Urgent message: Injection/aspiration therapy for selected musculoskeletal complaints is becoming more common in urgent care practice. Providers need a thorough understanding of injection/aspiration procedures and associated risks to be equipped to deliver rescue therapy to patients.
THOMAS V. GOCKE, III, MS, ATC, PA-C, DFAAPA
Joint pain, joint effusion, and recurrent soft-tissue trigger point irritation are common presentations in urgent care. As more and more patients present seeking immediate relief of such symptoms, it’s important that urgent care providers know how to perform injections into soft tissue. Although the skills required are not demanding, introducing needles into joint spaces can be painful and a thorough understanding of the pertinent musculoskeletal anatomy is necessary.
This article provides an overview of the inflammatory response, use of corticosteroids and anesthetic agents, pre- and post-injection/aspiration considerations, and the approach to injections for subacromial impingement syndrome. Part 2 of this series, in a future issue, will review approaches to lateral epicondylitis, olecranon and prepatellar bursitis, ganglion cyst, trochanteric bursitis knee injection and aspiration, and evaluation of joint infection.
The objective of this series is to focus on common musculoskeletal conditions for which urgent care providers might consider injection or aspiration. The list of conditions presented is not exhaustive but it highlights common presenting symptoms and successful approaches for injection or aspiration in frequently encountered clinical scenarios. Keep in mind that any injection or aspiration procedure should be performed using sterile technique.
The Inflammatory Response
An acute inflammatory response occurs when bodily injury triggers a non-specific immune response that causes proliferation of leukocytes and increase in blood flow secondary to trauma. The increased blood flow brings polymorphonuclear leukocytes (which facilitate removal of the injured cells/tissues), macrophages, and plasma proteins to the injured tissues. As a result of this process, redness occurs at the injury site, tissue warmth occurs as result of increased cellular activity, swelling results from increased fluid, and pain ensues from tissue injury and stretching of nerve structures. The accumulation of fluid/edema at the injury site can limit the healing process by reducing joint range of motion (ROM), thus facilitating the formation of scar tissue. Therefore, limiting bleeding/edema at an injury site and initiating ROM activities when appropriate (non-fracture trauma) is important to the tissue healing process. Corticosteroids limit release of leukocytes, macrophages, and vasoactive substances, and the formation of prostaglandins that contribute to the inflammatory process.1
Corticosteroids
Performing an injection is a simple procedure with few complications. Selection of the injection site is important, taking into consideration skin integrity, potential for infection, underlying medical conditions and intended use of the steroid injection. Having a good understanding of the musculoskeletal anatomy, nerve and vascular anatomy in a particular joint or musculoskeletal region is important to avoid unintended injection or post-procedure complications. As with any procedure, corticosteroid injections, regardless of location, should be performed under sterile technique.
A thorough understanding of surface anatomy usually is enough to adequately deliver a steroid injection into a joint or soft tissue structure. Some providers may elect to use ultrasound to confirm needle placement in the intended joint space or soft-tissue structure, which requires additional training. Whether steroid injections are guided by anatomic landmarks or ultrasound, their number should be limited to reduce risk of premature destruction of joint articular cartilage or tendon rupture associated with repeat injection.2-5
No more than one injection every 3 to 4 months is a sound rule of thumb, taking into consideration the patient’s age, level of arthritic changes, comorbidities, and eligibility for other therapies. In rare cases, patients can be given steroid injections more frequently than 3 to 4 times per year.2-5 Many corticosteroids are available for injection and the simplest way to choose is based on desired speed of onset and duration of action (Table 1). Like anesthetic agents, corticosteroids have short-onset/short-duration and long-onset/long-duration components. Longer-onset/longer-duration steroids take effect in 2 to 3 days and their effects may last for several weeks to months or completely resolve a patient’s problem. However, relief of pain and inflammation is not always predictable. Some patients will respond, others will not, and the occasional patient will have a reaction to the steroid itself. Such a “flare reaction” may cause increased local redness and rather severe pain for 12 to 24 hours and can happen for several reasons. One is local injury secondary to the needle stick that triggers a local inflammatory response. The steroid crystallizes and deposits into the soft tissues or synovial lining, resulting in a secondary synovitis in a joint with pain and swelling.
