Urgent message: When presented with a patient who has experienced an insect bite or sting, the most crucial role for the urgent care clinician is to triage for anaphylaxis, venom toxicity, and local tissue damage.
Kent A. Knauer, MD
Now that summer is here, it is likely that urgent care practitioners—especially those practicing in suburban and rural areas—will see an increasing number of patients who have experienced
an insect bite or sting.
Though data are scarce, it is accepted that the most common such events leading to an urgent care visit are multiple stings or bites or larger than normal localized swelling—especially worrisome
if on the face or neck. Frequently, there is a small puncture wound visible in the central part of the lesion.
It is important to establish whether a stinger is still present in the wound, and whether the swelling indicates an early cellulitis. More crucial, however, is the need to recognize potential severe injury from some uncommon spider bites. Positive identification of a spider is rare, however; in fact, the identity of the stinging or biting insect is not clear in most cases.
Another area of concern is the potential presence of additional organ involvement such as throat symptoms, possible airway swelling, or a generalized rash. This often occurs in a setting of much patient and/or family alarm. The worst reactions are truly anaphylactic in nature and require prompt aggressive therapy. Some patients need referral to an allergist for further evaluation and treatment.
The Players: Arthropods
Over 60% of the world’s animal species are arthropods. Fortunately, only a small number are venomous and able to cause harm to humans. Among the most common complaints are potentially dangerous stings and bites from arachnids (spiders and scorpions) and Hymenoptera species (bees, wasps, and ants).1 This article excludes a discussion of scorpion stings; a good resource regarding such events can be found in Amitai’s article in Public Health Review.2
Occasionally, a patient presents with multiple, even dozens, of small raised lesiona condition called papular urticaria (Figure1). Often on the legs of young children, these lesions are caused by mosquitoes or chiggers, and although medically harmless, they can cause a few days of intense pruritis and sleepless nights. The treatment includes cool baths and antihistamines, either oral or topical, and topical corticosteroids. Allergic reactions to these insects are rare.
Bite or Sting?
Technically, a bite comes from mouth parts, and a sting from a posterior needle-like structure. Stings are mostly defensive and the venom hurts.
On the other hand, bites are usually meant to kill the victim by various means. Bites from some spiders, therefore, can potentially lead to tissue damage and necrosis.
Only honey bees leave a stinger behind. It should be readily visible on the surface; contrary to popular opinion, it should be removed by any means as soon as possible.
A dark puncture mark at the sting site from other species is not hiding a sting. Most of these creatures sting or bite when attacked or caught, though some sting to defend their nest. Yellow jackets, hornets, and fire ants are the most aggressive, while honey bees and wasps are the least likely to sting. Most spiders bite only when there is a perceived attack.
Bees, Wasps, and Ants
There are three types of reactions to Hymenoptera species: a normal skin response, a large local skin reaction, and a systemic or allergic reaction.3
“Normal” Reaction
Initially, the normal reaction consists of pain, pruritis, or intense burning (fire ants) and a small wheal. Dozens of stings can be inflicted by a swarm of bees, but hundreds of bites can be inflicted by a colony of fire ants within sec- onds. Bee and wasp stings resolve spontaneously over a few hours.
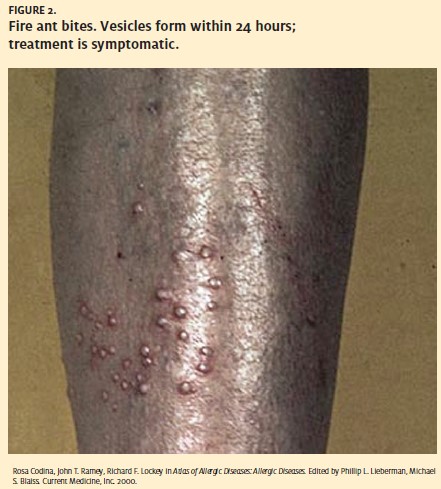
Unlike bee stings, fire ant lesions develop into sterile vesicles within 24 hours. The pustule may last for several days before rupturing and forming a crust which heals over a period of several days (Figure 2). Secondary infection is a possibility in the later stages. Initial treatment is by ice, oral antihistamines, and topical corticosteroids.
Treatment
There is controversy over the use of oral corticosteroids for fire ant bites.4
Large Local Reactions
A large local reaction can occur with bee and wasp stings and consists of a swelling that is larger than normal but is limited to the area adjacent to the sting.
The swelling may cross several joints. For example, a bee sting on the back of the hand could swell up to beyond the elbow.
These reactions progress slowly over hours, and can last up to five days or more. They are alarming but not particularly painful except for stretching of the skin, and they may not itch. They are warm but not necessarily red and usually not tender. The lack of tenderness distinguishes them from cellulitis.
