Urgent message: Data show that urgent care centers are becoming a more common destination for patients experiencing chest pain. Immediate recognition of emergent vs. urgent causes may be the make-or-break moment for the patient’s outcome.
Jasmeet Singh Bhogal, MD
Introduction
Evaluation of chest pain always presents as a diagnostic challenge, be it in the outpatient family medicine setting or the hospital emergency department. In fact, urgent care centers occupy a unique position in the equation; while most urgent cares usually do not have the high-end services of an emergency department that can offer serum troponin levels, areas for monitoring of patients over a period of time, etc., they may have electrocardiograms, the ability to do basic blood work, and other services that set them apart from a typical family practice office.
Despite the availability of emergency medical services in most areas, urgent care centers are seeing more and more adult patients with chest pain.1 Many are high-acuity cases who require emergent attention, in spite of the fact that they may be in urgent care hoping to get a “quickfix” for their chest pain so they can go on with their activities without being admitted to the hospital.
Given this, it is all the more important for urgent care providers to be familiar with and to constantly re- mind themselves of the common emergent and urgent causes of chest pain. Patients need to be evaluated with the resources we have available and then triaged in a timely manner to the appropriate level of care.
This article will focus on the diagnostic evaluation of the emergent causes of chest pain, and the principles that may help in the development of chest pain protocols at the urgent care level.
Acute Coronary Syndrome
Despite considerable progress, heart disease is still the leading cause of death in the United States.2 In fact, the fear of heart attack is probably the most common reason for patients to go to a medical facility to get evaluated for chest pain.
The diagnostic approach to chest pain starts with the ba- sic history and physical examination. A retrosternal chest pain that is episodic, lasting <10 minutes and provoked by exertion usually represents typical exertional angina.3
On the other hand, a similar pain that is present at rest and not related to exertion may represent atypical angina.3 Any change in the character of an already existing pain may represent unstable angina, and may put the patient at a high risk of acute myocardial infarction (AMI) and death.3
Certain characteristics of chest pain that increase the likelihood of AMI include, in decreasing order of likeli- hood ratio: radiation to right arm or shoulder; radiation to both arms or shoulders; associated with exertion; radi- ation to left arm; associated with diaphoresis; associated with nausea or vomiting; worse than previous angina or similar to previous MI; described as pressure.4
Characteristics that decrease the likelihood of AMI include: pain described as pleuritic, positional, or sharp; pain that is reproducible with palpation; inframammary location; not associated with exertion.4
Diagnosis
It is important to note that although certain elements of the chest pain history are associated with increased or de- creased likelihoods of a diagnosis of acute coronary syndrome (ACS) or AMI, none of them alone or in combination identifies a group of patients that can be discharged safely without further diagnostic testing.4
The response to the administration of nitroglycerin is often used by physicians to differentiate whether chest pain is cardiac or non-cardiac in nature.5 However, there is evidence suggesting that neither a response nor lack of response to nitroglycerin predicts active coronary artery disease in patients presenting to an ED with chest pain (LOE=2b).5 Another consideration is the fact that certain other disorders (e.g., esophageal spasm) respond to nitroglycerin.
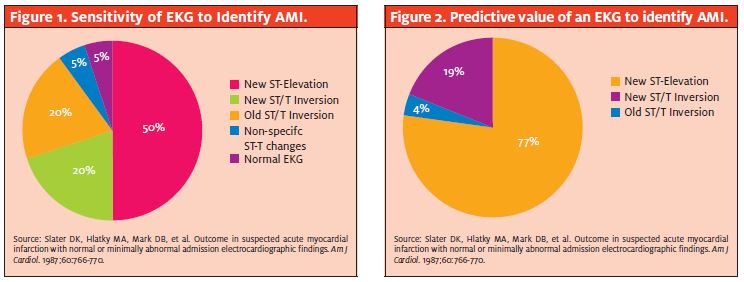
The EKG is also a very important diagnostic tool in the evaluation of chest pain. Although new abnormalities in the ST-segment and t-waves represent myocardial ischemia, the EKG may be normal or non-specific in patients with either ischemia or infarction. The sensitivity and the positive predictive value of an EKG to identify AMI are shown in the Figure 1 and Figure 2.