A corticosteroid’s solubility also has an impact on likelihood of flare reaction. The more soluble a steroid (Betamethasone acetate®) the shorter the duration (faster onset) and thus, the lower the risk of flare reaction. The less soluble a steroid (methylprednisolone acetate injectable suspension) the longer the onset and duration but the higher the risks of flare reaction. It should be noted that in a 2009 study, Seshadri et al reported that lidocaine 1% combined with methylprednisolone had a toxic effect on joint chondrocytes in an in vitro model.6 When selecting a steroid agent for injection, the goal is to maximize anti-inflammatory effects and minimize adverse effects.2-5
Anesthetic Agents
Before selecting an agent for soft-tissue injection, urgent care providers should be meticulous about reviewing and documenting a patient’s allergy history. Occasionally, for example, patients report that they cannot have lidocaine because of an allergy to dental Novocain. In some cases, the allergy may be to the preservative in the solution rather than to a medication itself. In susceptible individuals, metabisulfite, a sulfite that acts as a preservative, can cause allergic-type reactions ranging from asthmatic episodes to life-threatening anaphylaxis. The overall prevalence of such sensitivity in the general population is unknown but probably low. It is more common in asthmatics than in those who do not have asthma. Mixing epinephrine with an anesthetic agent is not recommended, particularly for joint injections, because in the intra-articular space, it can lead to constriction of the synovial lining, resulting in increased pain.
An anesthetic agent’s effectiveness also is a consideration when performing soft-tissue vs. intra-articular injections. For soft-tissue injections, a shorter-onset anesthetic agent may give more immediate pain relief but the duration of pain relief will be shorter. Likewise, a longer-onset anesthetic agent will take longer to provide pain relief but it usually will last for a longer period of time. Regardless of which anesthetic agent you select, being aware of its indications, contraindications, and adverse effects—and particularly its toxic range—is important. Keep in mind that while the toxic dose is calculated based on weight, factors such as age, medical conditions, and overall nutritional status should be taken into consideration when choosing an anesthetic and determining the amount of solution to inject. Patients with hepatic or cardiovascular disease warrant special attention when administering lidocaine injections. Lidocaine is metabolized via the liver and any impairment could lead to toxic adverse effects. Patients with cardiovascular disease may not be able to accommodate the prolongation of A-V conduction associated with use of the drug.
Selection of anesthetic injectable solutions varies widely among urgent care providers (Table 2). High concentrations of bupivacaine have been proven to result in degenerative changes to the articular cartilage with prolonged infiltration of joint structures.7-10 Therefore, use of lower concentrations of bupivacaine 0.125% or 0.25% are recommended for repetitive intra-articular injections. Lower concentrations of bupivacaine 0.25% or 0.125% are beneficial for repetitive intra-articular injections. A similar issue exists regarding use of lidocaine for intra-articular injection. In a study by Dragoo et al in 2012, lidocaine 1% was found to have toxic effects on joint chondrocytes in an in vitro model. Commenting on their in vitro model of lidocaine 1% combined with methylprednisolone, however, Seshadri and colleagues nevertheless noted that “physicians (surgeons) have been injecting patients’ joint with these agents for years without any significant adverse effects in human subjects.”2-16
Particular attention should be paid to maximal toxic dosing of bupivacaine and lidocaine in patients who are elderly or patients with medical complications that put them at risk for adverse effects with administration of these medications.
Pre- and Post-Injection/Aspiration Considerations
Before administering an aspiration or injection, as with any procedure, it is important to perform a thorough physical and history. Assessment of involved musculoskeletal structures to determine the extent of musculoskeletal injury is important and can be done with radiographs, and in some cases, magnetic resonance imaging. A patient’s symptoms may range from dull persistent aches to pain with range of motion, to discomfort with resistive motion to pain that is constant and unaffected by motion or rest. Patients with acute injuries will generally experience more severe pain while those with repetitive use or chronic injuries will report a persistent dull achy quality to their pain. For example, some patients with rotator cuff tendinitis may experience some pain with certain ROM but others may experience only general soreness with activity but no pain at rest. Patients who have a tear in the rotator cuff tendon may have acute pain that is present regardless of their activity or shoulder motion. Keep in mind that not all patients experience pain in the same way. A thorough understanding of a patient’s activities can help to localize the structures that are either acutely or chronically inflamed. In cases when conservative measures fail, intra-articular corticosteroid or local trigger point injection may provide symptom relief.2,3,11,17-31
Needle selection. Needle selection should be based on the intended injection surface/site. Intra-articular injections, for example, require a 1 ½- to 2-inch hypodermic needle to penetrate the skin structure in order to enter the joint space. In a patient who has larger surface area and body girth, a spinal needle and/or injection under ultrasound or fluoroscopic guidance may be needed to ensure that the needle is introduced into the intra-articular space. For trigger-point injections, a shorter hypodermic needle should be used. For a para-scapular trigger-point injection, for example, use of a 2-inch needle would risk piercing the pleura, resulting in pneumothorax. For knee and shoulder injections, a 21-gauge or 22-gauge 1 ½-inch hypodermic needle is preferable. For injection of smaller joints such as the AC joint or trigger point injections (epicondyle), a 25-gauge or 26-gauge 1/2–inch hypodermic needle can be used. For an aspiration, the needle gauge should be of sufficient size to allow fluid to be aspirated out of the joint, ganglion or bursae; a 16-gauge or 18-gauge 1 ½-inch hypodermic needle can be used. A 22-gauge spinal needle is preferable for trochanteric bursitis injections and can be used to reliably penetrate to the depth necessary to deliver an injection to the bursae region.2,11,15
Skin preparation. A variety of solutions are available that can create a sterile skin field in preparation for any procedure. Because introducing a needle into a sterile joint has the potential to cause an infection, as a general rule, joint injection/aspiration and trigger point injections should be performed under sterile technique. That means prepping the skin with an antiseptic solution and using sterile gloves to palpate the injection site while delivering the injection.