Cellulitis as a result of a bee or wasp sting is rare.
Treatment
Large local reactions should be treated with ice, antihistamines, and oral corticosteroids in a burstand-taper method. They do not require antibiotics. These reactions tend to recur, but usually do not progress to systemic reactions.
Systemic Reactions
Systemic reactions differ in children and adults. In early teens and children, a hive-only reaction may not represent life threatening anaphylaxis, and has a good prognosis for being outgrown. These children have no related gastrointestinal, cardiovascular, or respiratory symptoms. The hive-only reaction may recur but does not progress.5
It is sometimes difficult to determine the presence or absence of other organ system involvement in young children, so when in doubt treat them for anaphylaxis. Heart rate is always increased in anaphylaxis, whereas vasovagal reactions are associated with bradycardia. A serum tryptase level drawn at the time of the sting can be useful at a later time to decide if the event was truly anaphylactic. Tryptase is a specific marker for mast cell activation and mediator re- lease. Skin testing or radioallergosorbent testing (RAST) for venom is the final determinant for allergic sensitization (Figure 3).
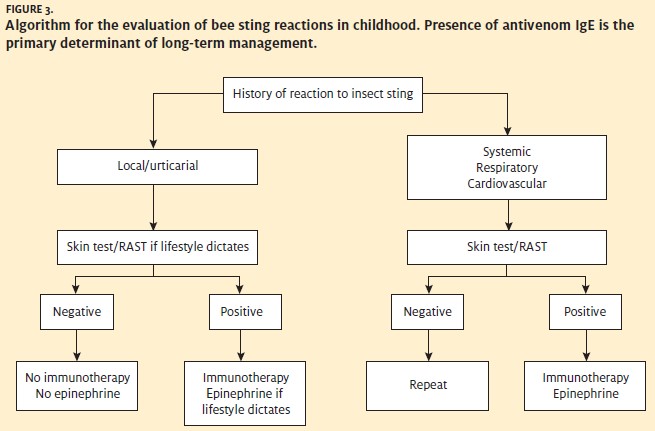
In adults, any reaction outside of the immediate sting site is considered anaphylaxis. These include hypotension; generalized hives; mouth, tongue, or throat swelling; wheezing or chest tightness; and nausea, vomiting, or diarrhea.
Anaphylaxis is IgE-mediated and can occur on any sting other than the first sting. Typically, the reaction proceeds rapidly from itchy palms to generalized hives and itching and then to other organ involvement, but hypotension and loss of consciousness may be the first symptom. On rare occasions, cardiac arrest may occur and death can result, although this is rare and frequently related to the adverse effects of hypotension on underlying medical conditions such as coronary artery disease.
Treatment
After quick assessment, epinephrine (with dose dependent on age and weight) is the treatment of choice, and may be repeated several times if necessary to maintain airway patency or to maintain blood pressure.6 Supplemental oxygen, IV fluids, and parenteral antihistamines and steroids are adjunctive therapies. A common error is to give IV steroids and/or anti- histamines as first-line therapy, presumably out of concern over the safety of epinephrine. Anaphylaxis itself is much more dangerous than epinephrine, and withholding epinephrine for treatment of anaphylaxis can be a fatal mistake. Patients require observation to monitor for secondary late recurrences four to eight hours later. Patients with anaphylaxis need a self-injecting epinephrine device and instructions on when and how to use it.
Allergist referral is recommended for specific venom testing and possible desensitization.
Spiders
Fewer than half of arthropod bites and stings in North America are spider bites. Of these bites, the two species that cause most of the harm are the black widow (Latrodectus species) and the brown recluse (Loxosceles species). These bites have potential for both skin and systemic toxicity, but anaphylaxis does not occur.
Identification and treatment of these bites is complicated by a lack of proper identification of the spider and delays in seeking medical care. Most patients may be able to determine whether the spider was brown or black, and large or small, but very little beyond that unless the spider was captured in a condition to allow identification.
The instinctive reaction is to run away from spiders. (It is amazing that such a small creature can cause a 150-pound mammal to flee in terror!) Both species are nocturnal, and only bite when trapped against skin in bed linen, clothing, or shoes and boots, or squeezed when a hand reaches blindly under an object.7
Initial treatment of a spider bite includes cleansing and application of an ice pack. Parenteral analgesics may be considered. Tetanus prophylaxis is recommended for all significant spider bites. Beyond that, treatment is specific for species and symptoms.
Black Widow Bites
The black widow bite is probably the most important to identify or consider due to the availability of specific antivenin.