Many urgent care centers now incorporate the use of serum troponin level in the evaluation of chest pain. Among patients with non-ST elevation ACS, the short- term odds of death are increased three- to eightfold for those with an abnormal troponin test.6
Bedside tests for cardiac-specific troponins are highly sensitive for early detection of myocardial-cell injury in ACS. Negative tests are associated with low risk.7 Elevated levels of troponin I (i.e., >1 ng per ml, though reference ranges may vary according to the brand of reagent/testing equipment) at least six hours from presentation support the diagnosis of MI or ACS and increase the likelihood of death or recurrent MI within 30 days.8
Normal level of troponin I between six and 72 hours after the onset of chest pain is strong evidence against ACS and MI, particularly if the EKG is normal.8
Risk scores
Once that information is available, the next step is to eval- uate all these findings in order to stratify risk for the pa- tient and henceforth determine appropriate triage.
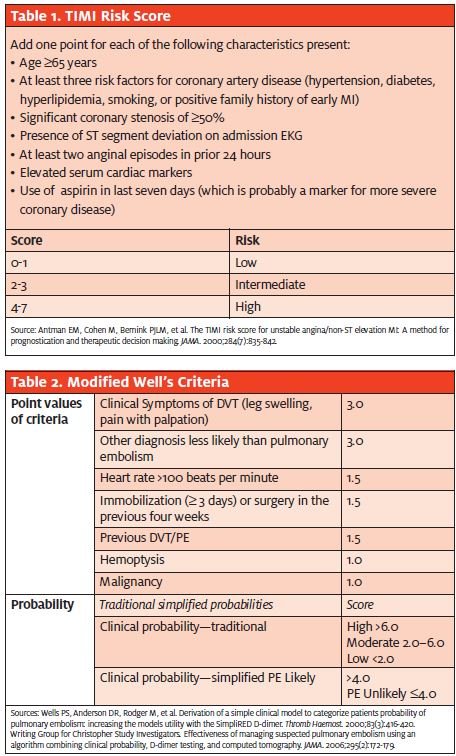
Various risk scores have been developed to facilitate this. Examples include the Agency for Healthcare Policy and Research Risk Prediction Model, Rush Risk Prediction Model, Goldman Chest Pain Protocol, and the Acute Coronary Ischemia Time-Insensitive Predictive Instru- ment. The most commonly used, however, is the TIMI Risk Score (Table 1). It uses seven variables at presenta- tion, which are independently predictive of outcome in patients with unstable angina or non ST-elevation MI (NSTEMI). A value of 1 is assigned for each factor present (0 if it is absent).
The combination of the findings on the EKG, troponin levels, and TIMI risk score can provide a very good tool for evaluation of ACS in urgent care centers. Based on this evaluation, the physician may make informed decisions on giving the patient aspirin, oxygen, and nitroglycerin.
The physician may also decide on the appropriate means of transferring the patient at this time (e.g., 911 versus regular ambulance).
Finally, this evaluation may also help the physician give the accepting ED a more detailed summary and help expedite further management of the patient once he or she is in the ED.
Aortic Dissection
Data defining the incidence of aortic dissection are limited. Estimates range from 2.6 to 3.6 per 100,000 person- years.9 Although not very common, it is a catastrophic illness, typically presenting in the elder population (usually >60 years old), with males being affected more than females (two thirds of patients are male).10
Chest pain is typically the most common presenting symptom. It is described as sharp, or tearing (approximately 50% of patients) in character. It may be located in the posterior chest or back if the dissection is distal to the left subclavian artery, or it may be anterior chest pain if the dissection is in the ascending aorta.