Povidone-iodine (or its equivalent) is the default for skin prep prior to injection but chlorhexidine can be used for patients who are allergic to povidone-iodine. Before the prep, the location of the injection entry point should marked on the patient’s skin using the hollow end of a pen, skin marking pens, or the capped end of the needle. The mark helps the clinician guide the needle into its intended location. Once the marking is completed, the patient’s skin should be prepped. Starting at the marked injection point and going out 3 cm all around it, povidone-iodine sticks or sterile gauze pads soaked in chlorhexidine can be painted on the skin in a circular motion three times. Next, put on sterile gloves and palpate the injection entry point again to confirm that the entry point mark is in the correct position. Just prior to the injection, have an assistant use cold spray to deaden the skin.
With a sterile gloved hand, confirm the entry point again and then introduce the needle into the intended injection site. Deliver the solution with a steady even flow until the solution is completely deposited. Afterwards, withdraw the needle and clean the skin with alcohol to remove the povidone-iodine (or chlorhexidine) and apply an adhesive bandage to minimize bleeding. For patients who are on aspirin or anticoagulant medication, a compression bandage should be used to minimize bleeding at the injection site.
Discharge Instructions. A discharge instruction sheet should be provided and reviewed with the patient who has undergone a joint aspiration or intra-articular/trigger point corticosteroid injection (Table 3). It should outline the intended effects of the injection and potential adverse effects, and provide instructions for pain management and a call-back phone number to answer marks. Less skilled urgent care providers will deliver a sub-muscular injection if they fail to enter the subacromial space. The anterior approach is used less often and is recommended only for skilled practitioners.2,3,17, 23, 32,33
| Table 3. Discharge Instruction Example |
| Corticosteroids are a class of medications related to cortisone – a steroid. Medications in this class of anti-inflammatory drugs are powerful and can reduce inflammation quickly. Corticosteroids are not pain medications but when they reduce inflammation, they can have a direct impact on pain relief. While the inflammation for which corticosteroids are given can recur, in most cases, patients experience relief of their symptoms for many months and possibly for years. Steroid injections are intended to relieve inflammation from conditions such as tendonitis, bursitis, arthritis, and painful spinal cord/nerve root conditions. Steroid injections should be limited to three to four times per year because of the potentially harmful changes seen in tissue/joint structures in patients who receive too many steroid injections. Side Effects
Instructions
|

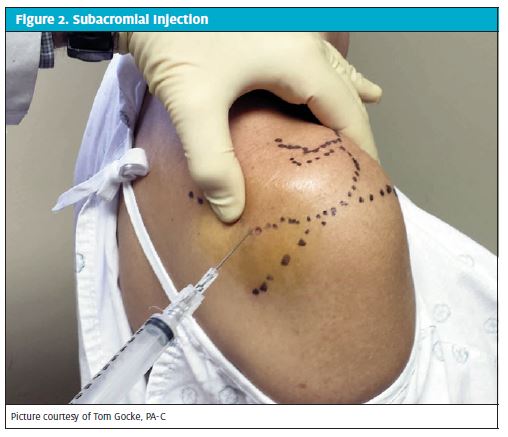
The best patient position for a shoulder injection is with the patient seated and regardless of the approach, the appropriate body landmarks should be identified prior to injection to ensure that the injection is delivered into the subacromial space appropriately (Figure 2). Mark the posterior injection site and then prep the skin with antiseptic solution. As a guide for injection, place your index finger on the coracoid process and your thumb adjacent to the injection portal. When the needle is introduced into the subacromial space, follow the path toward the coracoid process and angle slightly cephalad to slide beneath the acromial spine. Once the needle enters the subacromial space, there is little resistance when the cortisone–anesthetic solution is injected. Most patients report no pain associated with the procedure.
