Urgent message: Investing time in designing repeatable processes and documentation can pay off in a more efficient, effective, and scalable urgent care operation.
ALAN A. AYERS, MBA, MAcc Practice Velocity
Introduction
Despite management’s best intentions to deliver extraordinary patient experiences, many times employees just don’t know what to do. Front-line staff members are often conflicted between “doing what’s right” for the business, avoiding management scrutiny, exerting extra unrewarded effort, and “doing what’s right” for the patient.
Ultimately, employees should act in ways that exemplify the center’s “brand promise” what identifies the center in the minds of consumers, distinguishes it from competitors, and constitutes the reason patients choose the center over other options. For successful urgent care centers, the “brand promise” typically focuses on delivering an outstanding patient experience.
But lack of employee direction leads to inconsistency in service delivery among patient encounters, between center locations, in quality of care, and in medical outcomes which necessarily undermines the brand. Employees should never be left guessing what to do, which is why successful urgent care centers implement documented, measurable, improvable processes supported by technology.
What Is a Repeatable Process?
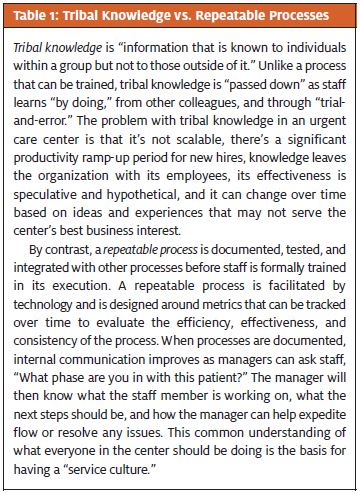
Because many urgent care centers have not documented their operational processes, employees spend time recreating processes every time they’re carried out. Staff may be intent on satisfying patients, but they perform their jobs on-the-fly and the processes they follow may vary significantly in terms of order, attention to detail, and quality. While a majority of patients may experience the “brand promise,” there will be significant variation between those who are highly satisfied and highly dissatisfied with the service received. Consider the differences between “tribal knowledge” and “repeatable processes” in Table 1.
A “repeatable process” refers to performing a task numerous times with a certain level of predictability in terms of the quality of the output. For example, when registering a patient, certain steps should occur, such as scanning identification cards, verifying the patient’s correct address and phone number, ensuring that insurance coverage is valid, and collecting co-pays, deductibles, and prior balances. If a front-office assistant fails to follow these steps consistently, the center will see increases in rejected claims, patient receivables, returned mail, and operating losses.
The major processes in an urgent care center should be documented and from those processes, policies and instructions created for employees to carry out their responsibilities. Once standardized, a process can be measured, which allows monitoring and facilitates improvements over time every position in the center. In football, the coach’s playbook contains descriptions and diagrams of plays that the team has practiced and is capable of executing in a game. More succinct, a playbook is a collection of tactics and methods that have been tested and tried. In an urgent care center, an operational playbook includes roles and responsibilities, policies and procedures, workflows, checklists, templates, forms, and various other job aids. It’s difficult to come up with the ideal repeatable process unless you fully grasp how the center is functioning today. The development of a playbook starts with documenting all the processes and procedures currently used in the urgent care center. As illustrated in Figure 1, simple flow diagrams can be used to understand every process in the center. Involve front-line staff, medical providers, center support functions, and senior management in process documentation via brainstorming sessions, individual interviews, and direct observation. Engaging everyone in the center can provide a 360- degree view as to how things are working, bottlenecks and pain points, and opportunities for improvement.
After the process is understood, the next step is to identify measures around the processes. Measures related to time, quantity, errors, cost, supplies, resource count, and profit should be tied to the performance of a specific process, such that the process can be monitored over time. Monitoring should be detailed to the level of a center, position, or employee. For example, when looking at the accuracy of front-office data entry, the number of “zero EOBs” is a good metric, but the ability to tie an EOB to a specific event and then aggregate those events to demonstrate trends will demonstrate where the process is and is not being followed. Corrective action can thus follow.
Continual Improvement
Even when a process is intended to be repeated without variation, that doesn’t mean the process can’t adapt and change over time. As the details of health care reform become more defined, urgent care centers can expect to see significant changes related to billing, reimbursement, technology, and patient utilization. In addition, as new competitors enter the fray, urgent care centers will be forced to examine their staffing models, marketing tactics, and product line offerings. So, to be successful over time, it’s clear that a center’s processes must be able to adapt and change.
In addition to monitoring metrics, an urgent care operator should engage key stakeholders including front-line staff, providers, center support functions, and even patients in periodically reviewing and suggesting improvements to processes. Once a detailed playbook is in place, updating processes is as easy as replacing pages in the playbook because the structure and context for the process is already in place.