Syncope is another important symptom of aortic dis- section that may be present in 10% to 12% of patients.11 Patients may often present with an initial syncopal episode, followed by regaining of consciousness, and complain of severe abdominal or back pain. Syncope is associated with a worse prognosis.11
Chest pain as a symptom is more common in patients with dissections of the ascending aorta, while back and abdominal pain is common in all other dissections.10 Aortic dissection can also be painless, but this is relatively uncommon.
Physical examination may reveal a pulse deficit in the carotid, brachial, or femoral pulse. A variation of >20mm Hg in the systolic blood pressures of both arms may be associated with dissection of the ascending aorta. The patient may also show signs of hypotension or shock.
The most important predisposing factor in the elderly that may be evident on further evaluation is the presence of systemic hypertension (72% of patients). Ath- erosclerosis is another risk factor, present in approximately 31% of patients.10
Specific risk factors that may predispose younger people to aortic dissection include: pre-existing aortic aneurysm, inflammatory diseases causing vasculitis (e.g., giant cell arteritis, Takayasu’s arteritis, rheumatoid arthritis, syphilitic aortitis), disorders of collagen (e.g., Marfan’s syndrome, Ehlers-Dan- los syndrome, annuloaortic ectasia), a positive family history, bicuspid aortic valve, aortic coarctation, and Turner syndrome. Other predisposing factors include previous aortic valve replacement, cardiac catheterization, use of crack cocaine, and high-intensity strenuous resistance training. Coronary artery bypass graft and trauma are rare causes of aortic dissection.
Diagnosis
The diagnosis of aortic dissection is usually made on the basis of history and physical exam findings, especially in an urgent care center.
EKG usually adds little to the evaluation, though it may be used to differentiate from a myocardial infarction. In aortic dissection, the EKG may be normal, show non-specific ST-T changes (LVH associated with hypertension), or show ischemic or acute MI in a minority of patients.10
Routine blood work is non-diagnostic in aortic dissection.
The following is a useful tool that can be used as a clinical model for predicting acute aortic dissection:12
- Abrupt onset of thoracic or abdominal pain with a sharp, tearing and/or ripping character
- Mediastinal and/or aortic widening on chest radiograph
- A variation in pulse (absence of a proximal extremity or carotid pulse) and/or blood pressure (>20 mm Hg difference between the right and left arm). Incidence of dissection varies according to the combination of these factors present in a given patient. If all three are absent, incidence has been found to be 7%; if just pain is present, 31%; just chest x-ray abnormalities, 39%; variation in pulse or blood pressure differential, 83%. Incidence if any two out of the three are present is also 83%.
In practice, there may be not enough time for the patient to even undergo a chest x-ray or other diagnostic studies if there are signs of hemodynamic instability or if the suspicion of an aortic dissection is high based on the history and examination findings. Management of airway, breathing, and circulation (ABCs) may take precedence over any further diagnostic evaluation, and the patient will need to be transferred to the ED or the ICU (based on availability) using means such as 911.
It is advisable to have a high index of suspicion for an aortic dissection in patients with chest pain, as these patients may become unstable very quickly and may need interventions such as intubation and ventilation.
Pulmonary Embolism
Pulmonary embolism (PE) is and has always been one of the most challenging diagnoses to make, no matter what the setting. Urgent care centers are no exception to this.
PE is a common cause of chest pain and can be fatal if not treated promptly. EKG and chest x-ray can aid in the diagnosis of acute PE. However, most urgent care centers do not have access to ultrasound, V/Q scan or
CT-angiography; these are required to confirm the diagnosis of PE.
Diagnosis
Factors that make diagnosing PE difficult in the urgent care setting include:
- non-specific The symptoms and signs may mimic other disorders. There is no specific pat- tern with which a patient presents.
