Resolution
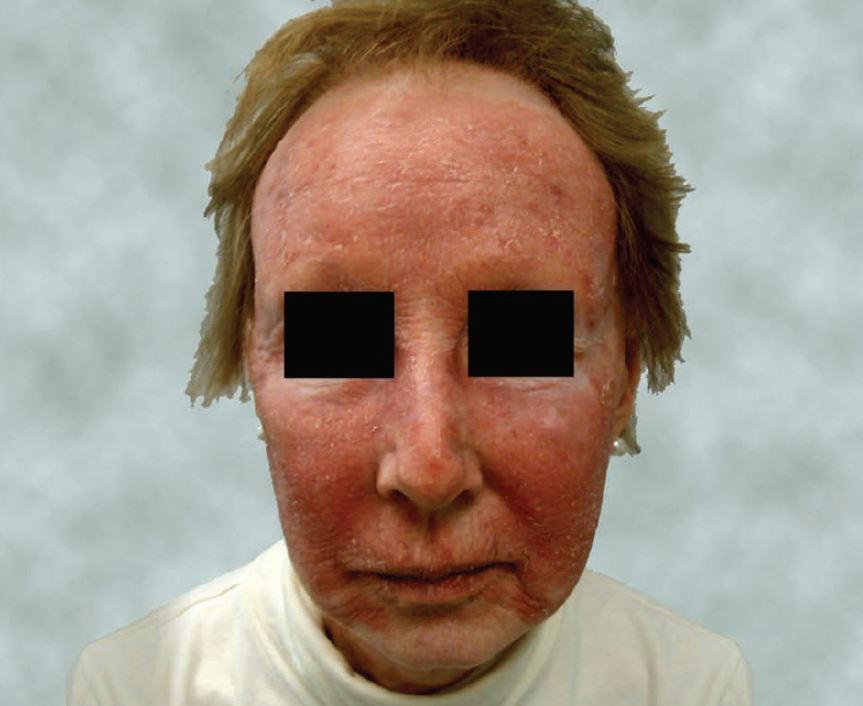
The correct diagnosis is C, tinea faciei, a dermatophyte skin infection confined to the glabrous skin of the face.
In the Northern Hemisphere, the most common pathogens are Trichophyton tonsurans and, less commonly, Microsporum canis. Transmission can be from person to person, pet to person, or from fomites such as athletic headgear or sharing of personal items such as make-up.
Tinea faciei is more common in women than men, but its counterpart, tinea barbae, is seen in the bearded area of men. The classic presentation is of a annular or serpiginous scaling plaques which have an active boarder and, sometimes, central clearing. There may also be papules, vesicles, or crusts.
Because of this varied appearance, tinea faciei is often misdiagnosed. It almost always itches and is made worse by steroids, as in this patient. Diagnosis requires demonstration of hyphae via wet mount with KOH. Scrapings are best obtained using a scalpel or glass slide to obtain a sample from the active border of the lesion.
Cultures can take three to four weeks to complete and are not recommended except in cases where the diagnosis is question or treatment failure occurs. Most cases respond to topical antifungals, but patients should be warned that resolution may take up to four to six weeks. Improvement, however, is usually seen in two weeks.
In this case, hyphae were seen as discoid lupus, polymorphic light eruption, and contact dermatitis. These entities may be clinically indistinguishable from tinea, which is what makes the KOH prep so important.
This patient was treated with clotrimazole cream twice daily. Although steroid containing antifungals may be used for tinea on other parts of the body, steroids are generally not recommended for the face.
Table 1. Topical Treatment of Tinea Faciei* |
||
| Drug | Rx or over=the-counter | Frequency |
| Naftifine 1% cream (Naftin) | Rx | Once daily |
| Terbinafine 1% cream (Lamisil) | OTC | Once or twice daily |
| Butenafine 1% cream (Mentax) | Rx | Once or twice daily |
| Clotrimazole 1% cream (Lotrimin) | OTC | Twice daily |
| Econazole 1% cream (Spectazole) | Rx | Once daily |
| Ketoconazole 1% cream (Nizoral) | Rx | Once daily |
| Miconazole 2% cream (Micatin) | OTC | Twice daily |
| Oxiconazole 1% cream (Oxistat) | Rx | Once or twice daily |
| Sulconazole 1% cream (Exelderm) | Rx | Once or twice daily |
| Ciclopirox 1% cream (Loprox)+ | Rx | Twice daily |
| Tolnaftate 1% cream (Tinactin) | OTC | Twice daily |
| *Typically, creams are recommended over ointments and lotions for the face. +Also exerts an anti-inflammatory effect for more inflamed lesions. |
||
| Resources Noble SL, Forbes RC, Stamm PL. Diagnosis and management of common tinea infections. Am Fam Physician. 1998; 58(1): 163-174, 177-178. Hainer BL. Dermatophyte infections. Am Fam Physician. 2003; 67(1): 101-108. Weinstein A, Berman B. Topical treatment of common superficial tinea infections. Am Fam Physician. 2006; 65(10): 2095-2102. Szepietowski JC, Schwartz RA. Tinea faciei. eMedicine; Feb 1, 2007. Available at: http://emedicine.medscape.com/article/1118316-overview. Wolff K, Johnson R, Fitzpatrick’s color atlas and synopsis of clinical dermatology. 4th ed. McGraw-Hill; 2001: 684-688, 698-699. Susilo R, Korting HC, Staruss UP. Dermatology cases of the glabrous skin. Clin Drug Investig. 2003; 23(6): 387-394. |
||
| Acknowledgement: Case presented by Tracey Q. Davidoff, MD. | ||

