Urgent message: Respiratory tract infections are a common complaint in the urgent care setting. Many patients present with the expectation of receiving antibiotics because they have usually done so. The rise of anti biotic-resistant infections requires that we take a close look at our prescribing habits and the need to reeducate patients on the harm of overusing antibiotics. Delayed prescribing offers a way to both satisfy patients and reduce the use of antibiotics in respiratory tract infections.
KIM HASBACH, DNP, APRN-BC
Worldwide, overuse of antibiotics has created a growing problem of antibiotic-resistant bacteria. An estimated 60% of antibiotic prescribing for outpatients is for treatment of respiratory tract infections (RTIs). Most RTIs are viral infections, which do not require an antibiotic for treatment and therefore are a target condition where antibiotic use can be reduced safely. Delayed prescribing is one such strategy used to accomplish this. The study reported here examined current practices and attitudes toward delayed prescribing of 8 health-care providers and 27 of their adult patients with an RTI who received a delayed prescription for antibiotics. Participating patients completed a questionnaire about their treatment. Also, the study investigated the effect of an educational intervention for providers regarding antibiotic prescribing. Before and after the intervention, participating providers completed a questionnaire about their knowledge of delayed prescribing. The findings indicated that both patients and providers considered delayed antibiotic prescribing for RTIs a satisfactory treatment choice. In fact, patients expressed a preference for delayed prescribing should they experience similar symptoms in the future. Just over half of the patients did not fill their prescriptions, signifying that delayed prescribing can reduce the use of antibiotics. After the educational intervention, providers reported greater knowledge about the effects of antibiotic prescribing, indicating that the intervention was beneficial.
Introduction
The excessive use of antibiotics has resulted in the development of resistant bacteria. This in turn leads to diseases that are more difficult to manage and prevent. Decreased use of antibiotics is a top priority for quality care1 and may occur when patients are advised to delay filling a prescription for a respiratory tract infection (RTI), unless their symptoms persist or worsen. Delayed prescribing may impact patient satisfaction, provide a safety net for patients with worsening symptoms, and reduce antibiotic use.2 Although delayed antibiotic prescribing is used by many providers, many others are unfamiliar with this strategy.3 By promoting the prudent and efficacious prescribing of antibiotics and thus decreasing unnecessary antibiotic use, providers could have a positive influence in improving health care.
The purpose of the study reported here was to determine whether delayed prescribing decreases the number of antibiotic prescriptions filled and establish whether patient satisfaction is affected for patients aged 19 years or older, treated for RTIs in an outpatient setting. Another objective was to evaluate the influence of an educational intervention on the attitudes and knowledge of health-care providers about delayed prescribing for RTIs. The goals of the study included improving the quality of antibiotic prescribing by increasing awareness and understanding about delayed prescribing, decreasing the unnecessary use of antibiotics, and providing evidence-based prescribing solutions for patients and providers.
Annually, more than 100 million antibiotic prescriptions are written in the United States.4 RTIs, including acute otitis media, pharyngitis, the common cold, acute sinusitis, acute cough, and bronchitis, are the most common reasons for patients to seek outpatient medical care.3 RTIs account for 60% of all outpatient prescribing of antibiotics in ambulatory care.5
Antibiotic prescribing may be influenced by many factors, including patients, providers, and health-care systems.6 Patient factors include sociodemographic and health issues such as the need to return to work, child care, past experiences, care expectations, symptoms, and illness severity. Provider factors include clinical training, diagnostic uncertainty, judgment, fear of litigation, time pressure, and perceived patient expectations. System factors include the practice setting and health plan features, such as co-payments and pharmacy restrictions.7