- non-specific routine lab findings, including pulse oximetry, WBC, ESR, arterial blood gas, BNP, and troponin. Serum troponin elevations may be useful to determine prognosis, as they are associated with adverse 13
Given the non-specific symptoms and signs that a patient with PE can present with, physicians should rely on pretest clinical probability criteria and, if necessary, pursue tests like EKG and chest x-ray in a more focused fashion. This is important to note, as even the chest x-ray and EKG do not have specific diagnostic findings that confirm acute PE.
The most commonly used scoring system is Well’s criteria. The interpretation of the score can be done using either the original Well’s criteria or the modified Well’s criteria (Table 2). Each can be helpful in deciding the course of action for patients with suspected PE.
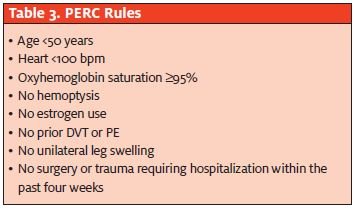
The PERC (PE Rule-out Criteria) (Table 3) is also useful in ruling out PE in patient populations presumed to have a low-risk of PE. When combined with Well’s criteria, the PERC has a high sensitivity and negative predictive value.14 It can essentially exclude acute PE and prevent further testing if all the criteria in the PERC rule are met, along with a low probability on the Well’s criteria.14 The PERC criteria, how- ever, has a low specificity and positive predictive value.14
Once it is decided that further investigation needs to be done, physicians may decide on which tests to perform based on the condition of the patient and the avail- ability of the test.
The classic EKG findings of S1Q3T3, right ventricular strain, and new incomplete right bundle branch block are seen in patients with massive acute PE and cor pulmonale.15-17 Findings associated with poor prognosis include:15-17
- atrial arrhythmias
- right bundle branch block
- inferior Q-waves
- precordial T- wave inversion and ST-segment
Although certain chest x-ray findings are common in PE, they are not diagnostic.18,19 Such findings include at- electasis, parenchymal abnormality, and pleural effusion. Published reports of the proportion of patients with PE who have normal x-rays range from 12% to 24%.18-20 The D-dimer is another test that may help in excluding PE but has little value in diagnosing PE. In patients with low or moderate pretest probability of PE, a D- dimer level <500 ng/ml by quantitative ELISA or semiquantitative latex agglutination excludes PE.21
The usefulness of this test depends on the pretest prob- ability and the type of assay performed.21 It should not be used to exclude PE in patient with high clinical prob- ability.21
The diagnostic test of choice for diagnosing PE is pulmonary angiography. Where available, a CT-chest may be performed to confirm the diagnosis of PE. If not available, then a V/Q scan or lower extremity venous ultrasound may be performed, again based on availability. If neither of these tests is available, then the patient may need transfer to a facility where the tests are available and the patient can be treated appropriately. The patient may also need transfer if the V/Q scan or lower extremity venous ultrasound is inconclusive, but the suspicion for PE is high.
Pericardial Tamponade
Based on the etiology, pericardial tamponade can present in the form of a patient with mild symptoms with no hemodynamic com- promise, to a patient in severe distress and hemodynamic instability, requiring resuscitation measures. The presentation may vary from that of chest pain, to signs of overt cardiogenic shock like peripheral cyanosis and cool extremities. Clinical features at presentation may vary based on the acuteness of symptoms (Table 4).
Physical examination findings that may be found in any of these types of tamponade include: sinus tachycardia, elevated jugular venous pressure, pulsus paradoxus, pericardial rub, and Kussmaul’s sign (usually associated with constriction).
EKG may reveal a sinus tachycardia and low voltage. A maximum QRS amplitude of <0.5mV in the limb leads may be a specific finding of pericardial tamponade.22A chest x-ray may show enlarged cadiac silhouette if 200 ml of fluid has accumulated in the pericardial space.23 The patient may need further investigation such as an ECHO and CT chest, which may be beyond the scope of urgent care.
Almost all patients with a suspected tamponade will need transfer to the ED or the ICU in consultation with the ED physician or the cardiologist, as available. Patients in hemodynamic compromise may need emergent attention to the ABCs along with expedited transfer to the ED. Again, it is important to keep a high index of suspicion for tamponade in patients presenting with the signs and symptoms as described above.
