Published on
Urgent message:
Asthma is increasing in prevalence and so, too, presentations of asthma in ambulatory settings. Urgent care providers have an important role to play in identifying and treating acute asthma exacerbations, including providing a written asthma action plan at discharge to improve long-term outcome.
BRADLEY M. TURNER MD, MPH, MHA, FCAP, FASCP and JANET M. WILLIAMS, MD, FACEP Patients often seek assistance in urgent care centers for acute presentations of asthma. This provides unique opportunities for short- and long-term management in the urgent care setting. Identification of relevant history, adequate treatment, and appropriate follow-up are essential, and are areas where the urgent care provider plays an important role. Protocols can be helpful in short-term management of the asthmatic patient presenting to an urgent care center. A written asthma action plan at discharge may help to improve long-term outcomes. In the first of a two-part series, we review the epidemiology and pathophysiology of asthma, and provide guidance on key aspects of medical history-taking and examination of the patient who presents for urgent care with symptoms suggestive of asthma. Part 2, in a subsequent issue, will review both short and long-term management of asthma through the use of pharmacotherapy, protocols for treatment, and a written asthma action plan at discharge.
Introduction
Asthma is a multifactorial chronic disorder of the airways, characterized by variable and recurring symptoms, airflow obstruction, bronchial hyper-responsiveness, and an underlying chronic airway inflammation.1-3 Inflammation is a central feature of asthma, and continues to be the foundation for assessment of asthma severity and control of the disease. The prevalence of asthma increased dramatically in the last decade,4 and ambulatory care use for asthma has also continued to increase during this period.2,5 These statistics suggest that urgent care facilities will continue to play a vital role in the short and long-term management of asthma patients.
It is essential that urgent care providers understand the underlying pathogenesis of asthma, and inquire about the risk factors associated with asthma exacerbations. The medical history and subsequent focused examination will provide the foundation for effective short-term management of asthma in the urgent care setting, and proper discharge planning in order to facilitate better long-term management of the disease.
Epidemiology
Asthma data are reported as prevalence (percentage of current population) because there are no national mechanisms in place to measure incidence (rate at which new cases of asthma occur in a population).3 Approximately 34 million Americans (24 million adults and 10 million children) have a diagnosis of asthma.3,6-8 Approximately 12 million (35%) have an asthma exacerbation (a worsening in asthma symptoms that requires a change in the intensity of treatment to prevent further deterioration in clinical status) over a 1-year period.2,3 The prevalence of asthma is higher in non-Hispanic African Americans and individuals with lower socioeconomic status.2-4 The prevalence of asthma increased approximately 12.3% between 2001 and 2009, with an estimated $50.1 billion spent on asthma-related costs in the United States in 2010.4,9 A percentage of these costs were generated by increased use of ambulatory care settings by patients who had an acute asthma exacerbation. Of note, the rates of emergency department (ED) visits, hospitalizations, and mortality for asthma have either held steady or, more importantly, declined over the last decade.3 These patterns suggest that an increasing number of patients with acute asthma exacerbations may present to urgent care centers for treatment and short-term management. In addition, if the pattern of decreased ED visits and hospitalizations is to continue, it is imperative for urgent care providers to provide appropriate and adequate discharge instructions for patients with the goal of preventing future asthma exacerbations. Understanding the pathogenesis is a fundamental building block to this end.
Pathophysiology
Central to the pathogenesis of asthma is presence of underlying airway inflammation.1,3 Airway inflammation is the result of many cell types, whose interactions ultimately result in epithelial cell injury and subsequent airflow limitation. Airflow limitation results in airway hyper responsiveness and/or airway obstruction, both of which result in clinical symptoms of cough, wheeze, and shortness of breath. These clinical symptoms present in a variety of severity patterns that reflect different aspects of the disease, such as intermittent versus persistent asthma, and well versus poorly controlled asthma. Understanding the fundamentals of asthma pathogenesis is a key factor in understanding the rationale behind both short-term and long-term management. Short-term management for asthma exacerbation is directed at controlling inflammation and airflow limitation, using drugs to reduce inflammation and relax the airway musculature in hopes of reversing air-flow obstruction. While short-term management can, to a large extent, reverse some of these processes, reversibility of airflow limitation may be incomplete in some patients with asthma. Long-term management is directed at prevention, through avoidance of triggers, and using drugs that help to reduce airway inflammation, airway hyper-responsiveness, and airflow obstruction. Understanding the rationale behind short and long-term management will lead more efficient assessment and management of patients presenting to an urgent care center with suspected asthma exacerbation.
