Nihar B. Gala, MD
Urgent message: The ability to distinguish between urgent and truly emergent conditions is an essential skill for all urgent care providers. That distinction is especially challenging when symptoms could indicate either a relatively benign diagnosis that is well within the purview of the urgent care setting or a more dire diagnosis better suited for a higher-acuity setting.
Introduction
“Familiar” symptoms such as vomiting, diarrhea, and abdominal pain could be due to a mild viral infection—or, as in this case, a potentially life-threatening emergency. The key to forming the correct diagnosis and providing appropriate medical treatment is in the history and physical examination. This case illustrates the importance of maintaining a wide differential and recognition of distress.
Case Presentation
A 58-year-old gentleman presented to an urgent care center accompanied by his daughter with the complaint of nausea, vomiting, and diarrhea for 2 days. The daughter noted that he had been breathing heavily for the past 24 hours, and that he appeared to be tired.
Past Medical History
The patient’s past medical history included coronary artery disease with previous coronary stent placement, congestive heart failure, diabetes, hypertension, asthma, and alcoholism.
Social History
His daughter revealed that he has a history of alcohol abuse and has recently consumed several alcoholic drinks. On physical examination, the patient was somnolent yet easily arousable, alert, and oriented to person, place, and time. When asked if he was short of breath, the patient said that he was “fine,” only to resume his labored breathing. His vital signs were as follows:
- Temperature: 99.1°F
- Blood pressure: 200/60 mmHg
- Pulse: 105 bpm
- Respirations: 18 breaths/min
- O2 saturation: 68% on room air
- Weight: 242 lb (109.77 kg)
Chest exam confirmed use of accessory muscles for inspiration. Pulmonary auscultation revealed bilateral rales during inspiration and expiration, with symmetric chest expansion. Cardiovascular examination revealed normal S1 and S2 with bounding peripheral pulses bilaterally. He grimaced and guarded his abdomen with deep epigastric palpation. No rebound tenderness or rigidity was noted. He followed commands with all four extremities with full strength on each side. Cranial nerves II to XII were grossly intact.
When he was placed on 100% oxygen via non─rebreather face mask, his O2 saturation improved to 94%.
Testing
A chest x-ray revealed diffuse bilateral pulmonary infiltrates (Figure 1). Electrocardiogram showed sinus tachycardia with no ST changes
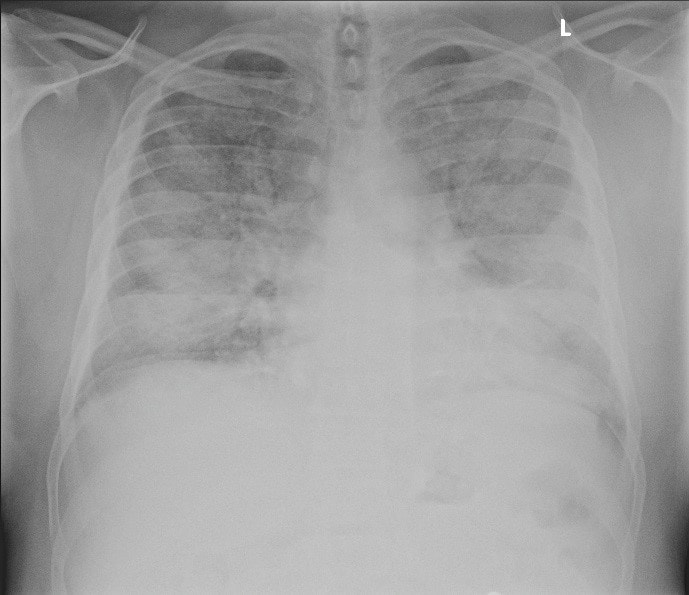
Figure 1. Upright posterior-anterior chest radiograph showing prominent bilateral pulmonary infiltrates.
Differential
- Pneumonia
- Diabetic ketoacidosis
- Acute pneumonitis
- Myocardial infarction
- Sepsis
- Gastritis
- Acute pancreatitis
- Pulmonary embolism
- Acute liver failure
- Acute alcohol intoxication
- Esophageal rupture
- Aortic dissection
- Pulmonary edema
- Pericarditis
- Cholangitis
The key points from the patient’s presentation are:
- Hypoxia
- Systolic hypertension
- Epigastric pain
- Nausea/vomiting
- History of alcoholism
The most critical element of the patient’s presentation is the hypoxia that improves with supplemental oxygen, suggesting a primary pulmonary etiology. Of note, hypoxia may be causing the altered mental status (or, conversely, altered mental status may be causing the hypoxia).
Clinical Course
Paramedics were summoned to transport the patient. He maintained adequate ventilation and oxygenation with no hemodynamic changes, but decompensated en route and was subsequently intubated. Laboratory studies in the ED showed significantly elevated lipase enzymes and a PaO2/FIO2 fraction of 150 mmHg.
Hospital Course
The patient was treated with corticosteroids, invasive mechanical ventilation, and fluid management and was discharged 21 days after admission.
Diagnosis
The patient was diagnosed with acute respiratory distress syndrome (ARDS), likely secondary to acute alcoholic pancreatitis.