Tension Pneumothorax
While presentation to the urgent care center may be rarer than in the ED, the urgent care clinician should nonetheless be prepared for pa- tients presenting with chest pain and severe distress that may ulti- mately be indicative of tension pneumothorax.
A history of blunt chest injury or a small penetrating wound may be elicited. Patients usually are in respiratory distress. Physical exam findings may reveal tachypnea, hypoxia, hyperresonance to percus- sion, and decreased or absent breath sounds on the affected side.
The crucial factor to bear in mind while evaluating such patients is that the diagnosis of tension pneumothorax is clinical; once confirmed based on the history and physical exam, immediate treatment with- out waiting for the chest x-ray is necessary if the patient is unstable. For a stable patient, diagnosis is confirmed using chest x-ray. It should be noted that tension pneumothorax is almost always unstable, and diagnosis should be made long before an x-ray is taken.
Tension pneumothorax may be one of the rare occurrences in which emergent intervention is needed in the urgent care center (as opposed to waiting for emergency transfer to a higher acuity facility). In such a case, a nee- dle thoracostomy may be the only available option. This involves putting a large bore (16 gauge) needle in the second intercostal space in the midclavicular line in order to convert a tension pneumothorax into a simple pneumothorax. Leave the needle in place until a definite chest tube is put in.
Esophageal Rupture
Esophageal rupture is a relatively rare cause of chest pain; however, it can be fatal if missed. Again, its presentation may be somewhat less common in urgent care com- pared with the ED due to the degree of hyperemesis in- volved. In addition, causative penetrating trauma of this nature typically goes directly to the ED.
Patients with esophageal rupture present with retrosternal chest pain or upper abdominal pain, typically after an episode of severe retching and vomiting. This vomiting could be induced by caustic ingestion, alcohol ingestion, blunt or penetrating chest trauma, esophagitis secondary to pill ingestion, Barrett’s ulcer, or infectious ulcers in patients with AIDS, among other causes. Instrumentation of the esophagus can also lead to esophageal rupture.
Other findings may include odynophagia, fever, respiratory distress, cyanosis, and subcutaneous emphysema (not very sensitive).23 If transport is delayed and the patient is stable, a chest x-ray may be performed, which will reveal free air in the mediastinum or peritoneum.24 A neck film may demonstrate air in soft tissues of the prevertebral space. Patients can go into shock rapidly; therefore, while se- curing the ABCs, emergent transfer of the patient to the ED via 911 may be the only option for appropriately triaging. There may be no time to perform any x-ray studies in the urgent care center. The patient will eventually need a CT-chest and further evaluation and monitoring in the ED.
Conclusion
The challenge of assessing chest pain in the urgent care settings is often a difficult one. Relatively limited resources make the task even tougher, typically.
Initial evaluation should always include an assessment and stabilization of the airway, breathing, and circulation. Emergent causes, as described previously, should be considered first; further evaluation and management should be conducted as needed. Available resources should be used judiciously, and in a timely fashion.
It is often difficult to make people understand the se- riousness of the situation when dealing with chest pain in the urgent care center. It is important to always keep the patients informed about the reasons for various tests and the possibility that they might need to be transferred to a higher level of care if the need arises.
With more and more urgent care centers opening up, the number of patients presenting to this setting with chest pain is bound to increase. As urgent care providers, we must be well prepared to evaluate and provide these patients with timely and appropriate care.
REFERENCES
- Carrigan T, Weingart J, Resnick L, et The role of ambulatory urgent care centers in regional acute coronary syndrome care. Harrington and McLaughlin Heart and Vascular Institute University Hospitals Case Medical Center, Cleveland OH. 2009.
- Heron M, Hoyert D, Murphy S, et Deaths: Final data for 2006. National Vital Statistics Reports. 2009;57:14.
