Urgent message: The presentation of a pregnant woman to urgent care is often associated with consternation for both the patient and the provider. When a pregnant patient presents to urgent care with right upper quadrant pain, initial bedside ultrasound screening for gall bladder disease can facilitate initial interventions as well as expedite follow up care.
CASE PRESENTATION
History
A 25-year-old nulliparous female 24 weeks pregnant presented to urgent care 4 hours after onset of nausea, vomiting, and right upper quadrant pain. She was feeling weak with an acid taste in her mouth. Prior to this episode she reported good health and an unremarkable pregnancy for which she had been receiving routine prenatal care. She had a normal fetal anatomy ultrasound at 23 weeks gestation. No trigger food, travel, or substance exposure was identified. Her family history was negative for biliary disease.
Physical Examination
Her face was ashen, she was lying on the cart clasping an emesis bag. Mucus membranes were dry. Heart rate was regular and without excess heart tones. Lungs were clear to auscultation. Abdomen was gravid 24 cm above the umbilicus. There was no abdominal rigidity, guarding or rebound tenderness; she had no McBurney’s point tenderness although her Murphey’s sign was positive.
Point-of-Care Ultrasound
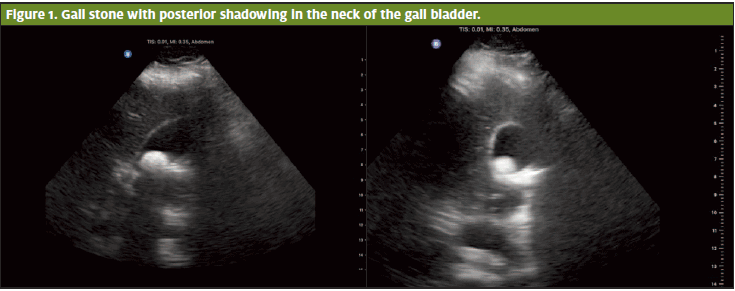
Bedside ultrasound showed good fetal movement and a measured heart rate of 154. Laying the patient in the left decubitus position simplified locating her gall bladder; brief sweeps in both long and short axis revealed a single large hyperechoic structure near the gall bladder neck with an accompanying posterior shadow. There was no pericholecystic fluid. The anterior wall of her gall bladder measured <3mm, sonographic Murphey’s equivocal and the common bile duct (CBD) was not visualized. These findings were consistent with cholelithiasis.
Follow-up
The patient was transferred to the emergency department where she had labs including liver function testing and lipase which came back normal. Formal ultrasound confirmed cholelithiasis without cholecystitis. She received IV fluids and antiemetics and felt much better.
Consultation with her obstetrician and general surgery resulted in recommendations for outpatient follow up.. Cholecystectomy was able to be postponed until two months post-partum. She had a successful vaginal delivery at 40 weeks 1 day gestation. Shortly after her cholecystectomy she returned to tolerating her normal diet.
Discussion
Gallbladder disease occurs in 20 million individuals in the United States, and is common in gravid women. The most common gallbladder disease in pregnancy is cholelithiasis, occurring in up to 3% of pregnancies. Risk factors include female sex, increased age, obesity, high serum lipid levels, as well as genetic predisposition.1,2 Women are at an increased risk during pregnancy due to the effects of progesterone and estrogen on the body.
Estrogen increases cholesterol secretion while progesterone reduces soluble bile acid secretion which leads to an increase in gallstone formation. Progesterone also slows emptying of the gallbladder.2 Both estrogen and progesterone naturally increase as gestational age advances, therefore increasing the risk of gallstone formation with advanced maternal age. Multiparous women have a higher risk of gallstone development (19%) compared to their nulliparous counterparts (7%).1
Biliary colic presents in pregnancy much like nongravid patients,6 with constant or intermittent pain in the RUQ that may radiate to the shoulder or scapula. The pain frequently presents as sudden onset often associated with eating, particularly after consumption of a high-fat meal. In general, biliary diseases in pregnancy are considered complicated.