The unnecessary use of antibiotics may cause the spread of contagious diseases, can increase the duration and severity of infections, may increase the risk of juvenile idiopathic arthritis,8 can cause adverse drug reactions,9 and can add to the rising cost of health care.10 More than 40% of hospital-acquired infections occurring between 1992 and 2004 were caused by methicillin-resistant Staphylococcus aureus (MRSA), which may affect 94,000 persons and result in 19,000 deaths annually in the United States. MRSA is becoming increasingly more common in the community setting. Other infectious agents and diseases of concern in the community are Escherichia coli and drug-resistant tuberculosis. In 1998, the cost of antibacterial resistance to the U.S. health-care system was $5 billion; it is estimated at 10 times that today.11
Prudent use of antibiotics can decrease bacterial resistance to antibiotics.1 Guidelines are available for using delayed prescribing for children and adults who have uncomplicated upper RTIs and who do not require antibiotic prescriptions immediately; these guidelines may help decrease unnecessary use of antibiotics and yet may provide satisfactory care for patients whose symptoms worsen.3,4,12,13 A recent study found that delayed prescribing decreased the use of antibiotics by 76%, without increased risk to the patient, and that patient satisfaction with care was >70%.3 Furthermore, examination of delayed prescribing for pharyngitis, based on the findings of 20 studies, demonstrated that antibiotic use was decreased by 31% with delayed prescribing and by 13% without any prescribing. Delayed prescribing also may be effective for patients with sinusitis who are not at risk for complications. In addition, delayed prescribing may decrease the cost of care, in part from savings on the prescriptions that are not filled; a recent study showed that delayed prescribing was the least costly strategy, compared with others in which antibiotics were not prescribed or were immediately prescribed.3
Methods
Patients
The Troy University Institutional Review Board approved the study reported here. Patients were recruited from an ambulatory acute-care clinic in southwestern Georgia. The walk-in clinic treats patients with sudden illnesses and accidents. The services available include a laboratory, radiography, drug screening, and cardiac monitoring. All patients aged 19 years and older who had a diagnosed RTI and who received a delayed prescription for antibiotics between August and November 2010 were invited to participate in the study. Inclusion criteria followed the guidelines provided by National Institute for Health and Clinical Excellence3 for the use of delayed prescribing. Patients who required immediate prescriptions for RTIs were not included. Figure 1 outlines guideline criteria.

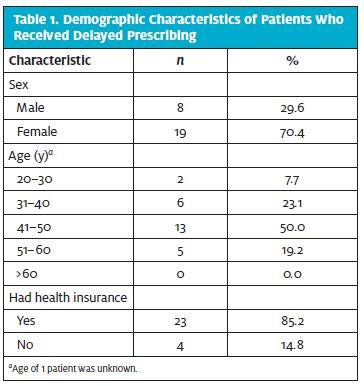
Of the 79 patients who signed the survey consent form, 27 (34%) completed and returned the survey, using the self-addressed, stamped envelope provided. Most of the 27 patients were women, were between the ages of 41 and 50 years, and had health insurance (Table 1). Eight of the 10 health-care providers participated in the educational intervention and survey, including 4 family practice physicians, 3 physician assistants, and 1 nurse practitioner. Because of schedule conflicts, 2 providers did not participate.
Survey
A survey tool created by Martin et al14 was used with permission to evaluate antibiotic treatment and satisfaction. The tool consisted of 7 questions about delayed prescribing and 3 demographic questions. One question on the Martin survey was excluded because this survey was given only to patients who received delayed prescribing (Table 2). The excluded question asked whether the patient received an antibiotic. Patients treated with delayed antibiotic prescribing were given a survey form and a stamped envelope, addressed to the clinic. No personal identifiers were required. The patients were asked to return the survey within 2 weeks after their clinic visit. The 27 completed surveys were returned according to the study protocol.
An educational intervention for health-care providers was developed that included the following information: (1) a definition of delayed prescribing, (2) information about the risks and benefits of delayed prescribing, (3) the evidence-based clinical guidelines for delayed prescribing, (4) examples of patients eligible for delayed prescribing, and (5) recommended advice for patients about symptom management and duration. The provider participants were encouraged to ask questions. Educational materials, including some for patients, were developed by the Centers for Disease Control and Prevention.12
A 7-question survey was designed for the study reported here to assess provider-delayed prescribing knowledge and attitudes and to evaluate the effectiveness of the educational intervention. Providers completed the survey twice: before the educational intervention and again afterward (Table 3). The provider survey was coded to ensure privacy and enable comparison of the before and after surveys.