Patients should be advised to take it easy for 24 hours after a subacromial injection to allow the medication to have its intended affect in reducing inflammation and to reduce the risk of post injection pain. Slings should not be used after injection because prolonged immobilization can reduce motion and promote stiffness rather than encouraging use of the shoulder. If patients are not discharged with ice on the shoulder, they should be instructed to apply it as soon as they are able. Cryotherapy has proven to help reduce post-injection soreness and pain.1-5, 11 Patients should be instructed to apply ice to the injection site for 20 to 30 minutes two or three times the day of injection, at 1- to 2-hour intervals.
References
- Knight KL, Pain and Pain relief during Cryotherapy: Cryotherapy: Theory, Technique and Physiology, 1st edition, Chattanooga Corporation, Chattanooga, TN 1985, p 127-137
- Diagnostic & Therapeutic Injections of the Shoulder Region. http://www.aafpa.org/afp/2003/0315/p1271.html
- Gocke TV. Common Injections & Joint Aspirations for MSK Injuries Orthopaedic Educational Services, Inc. 2013. http://www.orthoedu.com
- McNabb JW. A Practical Guide to Joint & Soft Tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010, p 3-5
- McNabb JW, A Practical Guide to Joint & Soft Tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010, p 8-11
- Seshadri V, Coyle CH, Chu CR. Lidocaine potentiates the chondrotoxicity of methylprednisolone. Arthroscopy. 2009;25(4):337-347.
- Hansen BP, Beck CL, Beck EP, Townsley RW. Postarthroscopic glenohumeral chondrolysis. Am J Sports Med. 2007;35:1628-1634.
- Busfield BT, Lee GH, Carrillo M, Ortega R, Kharrazi FD. Subacromial pain pump use with arthroscopic shoulder surgery: A short-term prospective study of complications in 583 patients. J Shoulder Elbow Surg. 2008;17:860-862.
- Busfield BT, Romero DM. Pain pump use after shoulder arthroscopy as a cause of glenohumeral chondrolysis. Arthroscopy. 2009;25:647-652.
- Life in the Fast Lane. http://lifeinthefastlane.com/education/procedures/localanaesthetic
- Mercier L, Injection & Aspiration Therapy. In: Practical Orthopaedics 4th edition. Mosby, St Louis: 1995, p 453-457
- Xylocaine Warning. The RxList, http://www.rxlist.com
- Lidocaine Injection. The MedicineNet.com. http://www.medicinenet.com
- Achar S, Kundu S. Principles of Office Anesthesia Part I: Infiltrative Anesthesia. Am Fam Phys. 2002;66(1: 91-95.
- Achar S, Kundu S. Principles of Office Anesthesia Part II: Topical Anesthesia. Am Fam Physician. 2002;66(1): 99-102.
- Dragoo JL,Braun HJ, Kim HJ,Phan HD, Golish SR. The in vitro chondrotoxicity of single-dose local anesthetics. Am J Sports Med. 2012;40(4): 794-799.
- Mercier L. Shoulder: Practical Orthopaedics 4th edition. Mosby, St Louis:1995, p 54-85
- Mercier L. Elbow: Practical Orthopaedics 4th edition. Mosby, St Louis:1995, p 86-89
- Mercier L. Forearm, Wrist, Hand: Practical Orthopaedics 4th edition. Mosby, St Louis:1995, p 98-104
- Mercier L. Hip: Practical Orthopaedics 4th edition. Mosby, St Louis:1995, p 183-184, 198
- Mercier L. Knee: Practical Orthopaedics 4th edition. Mosby, St Louis:1995, p 207-225
- Hunter DM. Shoulder pain in, Tintinalli, Ruiz, Krome: Emergency Medicine: A Comprehensive Study Guide, 4th edition. McGraw-Hill:1995, p1286-1293, 1298
- Rothaemel BJ. Shoulder Subacromial Injections. www.emedicine.medscapr.com/article/1592584-overview
- Lateral Epicondylitis Injection. www.emedicine.medscape.com/article/103440-overview
- Best Treatment for Lateral Epicondylitis Remains a Matter of Debate. www.aaos,org/news/aaosnow/dec12/clinical2.asp
- Scher DL. Lateral Epicondylitis. Orthopaedics. 2009;32(4)
- Griffin LY. Trochanteric Bursitis: Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons:2005, p 461-466
- Griffin LY. Procedure-Knee Aspiration/Injection: Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons:2005, p 571-573
- Griffin LY. Procedure-Dorsal Wrist Ganglion Aspiration: Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons:2005, p 367
- Griffin LY. Procedure-Olecranon Bursa Aspiration: Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons:2005, p 272-273
- Griffin LY. Procedure-Tennis Elbow Injection: Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons:2005, p 267-268
- University of Virginia and University of Maryland Emergency Medicine HotSpot. http://dailyem.wordpress.com/2012/11/13/quick-er-math-max-dose-lidocaine-forlocal-anesthesia.
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010, P40-45

