be required.
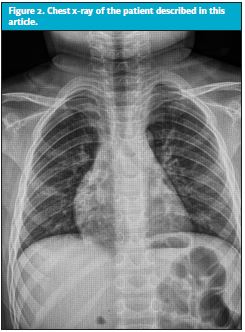
Chest radiographs should be ordered only if there are abnormal lung findings or hypoxia. These films should be interpreted cautiously in the urgent care setting as they may be falsely negative in the early time period after a drowning episode. Initial water in the lungs may be misinterpreted as pneumonia.4 Any radiographic abnormalities found warrant evaluation in the emergency department. Chemistry and hematologic studies are usually normal in the early drowning period and not required in UC if the patient is stable.4,8
Patients with a normal Glasgow Coma Scale score and an oxygen saturation of >95% on presentation are at low risk for complications and should be observed for 4 to 6 hours in a clinical setting. If this is not possible in urgent care, the patient should be sent to the ED for observation. Most patients who decompensate will do so within the 4- to 6-hour time period.
If at the end of the observation period the patient is asymptomatic the pulmonary exam is normal and the oxygen saturation remains >95%, the patient can be safely discharged with little to no risk of complications.8 Long-term survival with no morbidity in these patients is 99%–100%.7 Discharge instructions should include careful observation by a responsible adult and warnings to call 911 for mental status changes, fever, protracted cough, and dyspnea.
Steroids have not been demonstrated to prevent ARDS and improve outcome in these patients and are not recommended.5
In cases of pediatric drowning, neglect or abuse needs to be considered, with referral to children’s services should be made if warranted.
Case Resolution
The provider in this case ordered a chest x-ray based on the abnormal lung exam and borderline hypoxia. Bilateral hilar pulmonary infiltrates consistent with drowning were visible and confirmed by radiology (see Figure 1). Although the patient continued to remain asymptomatic and the oxygen saturation 95%, he was transferred by ambulance to the nearest children’s hospital. He was observed overnight and discharged in the morning with no complications.
Prevention
Drowning is a significant public health problem worldwide. It is estimated that over 85% of drowning episodes could be prevented.4,7 In the U.S., children are at significant risk. This can be mitigated with adequate supervision, physical barriers to water, swimming instruction, and public education measures. Providers should educate the public, especially parents of small children, about safe practices around pools and bodies of water.
References
- Vanden Hoek TL, Morrison LJ, Shuster M, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S829.
- Bulletin of the World Health Organization. 2005;83(11):808-880.
- Salomez F, Vincent JL, Drowning: a review of epidemiology, pathophysiology, treatment and prevention. Resuscitation. 2004;63(3):261-268.
- Mott TF, Latimer KM. Prevention and treatment of drowning. Am Fam Physician. 2016;93(7):576-582.
- Richards DB. Drowning. In: Walls RM, ed. Rosen’s Emergency Medicine Concepts and Clinical Practice. 9th ed. Philadelphia, PA; Elsevier; 2018:1801-1804.
- Battaglia JD, Lockhart CH. Drowning and near-drowning. Pediatr Ann. 1977;6(4):270.
- Szpilman D, Bierens JJLM, et. al. Current concepts: drowning. N Engl J Med. 2012;366(22):2102-2110.
- Tintinalli JE, ed. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. New York, NY: McGraw-Hill Education; 2020:1374-1376.
Tracey Quail Davidoff, MD, FCUCM, Advent Health Centra Care; JUCM Editorial Board. The author has no relevant financial relationships with any commercial interests.

