Urgent message: Remain diligent in the evaluation of headache; though often a benign condition, the possibility for severe morbidity and mortality warrants careful evaluation of subtle aspects within the history and/or physical exam.
INTRODUCTION
Headache is one of the most common complaints in the urgent care setting, yet also one that can be daunting for a provider. While there are many benign causes, such as a migraine or tension headache, the potential for an emergent condition exists. Accompanying symptoms can also be vague, making the decision to pursue further work-up even more difficult. Seemingly obvious “red flag” symptoms, like altered gait or level of consciousness, may be subtle in some patients, particularly in the acute setting. With a condition that is so common and often harmless in most patients, a diligent evaluation of the history and physical exam is necessary to recognize the few that truly are emergent headaches.
CASE PRESENTATION
A 54-year-old man with hypertension, migraines, and a history of NSTEMI presented to urgent care with 4 days of a diffuse headache. He was accompanied by his partner. He ranked the pain at 6/10 severity with associated malaise, dizziness, and nausea. He denied neck pain, vision changes, or shortness of breath. In eliciting history, it was difficult to establish a timeline and associated symptoms, as he and his partner reported differing symptoms (cough vs no cough, fatigue vs normal activity). His partner often spoke for him. She was adamant that he was acting normally and did not have altered mental status.
Vitals were T 37.1°C, BP 117/84, P 102, RR 40, O2 95%. He appeared somnolent and in pain but was resting quietly. He followed commands with continued prompting. He was not oriented to place. His gait was slow and unsteady; PERRL with photophobia. His scalp was tender in the occipital region with no nuchal tenderness or rigidity. With the exception of poor dentition, the rest of his physical exam was normal. Lab studies revealed a WBC of 11,000 cells/mm3, ESR of 24 mm/hr and CRP of 15.0 mg/L. All other labs were within normal limits. He was sent to the ED for further imaging.
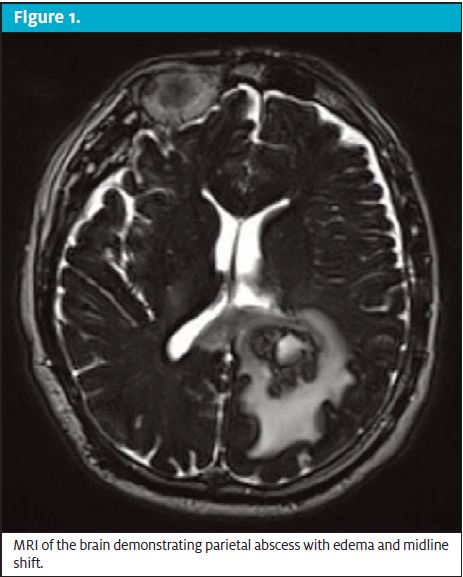
MRI of the brain revealed a 3.1 x 3.0 cm, rim-enhancing mass in the left parietal lobe with significant edema and midline shift (Figure 1). Biopsy confirmed abscess formation; tissue culture revealed Fusobacterium nucleatum and Parvimonas micra. Blood cultures were not suggestive of systemic bacteremia. Transesophageal echocardiogram (TEE) found a small patent foramen ovale (PFO) with right-to-left shunting.
The patient was treated with abscess drainage and a regimen of ceftriaxone/metronidazole with full resolution of his symptoms.
DISCUSSION
The lessons from this case are multifactorial, with implications for both clinical practice and decision-making. Patient communication discrepancies, paired with a vague neurological presentation, created a difficult dynamic for a correct diagnosis.
Brain abscess is not often high on the differential for a headache in an immunocompetent patient. It is a rare finding in the general population, with an incidence ranging from 0.4 to 0.9 cases per 100,000 people.1 Among its rare incidence, it is also frequently associated with immunocompromised status or head trauma.
This patient had neither of these comorbidities. Given his history and lack of focal neurological deficit, it seemed more likely he was experiencing a migraine or other benign source of headache. Symptoms of abscess can be subtle, and since there is no single unifying presentation, it can be difficult to determine the diagnosis clinically. Reports have shown symptoms ranging from blurred vision or memory loss to hemiparesis and fever with rigors; however, these severe symptoms are not always present. The most common triad of brain abscess symptoms—headache, fever, and focal neurological deficit—is complete in just 20% of patients.2 In this case, the patient presented with only one of these three cardinal symptoms.
Lab values in brain abscess can also vary and are not specific. The only commonalities amongst patients in the literature include an increased serum C-reactive protein and leukocyte count, which are only seen in about 60% of patients.3 Ultimately in this case, it was the determination of his subtle altered mental status, alongside the increased serum C-reactive protein and leukocyte count, that warranted head imaging.