Discussion
Approximately 200,000 patients become afflicted with ARDS annually, accounting for 10.4% of all ICU admissions.3,4 The mortality rate ranges from 34.9% to 46.1%, depending on the severity of the disease.4
Although recognized in the 1960s, ARDS was first defined in 1994 by the American─European Consensus Conference (AECC) as the most severe form of acute lung injury, characterized by the acute onset of bilateral pulmonary infiltrates and severe hypoxemia in the absence of cardiogenic etiology.1 The Berlin Definition, published in 2011, defined acute onset of respiratory symptoms within 1 week of known clinical insult; origin of pulmonary edema not fully explained by cardiac failure or fluid overload, requiring objective assessment to exclude hydrostatic edema when no risk factor present; and classification of mild, moderate, and severe ARDS2 (Table 1). The revised definition improved risk factor identification and prognostic determination, increasing the clinical value of epidemiologic studies.
| Table 1. The Berlin Definition of ARDS2 | |
| Timing | Within 1 week of a known clinical insult or new/worsening respiratory symptoms |
| Origin of edema | Not fully explained from cardiac failure or fluid overload, may require objective assessment to exclude hydrostatic edema |
| Chest imaging | Bilateral opacities not fully explained by effusions, collapse, or nodules |
| Oxygenation | |
| Mild | 200 mmHg < PaO2/FIO2 ≤300 mmHg with PEEP or CPAP ≥5 cmH2O |
| Moderate | 100 mmHg < PaO2/FIO2 ≤200 mmHg with PEEP ≥5 cmH2O |
| Severe | PaO2/FIO2 ≤100 mmHg with PEEP ≥5 cmH2O |
ARDS is characterized by three overlapping physiologic phases (Table 2).5,6 In early ARDS, increased permeability of the alveolar─capillary barrier results in accumulation of protein-rich fluids within the alveoli.7 The subsequent release of pro-inflammatory mediators augments pulmonary edema and hypoxemia. The acute phase of ARDS usually resolves completely. However, chronic pulmonary fibrosis often occurs due to accumulation of mesenchymal cells within alveoli spaces. Death is usually a result of progressive multisystem organ failure rather than respiratory deterioration.
| Table 2. The Three Pathophysiologic Phases of ARDS5 | ||
| Exudative Phase | (0-7 days) | Inflammatory mediation of alveolar and endothelial damage resulting in pulmonary edema |
| Proliferative Phase | (7-21 days) | Proliferation of type II alveolar cells resulting in epithelial cell regeneration, fibroblastic reaction, and remodeling |
| Fibrotic Phase | (After 7-10 days) | Collagen deposition in alveolar, vascular, and interstitial beds with development of microcysts |
Causes are varied, and include:
- Pneumonia
- Sepsis
- Transfusion-related acute lung injury
- Severe burns
- Trauma
- Pancreatitis
- Drowning
- Aspiration
- Inhalation injury
- Drug reaction
- Post traumatic fluid over-resuscitation
There is no definitive treatment for ARDS5; however, there has been considerable progress by the use of lung-protective ventilation strategies,8 as well as conservative fluid management.3 Survivors usually begin recovery within 2 weeks of onset and show progressive improvement in pulmonary functional studies up to a year.9
Summary
Patients may present to an urgent care center with a variety of nonspecific symptoms, including nausea and vomiting as a manifestation of more severe illness. A wide differential diagnosis is essential. ARDS has a mortality of 34.9-46.1%, making the timely diagnosis crucial.
Citation: Gala NB. Cardiopulmonary emergency masquerading as gastrointestinal symptoms. J Urgent Care Med. April 2018. Available at: https://www.jucm.com/cardiopulmonary-emergency-masquerading-as-gastrointestinal-symptoms/.
References
Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818-824.
- Force ADT, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526-2533.
- Matthay MA, Zemans RL. The acute respiratory distress syndrome: pathogenesis and treatment. Annu Rev Pathol. 2011;6:147-163.
- Bellani G, Laffey JG, Pham T, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA. 2016;315(8):788-800.
- Pierrakos C, Karanikolas M, Scolletta S, Karamouzos V, Velissaris D. Acute respiratory distress syndrome: pathophysiology and therapeutic options. J Clin Med Res. 2012;4(1):7-16.
- Udobi KF, Childs E, Touijer K. Acute respiratory distress syndrome. Am Fam Physician. 2003;67(2):315-322.
- Cepkova M, Matthay MA. Pharmacotherapy of acute lung injury and the acute respiratory distress syndrome. J Intensive Care Med. 2006;21(3):119-143.
- Bos LD, Martin-Loeches I, Schultz MJ. ARDS: challenges in patient and frontiers in research. Eur Respir Rev. 2018;27(147):17017.
- Valta P, Uusaro A, Nunes S, Ruokonen E, Takala J. Acute respiratory distress syndrome: frequency, clinical course, and costs of care. Crit Care Med. 1999;27(11):2367-2374.
Nihar B. Gala, MD is Medical Director at Alpha Care Medical. The author has no relevant financial relationships with any commercial interests.