- Acute coronary syndromes: Acute myocardial infarction and unstable In: Tint nalli J, ed. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 6thedition. New York, NY: McGraw-Hill Professional; 2005.
- Swap C, Nagurney Value and limitation of chest pain history in the evaluation of patients with suspected ACS. JAMA. 2005;294(20):2623-2629.
- Henrikson CA, Howell EE, Bush DE, et Chest pain relief by NTG does not predict active CAD. Ann Intern Med. 2003;139(12):979-986.
- Heidenreich P, Alloggiamento T, Melsop K, et The prognostic value of troponin in pa- tients with non-ST elevation ACS: A meta-analysis. J Am Coll Cardiol. 2001;38(2):478-448.
- Hamm CW, Goldmann BU, Heeschen C, et Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med. 1997;337(23):1648-1653.
- Cayley Diagnosing the cause of chest pain. Am Fam Physician. 2005;72(10):2012-2021.
- Meszaros I, Morocz J, Szlavi J, et Epidemiology and clinicopathology of aortic dissection: A population based longitudinal study over 27 years. Chest. 2000;117(5): 1271-1278.
- Hagan PG, Nienaber The International Registry of Acute Aortic Dissection (IRAD): New insights into an old disease. JAMA. 2000;283(7):897-903.
- Nallamothu BK, Mehta RH, Saint S, et Syncope in acute aortic dissection: Diagnostic, prognostic and clinical implications. Am J Med. 2002(6);113:468-471.
- Von Kodolitsch Y, Schwartz AG, Nienaber Clinical prediction of acute aortic dissec- tion. Arch Intern Med. 2000;160(19):2977-2982.
- Becattini C, Vedovati MC, Agnelli Prognostic value of troponins in acute pulmonary embolism: A meta-analysis. Circulation. 2007;116(4):427-433.
- Wolf SJ, McCubbin TR, Nordenholz KE, et Assessment of the pulmonary embolism rule-out criteria rule of suspected pulmonary embolism in the emergency. Am J Emerg Med. 2008;26(2):181-185.
- Thames MD, Alpert JS, Dalen The electrocardiographic manifestations of pulmonary embolism. JAMA. 1977;238(23):2509-2511.
- Geibel A, Zehender M, Kasper W, et Prognostic value of the ECG on admission in pa- tients with acute major pulmonary embolism. Eur Respir J. 2005;25(5):843-848.
- Ferrari E, Imbert A, Chevalier T, et The ECG in pulmonary embolism. Predictive value of negative T waves in precordial leads—80 case reports. Chest. 1997;111(3):537-543.
- Stein PD, Terrin ML, Hales CA, et Clinical, laboratory, roentgenographic findings in pa- tients with acute pulmonary embolism and no pre-existing cardiac or pulmonary disease. Chest. 1991;100(3):598-603.
- Stein PD, Saltzman HA, Weg Clinical characteristics of patients with acute pulmonary embolism, Am J Cardiol. 1991;86(17):1723-1724.
- Elliott CG, Goldhaber SZ, Visani L, et Chest radiographs in acute pulmonary embolism. Results from the International Cooperative Pulmonary Embolism Registry. Chest. 2000;118(1):33-38.
- Adapted from Thompson BT, Hayles Diagnosis of acute pulmonary embolism. Up- toDate. September 2010. Available at: http://www.uptodate.com/home/content/ topic.do?top- icKey=ven_pulm/6608.
- Bruch C, Schmermund A, Dagres N, et Changes in QRS voltage in cardiac tampon- ade and pericardial effusion: reversibility after pericardiocentesis and after anti-inflamma- tory drug treatment. J Am Coll Cardiol. 2001;38(1):219-226.
- Spodick Acute cardiac tamponade. New Engl J Medicine. 2003;349(7):684-690.
- Pate JW, Walker WA, Cole FH Jr, et Spontaneous rupture of esophagus: A 30 year experience. Ann Thorac Surg. 1989;47(5):689-692.