Medical History and Exam
Patients may present to an urgent care center without a known diagnosis of asthma. While it may not be practical to diagnose asthma in the urgent care setting, an urgent care provider can at least suspect the diagnosis and provide appropriate follow-up care for a patient. A patient’s medical history is essential in establishing whether a diagnosis of asthma is a consideration.
Although short-term management of a patient in respiratory distress may be similar in different diseases, establishing a specific diagnosis of “asthma exacerbation” is particularly important in patients without a known diagnosis for proper short-term and long-term management. The provider trying to establish a diagnosis of asthma should determine that episodic symptoms of airflow obstruction are present and that airflow obstruction is at least partially reversible. Alternative diagnoses should be excluded.1
Table 1 highlights key indicators that have been suggested by the National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program Expert Panel Report 3 (EPR-3) for considering a diagnosis of asthma. Although these indicators are not by themselves diagnostic, multiple key indicators increase the likelihood of a diagnosis of asthma.1 In the initial history and review of symptoms, an urgent care provider should attempt to identify precipitating factors (e.g., exposure at home, work, daycare, or school to inhalant allergens, or irritants such as tobacco smoke, or viral respiratory infections) and comorbidities that may aggravate asthma (e.g., sinusitis, rhinitis, gastroesophageal reflux disorder, obstructive sleep apnea).
The physical exam should focus on the upper respiratory tract, chest, and skin. Physical findings that increase the probability of asthma include1:
- Hyperexpansion of the thorax, especially in children; use of accessory muscles; appearance of hunched shoulders; and chest deformity
- Sounds of wheezing during normal breathing, or a prolonged phase of forced exhalation (typical of airflow obstruction). Wheezing may only be heard during forced exhalation.
- Increased nasal secretion, mucosal swelling, and/or nasal polyps
- Atopic dermatitis/eczema or any other manifestation of an allergic skin condition.
Note that wheezing is not a reliable indicator of airway limitation; however, it is the only physical exam finding that has been suggested as a key indicator for likelihood of a diagnosis of asthma. Although hyperexpansion of the thorax, nasal findings (i.e. nasal polyps), and skin findings (i.e. eczema) are often associated with asthma, they have not been suggested as key indicators by the EPR-3.
Once a diagnosis of asthma is suspected, the provider should consider risk factors associated with worse outcomes (Table 2), which may become important when considering discharge and follow-up.
| Table 2. Risk Factors for Death From Asthma* |
| Asthma history • Previous severe exacerbation requiring intubation or intensive care unit admission for asthma • Two or more hospitalizations for asthma in the past year • Three or more emergency department (ED) visits for asthma in the past year • Hospitalization or ED visit for asthma in the past month • Using >2 canisters of a short-acting beta2-agonist per month • Using >2 canisters of a short-acting beta2-agonist per month • Sensitivity to Alternaria Social history • Low socioeconomic status • Inner city residence • Illicit drug use • Major psychosocial problems Comorbidities • Cardiovascular disease • Other chronic lung disease • Chronic psychiatric disease Other • Lack of a written asthma plan |
| *Adapted from the National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma Full Report [EPR-3]. |
Laboratory testing is essential in assessing the severity of a patient’s presentation. The EPR-3 recommends that office-based physicians who care for asthma patients have access to spirometry. For diagnostic purposes, spirometry is generally recommended over measurements with a peak flow meter because there is wide variability even in the published predicted peak expiratory flow (PEF) reference values. Spirometry, which measures the rate at which the lung changes volume during forced breathing maneuvers, should be performed using equipment and techniques that meet standards developed by the American Thoracic Society. Basic spirometry can be performed in the urgent care setting with relative ease and inexpensive equipment (CPT code 94010 for normal spirometry and both CPT codes 94010 and 94060 for abnormal spirometry with the addition of a pre versus post bronchodilator spirometry test).