Data Analysis
Data were analyzed with SPSS statistical software (version 17.0; SPSS Inc., Chicago, IL). Satisfaction scores were entered into a database as numbers on a Likert scale (0 = excellent; 4 = poor). Provider responses to survey questions were entered as numbers on a Likert scale (0 = unable to answer; 50 = partial knowledge; 100 = sufficient knowledge). The level of measurement was nominal. A chi-square test was used to compare responses to patient surveys, and Spearman rank correlation coefficients were determined between responses to patient survey questions. The provider survey scores before and after the educational intervention were compared with a dependent sample t-test. The level of significance was defined as P < .05.

Results
Most of the 27 patients who returned the survey rated the treatment they received and their satisfaction with delayed prescribing for future use as excellent or good, and none of the patients consulted another health-care provider because of dissatisfaction with treatment (Table 2). Approximately one-half of the patients filled the prescription, and these patients waited at least 1 day before doing so (Table 2).
There was a significant positive correlation between patient assessment of treatment quality and patient satisfaction with delayed prescription (r [27] = 0.48; P = .012). There was a significant negative correlation between time delay to filling the prescription and patient age (r [12] = –0.805; P = .002). There was no significant correlation between replies to other questions of the patient survey.
A significantly greater frequency of patients who rated the quality of received treatment as excellent (4 of 4 patients [100%]) or good (14 of 14 patients [100%]) stated that they preferred delayed treatment in the future, compared with patients who rated the quality of treatment received as average (2 of 9 patients [22%]; df = 4; x2 = 18.9; P <.01). A significantly greater frequency of patients who rated the quality of received treatment as excellent (4 of 4 patients [100%]) or good (14 of 14 patients [100%]) stated that their satisfaction with delayed prescribing in the future was excellent or good, compared with patients who rated the quality of treatment received as average (6 of 9 patients [67%]; df = 6; x2 = 13.8; P = < .05). A significantly greater frequency of patients who preferred delayed prescription in the future (20 of 20 patients [100%]) stated that their satisfaction with delayed prescribing in the future was excellent or good, compared with patients who preferred immediate or no prescription (4 of 7 patents [57%]; df = 6; x2 = 17.7; P = < .01). A significantly greater frequency of patients with health insurance (20 of 23 patients [87%]) stated that they needed an antibiotic for treatment, compared with patients without health insurance (0 of 4 patients [0%]; df = 1; x2 = 13.4; P < .01).
All of the providers participating in the survey stated that they would use delayed prescribing in their practice. A dependent sample t-test was conducted between the total added pretest and posttest scores. Results of the t-test were significant (t(7) = –2.37; P = .050), indicating that the mean score at pretest was significantly lower than the mean score at posttest, demonstrating that providers gained understanding with the educational intervention.
Discussion
The results indicated that delayed prescribing provided a high level of satisfaction for both patients and providers. Furthermore, an educational intervention improved provider knowledge of delayed prescribing as a strategy to decrease unnecessary use of antibiotics for RTIs. These results support previous findings that delayed prescribing can maintain or improve patients’ satisfaction, provide safe treatment for patients with worsening symptoms, and decrease unnecessary use of antibiotics.14,15 Also, previous studies have shown that delayed prescribing may decrease reconsultation rates for similar symptoms and increase patient participation in the plan of care.2,16
Patient satisfaction is an important outcome measure in assessing, evaluating, and providing health care. In addition, patient satisfaction can be useful in assessing and improving the process of care. Patients satisfied with the care received are more compliant with the treatment plan and less likely to seek alternative care.17,18 Therefore, patient satisfaction may provide an incentive for providers to implement quality care in order to stay competitive in the market. Qualitative studies have demonstrated that patients are influenced by more than medical outcomes and that they want to receive instructions, care-coordinated diagnostic tests with follow-up, and compassionate treatment.19
The frequency of filling prescriptions when prescribing was delayed (48%; Table 2) was less than that expected from immediate prescribing. This is consistent with the results of 4 randomized controlled studies that showed decreased antibiotic use with delayed prescribing in RTIs.3
Interventions to decrease unnecessary use of antibiotics are most effective when the provider and patient jointly choose the treatment.1 Patient empowerment is improved with information about treatment options, including delayed prescribing. By using the delayed prescribing strategy, patients may increase their belief that antibiotics are not necessary in some situations.