The initial bite is commonly on an extremity, usu- ally painful and shows little or no surrounding inflammation. Systemic reactivity is atypical and rarely full blown. When it does occur, generally 30 minutes to two hours elapse before signs of systemic reactivity. First, muscle spasms occur locally at the site of the wound, and then progress centrally to the abdominal and facial muscles. Joint pain, fever, hypertension, and nausea and vomiting may also occur.
Treatment
Benzodiazepines are recommended for treatment of muscle spasm and rigidity. Antivenin is reserved for patients with severe regional or local systemic toxicity, or who have uncontrolled hypertension, seizures, or arrest. One vial is administered in 100 ml to 250 ml of saline over two hours and may be repeated for refractory symptoms. Antivenin may be effective, especially in children, up to three days after the bite, but symptoms generally resolve over two to three days. Death from black widow bites is rare.8
Recluse Spider Bites
Recluse spider bites are initially painless, but localized inflammation spreads rapidly. The venom causes local tissue damage leading to necrosis and ulceration. Systemic reactivity is rare and delayed up to three to seven days; symptoms may include fever, chills, and a maculopapular rash.
Under the best conditions, ulcers heal over one to eight weeks. Major scarring is expected in roughly one in 10 patients. There are essentially no deaths from recluse spider bites.8
Treatment
Antivenin is not available, and systemic manifestations are treated symptomatically. Additional wound care consists of elevation and immobilization of a bitten extremity. The lesion should not be excised, and the wound should not be injected with corticosteroids, since both of these measures may actually make the outcome worse. Wound care continues with debridement, culture and treatment of infection, and ultimately skin grafting if necessary.
Conclusions
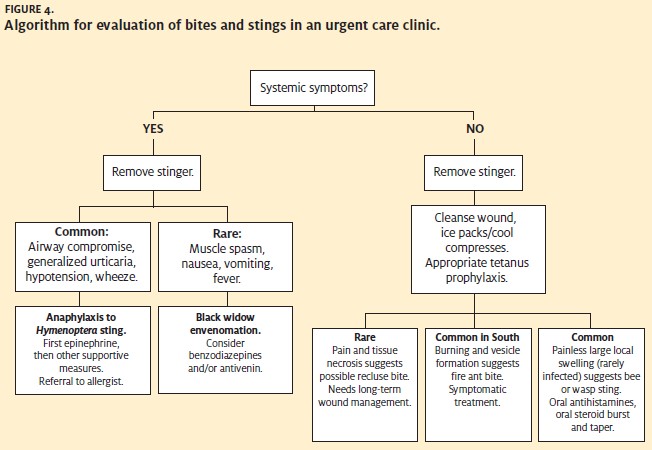
Most insect bites and stings need only local wound care and consideration for tetanus immunization. The role of the urgent care physician is to rapidly triage for anaphylaxis, venom toxicity and local tissue damage (Figure 4). Try to determine the culprit when possible, and the time since envenomation. Determine if there is a past history of an adverse reaction to a bite or sting. If a stinger is observed on the surface of the skin (left only by honeybees), remove it as soon as possible by any means. Don’t waste time searching for a stinger if one is not readily visible.
Signs of anaphylaxis—hypotension, airway compromise, generalized urticaria or angioedema, or wheezingrequire immediate use of epinephrine. In the case of spider bites, observe for signs of systemic toxicity, particularly painful muscle spasms, which indicate the possible need for antivenin treatment.
Analgesics, antihistamines, corticosteroids, and other symptomatic treatments can be helpful in specific situations.2 Epinephrine auto-injectors are prescribed for all patients with anaphylaxis from bee, wasp, or ant stings. Antibiotics are not needed in the majority of cases. Consider consulting with a specialist such as an allergist or surgeon where appropriate. Recommend avoidance measures such as gloves, long sleeves and pants, and insect repellants.
References
- Vetter RS, Visscher Bites and stings of medically important venomous arthro- pods. Int J Derm. 1998;37:481-496
- Amitai Clinical manifestations and management of scorpion envenomation. Pub- lic Health Rev. 1998;26(3):257-263.
- Gupta P, Greenberger Stinging insect allergy and venom immunotherapy. Al- lergy Asthma Proc. 2004;25(4, Suppl 1):S9-10.
- Reschly MJ, Ramos-Caro FA, Mathes Multiple fire ant stings: Report of 3 cases and review of the literature. Cutis. 2000;66(3):179-182.
- Wright DN, Lockey Local reactions to stinging insects (Hymenoptera). Allergy Proc. 1990;11(1):23-28.
- Sheikh A, Walker S. Anaphylaxis. BMJ. 2005;331(7512):330.
- Diaz The global epidemiology, syndromic classification, management, and pre- vention of spider bites. Am J Trop Med Hyg. 2004;71:239-250.
- Diaz JH, Leblanc Common spider bites. Amer Fam Phys. 2007;75:869-873.