Normal spirometry implies a forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) of 80% to 120% predicted, and an absolute FEV1/FVC ratio >0.7. The normal ranges for spirometry values vary depending on a patient’s height, weight, age, sex, and racial or ethnic background. Contraindications to spirometry include vomiting, nausea, vertigo, hemoptysis, pneumothorax, recent abdominal surgery, recent eye surgery, recent myocardial infarction or unstable angina, and thoracic aneurysms.10 If a diagnosis of asthma is not already documented, and cannot be established with spirometry in the urgent care setting, PEFs can act as surrogate data. Any abnormal results should be documented by the provider and the patient should be referred back to either a primary care provider or a specialist with a “suspected diagnosis” of asthma exacerbation.
| Table 3. Differential Diagnosis of Asthma in Infants, Children, and Adults* |
Infants and Children
Adults
|
| *Adapted from the National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma Full Report [EPR-3]. |
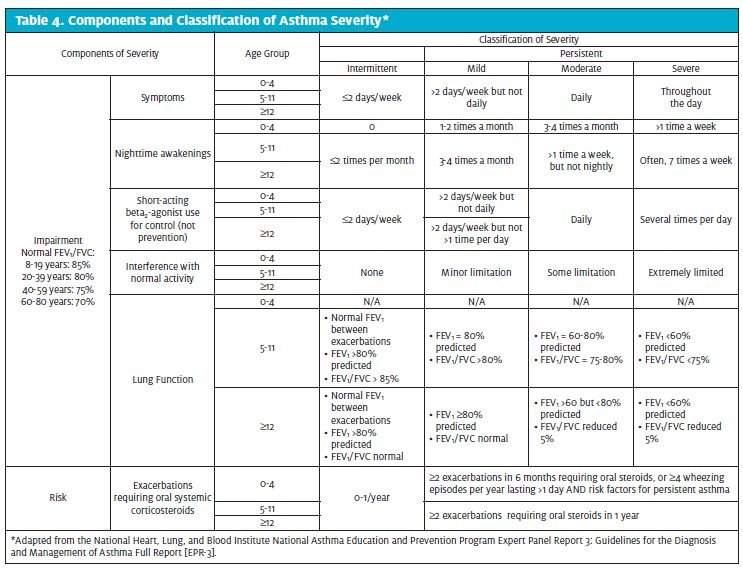
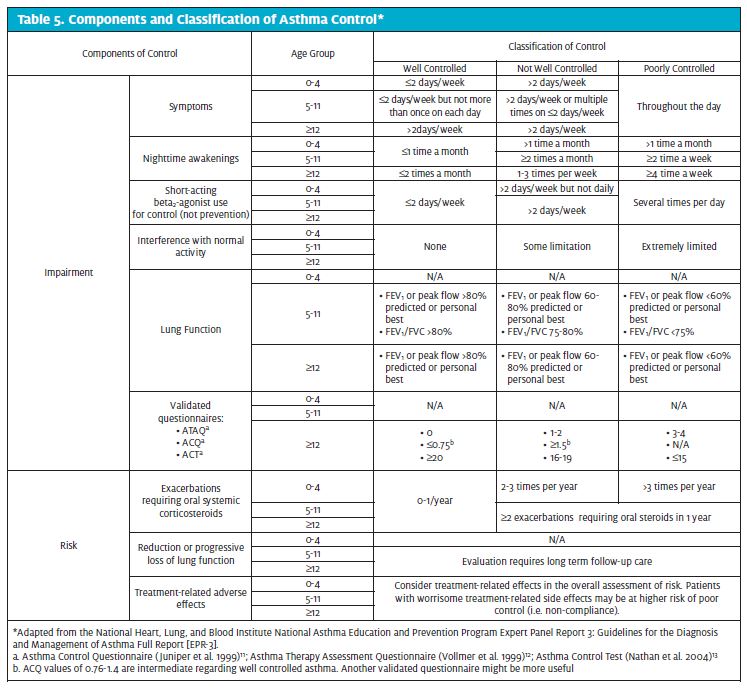
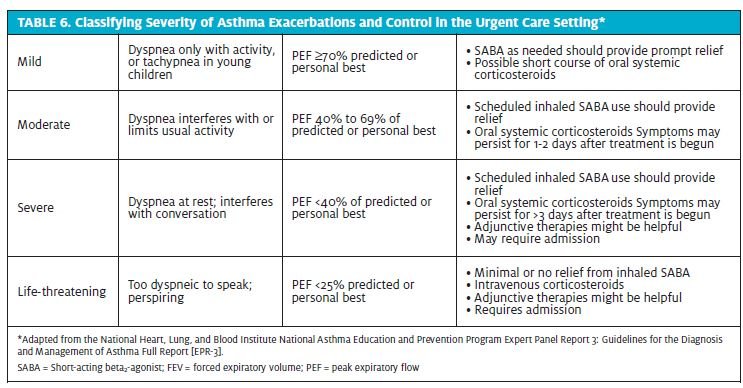
A differential diagnosis should be established (Table 3), with additional laboratory testing in to rule out other possible etiologies. Once a suspected diagnosis of asthma exacerbation has been established, information obtained from the diagnostic evaluation should be used to characterize a patient’s asthma severity and control in order to guide decisions for therapy (Tables 4 and 5).11-13 For clinical management, the emphasis should be on assessing asthma severity for initiating therapy and assessing control for monitoring and adjusting therapy.1 Asthma severity is defined by the EPR-3 as the intrinsic intensity of the disease process,1 or the difficulty in controlling asthma with the patient’s current treatment.3 Severity is most easily measured in a patient not receiving long term-control therapy,1 and should be evaluated after exclusion of modifiable factors such as poor adherence, smoking, and comorbidities. Severity largely reflects the required level of treatment and the activity of the underlying disease state during initial treatment.3 During a patient’s initial presentation, if he or she is not currently taking long-term control medication, asthma severity is assessed to guide clinical decisions on the appropriate medication and other therapeutic interventions.1 Asthma control is defined by the EPR-3 as the degree to which the manifestations of asthma (symptoms, functional impairments, and risks of untoward events) are minimized and the goals of therapy are met.1 Asthma control not only encompasses a patient’s current clinical state, but also considers future risk. If a patient has a documented established diagnosis, the emphasis for clinical management should be on assessment of asthma severity and control. The level of asthma control will guide decisions to either maintain or adjust therapy.1 Asthma severity and control should be based on both the patient’s impairment over the last 2 to 4 weeks and the most severe impairment or risk category. In patients aged 5 years and older, spirometry or peak flow measurements should also be used to assess asthma control. Table 6 outlines an example of how asthma severity and control might be assessed in the urgent care setting based on the EPR-3 guidelines.