Successfully performing a task (active attainment) may improve self-efficacy to perform the task or to use the strategy again.20 The study reported here demonstrated that the perceived quality of treatment increased with the use of delayed prescribing and that most of the patients would choose to use this strategy in future treatment, with similar symptoms. Using active attainment with delayed prescribing may enable the patient to determine whether the illness will resolve without the use of antibiotics, and this may decrease the need for future consultations for similar symptoms.21
| Table 3. Survey for Provider Knowledge and Attitudes About Delayed Prescribing of Antibiotics |
| 1. What is delayed prescribing? a. I have sufficient knowledge to answer the question. b. I have partial knowledge to answer the question. c. I cannot fully answer this question with my present knowledge. 2. What are the benefits of delayed prescribing? a. I have sufficient knowledge to answer the question. b. I have partial knowledge to answer the question. c. I cannot fully answer this question with my present knowledge. 3. What are the risks of delayed prescribing? a. I have sufficient knowledge to answer the question. b. I have partial knowledge to answer the question. c. I cannot fully answer this question with my present knowledge. 4. What is the average length of symptoms for respiratory tract infections? a. I have sufficient knowledge to answer the question. b. I have partial knowledge to answer the question. c. I cannot fully answer this question with my present knowledge. 5. Is antibiotic resistance a problem? a. I have sufficient knowledge to answer the question. b. I have partial knowledge to answer the question. c. I cannot fully answer this question with my present knowledge. 6. Does inappropriate antibiotic prescribing contribute to antibiotic resistance? a. I have sufficient knowledge to answer the question. b. I have partial knowledge to answer the question. c. I cannot fully answer this question with my present knowledge. 7. Would you use delayed prescribing in your practice? a. Yes b. No |
Limitations
Although a mailed survey may provide participant anonymity and less selection bias than a telephone survey,12 the frequency of the patient response resulted in a small sample size that limited the statistical analysis. The study population was drawn from 1 acute-care outpatient center, which limits the general application of the results. Interestingly, the providers in the clinic stated that they had a high level of knowledge before the survey, but 2 mentioned that they did not know that guidelines for delayed prescribing existed, and 1 provider stated that her ego influenced her answers because she did not want to admit insufficient knowledge.
Future Research
Future research may include improved methods to increase the number of responses for the patient survey, such as conducting a survey by telephone or offering participants an incentive. Evaluation of patients and providers in varied clinical organizations and geographic locations may clarify the effect of other clinical and socioeconomic factors, such as income, education level, and employment, on patient satisfaction. The answers to the provider survey could be worded differently to increase objectivity of the responses. Further evaluation with different populations, clinical settings, and diagnoses may contribute to the understanding of prescribing strategies and more widely decrease the unnecessary use of antibiotics.
General Implications for Practice
Changes in prescribing practices in primary care need to occur to improve patient outcomes and affect the prevalence of antibiotic resistance in the community. Educating providers about the evidence for delayed prescribing at a practice level increases knowledge and therefore increases acceptance of its safe use in practice. The use of delayed prescribing may decrease antibiotic use and maintain patient satisfaction. Evidence-based clinical practice guidelines for delayed prescribing can satisfy patient and provider factors that may influence antibiotic use, and may decrease subsequent repeat consultations for similar symptoms in the future by increasing patient and provider knowledge and self-efficacy.
Implications for Urgent Care
Urgent care practices have a unique challenge in developing trusting relationships with patients, owing to the nature of the setting. Many patients are seen only once in this setting and others are seen infrequently. The opportunity to establish a trusting partnership is brief and often occurs only once. The study reported here has shown that patients are satisfied with the time spent to educate them about the importance of proper treatment and that overprescribing antibiotics can be harmful. The discussion educates the patient on the benefit of delayed prescribing to them. In such discussions, it is important to inform patients that even if they do not overuse antibiotics, many in their community do, and that such a practice will still affect them. The very act of using delayed prescription is an act, by a health-care provider, of trust and confidence in the patient. The patient, in turn, will be more receptive to messages about the need to reduce antibiotic use and will be more compliant with the plan of care.