Before implementing a process in a center, however, the process should be piloted. A pilot is a small-scale preliminary study conducted in order to evaluate the feasibility, efficiency, dependencies, and adverse impact of a process prior to its full implementation. Once a process has been piloted, refined, and agreed upon by the stakeholders, then the playbook can be updated and the process implemented through staff training.
Technology Integration
Technology forms the backbone of repeatable processes. Consider the use of technology to support front-end processes in another industry the airlines. Whereas all passenger transactions simple or complex were at one time handled at the ticket counter, today customers largely use self-service technologies to buy tickets online, check-in for flights using a smartphone app, and check bags using a street-side kiosk. These technologies have not only reduced the costs of operating the ticket counters, but they’ve also freed airline agents to spend more time helping those customers most “in need” with canceled flights or missed connections.
How To Develop Repeatable Processes
The urgent care operator’s goal should be a “playbook” for not only reduced the costs of operating the ticket counters, but they’ve also freed airline agents to spend more time helping those customers most “in need” with canceled flights or missed connections.
Likewise, an urgent care center should have technology that fully supports its processes. The packaged practice management and electronic medical record systems used in most urgent care centers are built around best-practice workflows, therefore, a center ideally should adapt its processes to the technology in place. As organizations grow, they acquire the means to build custom technology solutions or modify existing technology to meet their specific process needs.
Why Repeatable Processes Are Necessary for Growth
There are a number of ways that an urgent care center can grow. As patient volume increases, the center can extend its hours, expand its square footage, and hire more providers. It can also introduce new services, perhaps expanding into occupational medicine and travel health. Or, it can open additional locations to increase its presence in a community. Regardless of how it grows, an urgent care center cannot grow if its operating model is not scalable.
Scalability refers to the ability of a process or system to accommodate increased volume. Absent a focus on developing repeatable processes, organizations typically become more complex as they grow. The demands of an expanding number of products, systems, and protocols can be overwhelming to staff. As matrix layers of management become further removed from frontend delivery, ever-increasing demands of the front-line mean that productivity, quality, and the patient experience begin to suffer. Growth stalls and from a profit and loss perspective, the organization may end up worse off than if it had remained small and focused. Key to scalability is thus simplicity and flexibility—processes and systems that are easy to use and can be modified to fit an increasing number of business scenarios.
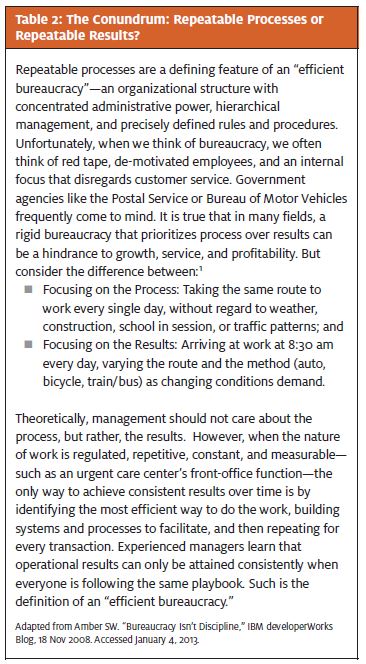
Table 2 demonstrates that when work is repetitive in nature and output is measurable, the most effective organizational structure is one built around repeatable processes.
Conclusion
The development of repeatable processes is the basis for building and running an efficient, effective and scalable urgent care operation. Achieving consistent quality results is therefore dependent on investing time in process design and documentation. Once an operational playbook is developed and processes are implemented, they must be measured and monitored in the pursuit of continuous operational improvement.
Additional References
- “The Strategic Principles of Repeatability,” James Allen and Chris Zook, Bain & Company, May 4, 2012.
- http://www.bain.com/publications/articles/the-strategic-principles-of-repeatability.aspx Accessed January 4, 2013
- Allen J, Zook C. Repeatability: Build Enduring Businesses for a World of Constant Change. 2012. Harvard Business Press Books
- Latham A. Are We STILL Making Mistakes? – Five Keys to Predictable, Repeatable Processes. 2005. www.uncommonclarity.com
- Kennedy P, Leathley C, Hughes C. Clinical practice variation. MJA. 2010;193(8)
- Madsen L. Healthcare Business Intelligence: A Guide to Empowering Successful Data Reporting and Analytics. 2012. Wiley
- Page S. Power of Business Process Improvement – 10 Simple Steps to Increase Effective- ness, Efficiency, and Adaptability. 2010