Conclusion
The increase in prevalence of asthma with increasing presentations to ambulatory care settings presents unique opportunities in short and long-term management for the urgent care provider. An appreciation of the fundamental pathogenesis of airway inflammation in asthma and the variable, interactive expressions of airway hyperesponsiveness and airway obstruction will give an urgent care provider a better understanding of the opportunities to control the disease. Suspecting a diagnosis of “asthma exacerbation” is particularly important in the patient without a known diagnosis for proper short-term and long-term management. Knowledge of key indicators for a diagnosis of asthma on history and examination is important in further evaluating risk factors for worse outcomes in patients with asthma. Part 2 of this topic, in a subsequent issue, will review both the short- and long-term management of the disease in the urgent care setting.
References
- US Department of Health and Human Services, National Institutes of Health, National Heart Lung and Blood Institute. National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma; 2007:1-417.
- Greenberg S. Asthma exacerbations: predisposing factors and prediction rules. Curr Opin Allergy Clin Immunol. Jun 2013;13(3):225-236.
- Myers T, Tamasio L. Asthma: 2015 and Beyond. Respiratory Care. 2011; 56(9):1389-1410.
- Gold L, Yeung K, Smith N, Allen-Ramsey F, Nathan R, Sullivan S. Asthma Control, Cost, and Race: Results from a National Survey. Journal of Asthma. 2013 Sep; 50(7):783-790.
- Hing E, Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2004. Advance data from vital and health statistics; no 374. National Center for Health Statistics; 2006.
- Centers for Disease Control and Prevention. National Health Interview Survey (NHIS) 2007 data release. http://www.cdc.gov/NCHS/nhis/nhis_2007_data_release.htm.
- Centers for Disease Control and Prevention. 2007 National Health Interview Survey (NHIS) Data. Table 1-1. Lifetime asthma population estimates, in thousands, by age, United States: National Health Interview Survey; 2007.
- Centers for Disease Control and Prevention. 2007. National Health Interview Survey (NHIS) Data. Table 4-1. Current asthma prevalence percents by age. United States: National Health Interview Survey. 2007.
- Vital signs: asthma prevalence, disease characteristics, and self-management education:United States, 2001-2009.MMWR Morb Mortal Wkly Rep. 2011;60:547-552.
- Barrieiro T, Perillo I. An approach to interpreting spirometry. Am Fam Physician. 2004; 69:1107-1114.
- Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902–907.
- Vollmer WM, Markson LE, O’Connor E, Frazier EA, Berger M, Buist AS. Association of asthma control with health care utilization: a prospective evaluation. Am J Respir Crit Care Med. 2002; 165(2):195–199.
- Nathan RA, Sorkness CA, Kosinski M, et al. Development of the Asthma Control Test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65.