References
- Ranji SR, Steinman MA, Shojania KG, et al. Technical Review, No. 9: Closing the quality gap. Vol. 4: Antibiotic prescribing behavior. Rockville, MD: Agency for Healthcare Research and Quality; 2008. AHRQ Publication No. 04(06)-0051-4. Available from: http://www.ahrq.gov/research/findings/evidence-based-reports/qualgap1.pdf
- Newson LR. Delayed prescribing. Practice Nurse. 2009;37:21–26. Available from: http://connection.ebscohost.com/c/articles/36499712/delayed-prescribing
- National Institute for Health and Clinical Excellence. Respiratory tract infections— antibiotic prescribing: prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care (guideline 69). London, UK: National Institute for Health and Clinical Excellence; 2008. Available from: http://www.nice.org.uk/ guidance/cg69/resources/guidance-respiratory-tract-infections-antibiotic-prescribing-pdf
- Wong DM, Blumberg DA, Lowe LG. Guidelines for the use of antibiotics in acute upper respiratory tract infections. Am Fam Physician. 2006;74:956–966.
- Tan T, Little P, Stokes T; Guideline Development Group. Antibiotic prescribing for self limiting respiratory tract infections in primary care: summary of NICE guidance. BMJ. 2008;337:a437.
- Hart AM, Pepper GA, Gonzales R. Balancing acts: deciding for or against antibiotics in acute respiratory infections. J Fam Pract. 2006;55:320–325.
- Zoutman DE, Ford BD, Bassili AR, et al. Factors affecting antibiotic decisions for upper respiratory tract infections I: A survey of family physicians. International Journal of Infection Control. 2008;4:1–7. Available from: http://www.ijic.info/article/view/3031/2214
- Horton DB, Scott FI, Haynes K, et al. Antibiotic exposure and juvenile idiopathic arthritis: a case-control study. Pediatrics. 2015;136:e333–e343. Available from: http://pediatrics .aappublications.org/content/136/2/e333.long
- European Centre for Disease Prevention and Control. Factsheet for general public. Stockholm, Sweden: European Centre for Disease Prevention and Control; 2009. Available from: http://ecdc.europa.eu/en/eaad/antibiotics/Pages/facts.aspx
- Roberts RR, Hota B, Ahmad I, et al. Hospital and societal costs of antimicrobial-resistant infections in a Chicago teaching hospital: implications for antibiotic stewardship. Clin Infect Dis. 2009;49:1175–1184.
- Infectious Disease Society of America. Facts about antibiotic resistance. Arlington, VA: Infectious Disease Society of America; 2009. Available from: http://www.idsociety.org/ AR_Facts/
- Centers for Disease Control and Prevention. Get smart: know when antibiotics work. Atlanta, GA: Centers for Disease Control and Prevention; 2006. Available from: http://www.cdc.gov/getsmart/community/index.html
- Cosby JL, Francis N, Butler CC. The role of evidence in the decline of antibiotic use for common respiratory infections in primary care. Lancet Infect Dis. 2007;7:749–756.
- Martin CL, Njike VY, Katz DL. Back-up antibiotic prescriptions could reduce unnecessary antibiotic use in rhinosinusitis. J Clin Epidemiol. 2004;57:429–434.
- Spurling GK, Del Mar CB, Dooley L, Foxlee R. Delayed antibiotics for respiratory infections. Cochrane Database Syst Rev. 2007;3:CD004417.
- Watson HM. Delayed prescribing in out-of-hours care: a case study. Nurse Prescribing. 2007;5: 451–454. Available from: http://www.magonlinelibrary.com/doi/abs/10.12968/ npre.2007.5.10.27556
- Andrew S, Salamonson Y, Everett B, et al. Beyond the ceiling effect: using a mixed methods approach to measure patient satisfaction. Int J Mult Res Approaches. 2011;5:52–63.
- Chow A, Mayer EK, Darzi W, Athanasiou T. Patient-reported outcome measures: the importance of patient satisfaction in surgery. Surgery. 2009;146:435–443.
- Anderson R, Barbara A, Feldman S. What patients want: a content analysis of key qualities that influence patient satisfaction. J Med Pract Manage. 2007;22:255–261.
- Resnick B. Self-efficacy. In: Peterson SJ, Bredow TS, eds. Middle Range Theories: Application to Nursing Research. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2009:117–146.
- Moore M, Little P, Rumsby K, et al. Effect of antibiotic prescribing strategies and an information leaflet on longer-term reconsultation for acute lower respiratory tract infection. Br J Gen Pract. 2009;59:728–734.