Once it was determined his headache was the result of an abscess, the additional question arose about the origin of his infection. Most brain abscesses are seeded either from previous neurologic surgery, injury, or hematologic spread. He was an immunocompetent, nonseptic patient with no obvious infectious symptoms that would point towards a particular location. Confirmation of his right-to-left-shunting PFO raised concern for paradoxical embolism reported rarely in the literature. Dental caries and poor dentition were found on exam, implying the likely infectious origin to be the oral cavity. Biopsy results yielding F nucleatum and P micra, anaerobic bacteria associated with periodontal disease, provided further evidence for this theory.
The first suggestion of brain abscess secondary to paradoxical embolism through a PFO emerged in 2001.3 Few case reports since have detailed cases similar to this patient’s combination of immunocompetent status with a silent, right-to-left shunting PFO and presence of anaerobic bacteria on biopsy. There are reports detailing various combinations of patients with a level of immunodeficiency (ie, IV drug user, COPD) or with other cardiac abnormalities such as Ebstein anomaly or ventricle septal defect.4,5 Though there has yet to be a population study proving a causal relationship between PFO and brain abscess, this report joins the current literature to suggest a correlation.
His silent PFO, which likely acted as a catalyst for disease, serves as a reminder to maintain broad differentials. A paradoxical embolism through a PFO could be more common than one would expect, as roughly 25% of individuals in the general population have been found to have an incidental PFO on autopsy.3 While brain abscesses are rare, their potential for mortality (18%–20% in those with an anaerobic abscess) lends reason to be diligent in the evaluation of a headache.6
Lastly, the patient-partner dynamic in this case highlights the complexity of communication and clinical decision-making in a patient encounter. Studies have shown a positive correlation with family-centered communication and health outcomes, such as increased patient advocacy and trust in the medical system. Physicians have reported that people accompanying patients had a positive influence on medical encounters about 95% of the time.7 However, there is also recognition that inclusion of a third party can complicate the patient encounter and require an expanded communication skillset among physicians. Recommendations from the American Academy of Family Physicians to mediate this situation include: 1) establish the role of the family member, 2) encourage the family member to be specific, and 3) assess the patient in private when indicated.8
In this case, a thorough physical exam resolved communication discrepancies to establish that the patient truly did have altered mental status. This objective data point then served as a foundation to pursue further diagnostic evaluation.
Conclusion
Overall, this case of an immunocompetent 54-year-old man who presented to urgent care with headache and malaise, which ultimately resulted in discovery of a large parietal lobe brain abscess, highlights the importance of maintaining a wide differential. Though symptoms and lab abnormalities of brain abscess may be nonspecific, the potential for morbidity and mortality lends reason to be diligent. Physicians should recognize that the combination of a patent foramen ovale with poor dentition can result in this extreme pathology. In addition, urgent care physicians should remain attentive during patient encounters requiring complex communication skills, particularly involving information that could alter a differential diagnosis.
References
- Brouwer MC, Tunkel AR, McKhann GM, van de Beek, D. Brain abscess. N Engl J Med. 2014;371(5):447–456.
- Sonneville R, Ruimy R, Benzonana N, et al. An update on bacterial brain abscess in immunocompetent patients. Clin Microbiol Infect. 2017;23(9):614–620.
- Kawamata T, Takeshita M, Ishizuka N, Hori T. Patent foramen ovale as a possible risk factor for cryptogenic brain abscess: report of two cases. Neurosurgery. 2001;49(1):204–207.
- Hischebeth GT, Keil VC, Gentil K, et al. Rapid brain death caused by a cerebellar abscess with Fusobacterium nucleatum in a young man with drug abuse: a case report. BMC Research Notes, 2014;7:353.
- Stathopoulos GT, Mandila CG, Koukoulitsios GV, et al. Adult brain abscess associated with patent foramen ovale: a case report. J Med Case Rep. 2007;1(1):68.
- Wexler HM. Anaerobic infections. In: Tang Y-W, Sussman M, Schwartzman, eds. Molecular Medical Microbiology. 2nd ed. Waltham, MA: Academic Press; 2015;875–897.
- Brown JB, Brett P, Stewart M, Marshall JN. Roles and influence of people who accompany patients on visits to the doctor. Can Fam Physician. 1998;44:1644–1650.
- Omole FS, Sow CM, Fresh E, et al. Interacting with patients’ family members during the office visit. Am Fam Physician. 2011;84(7):780–784.
Author affiliations: Rachel Murphy, University of Colorado School of Medicine. Lindsey E. Fish, MD, Denver Health and Hospital; University of Colorado School of Medicine. The authors have no relevant financial relationships with any commercial interests.
View Similar Articles
- Evaluation Of Headaches In Urgent Care Part 1: Emergent Headaches
- Evaluation Of Headaches In Urgent Care Part 2: Non-Emergent Headaches