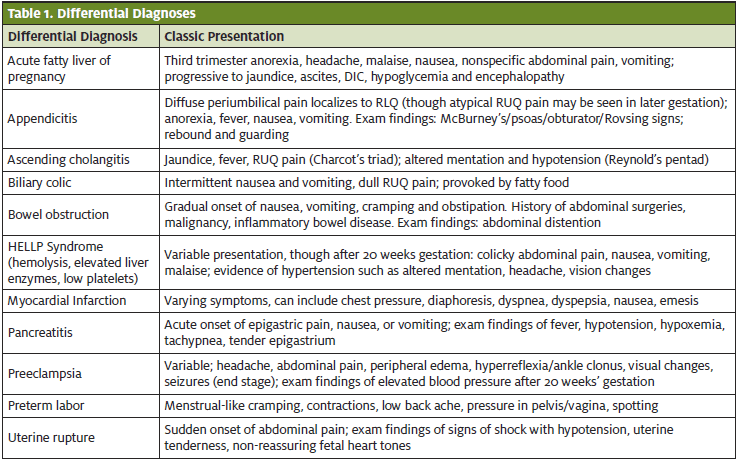
In pregnancy, POCUS can help to identify gallstones, although more serious etiologies (Table 1), still need to be excluded.
Conditions with high morbidity and/or mortality such as acute cholecystitis, appendicitis, ascending cholangitis, HELLP, myocardial infarction, preeclampsia, and pancreatitis deserve careful consideration even in the presence of cholelithiasis seen on POCUS. The literature supports the utilization of POCUS in a variety of specific clinical scenarios to assess for a number of pathologic processes; however, each application needs to be used within the indications and guidelines supported by evidence-based medicine. In the presentation of RUQ pain with or without pregnancy, the personal and family history, risk factors, exam findings, and ancillary tests all add to the clinical decision-making process.
POCUS is both sensitive and specific for assessing the presence of cholelithiasis as well as acute cholecystitis. These sonographic features are synonymous in the pregnant and non-pregnant patients.2 Bedside ultrasound can help accurately diagnose some biliary pathology and expedite the treatment process.3
POCUS involves assessing for the presence of:
- Gallstones or sludge
- Gallbladder wall thickening (normal is < 3mm)
- Pericholecystic fluid
- Sonographic Murphy’s sign
- Common bile duct (CBD) dilation (normal is <8 mm)
The last four features are characteristic signs of acute cholecysitis.1,3,4
Identifying the dilation of the CBD is the most technically challenging component of a limited RUQ sonographic exam, but is unlikely to be of benefit in patients with normal lab values, without sonographic Murphey’s sign, who have a gallbladder wall thickness <3mm, and have no pericholecystic fluid on POCUS.3
Ultrasound is the preferred imaging modality in pregnancy.5 The sensitivity and specificity of ultrasound for cholecystitis is 85% sensitive in pregnancy and 95% specific, compared to only slightly higher sensitivity and specificity with a CT scan, at 91.7% and 99.1% respectively.2
Outcome of Case
With this particular patient, obtaining the POCUS allowed for direct visualization of a stone and empowered the clinician to provide supportive measures immediately. Keeping in context this patient’s history, stable/afebrile vitals, and physical exam with additional ultrasonic measurements of a normal gall bladder wall thickness, and the absence of pericholecystic fluid, the clinician had sound reason to treat this pregnant woman with biliary colic in-house.
With her report of fetal movement, no uterine contractions or vaginal bleeding in addition to her ongoing stable vitals and clinical response to medical management, she had no indication for emergent transfer for higher level of care.
This scenario and discussion highlights a POCUS opportunity within the scope of urgent care to assist with providing an understanding of specific answers in the face of acute biliary symptoms in and outside of pregnancy. Bedside ultrasound can reduce resource expenditure as well as reduce time to diagnosis and definitive care. It is important to acknowledge red flags in pregnant individuals who present with acute biliary disease as they are relatively high risk individuals. UC clinicians may take an opportunity such as this to further patient advocacy and provide inter-specialty continuation of care.
Summary
- Acute biliary disease is common in pregnancy.
- It is important to remain alert for red flags suggestive of high morbidity and mortality biliary disease processes.
- POCUS has a role in pregnant and non-pregnant individuals present with biliary signs and symptoms.
- POCUS can reduce time to diagnosis and treatment in a number of biliary disease processes.
References
- Brown KE, Hirshberg JS, Conner SN. Gallbladder and biliary disease in pregnancy. Clin Obstet Gynecol. 2020;63(1):211–225.
- Gilo NB, Amini D, Landy H. Appendicitis and cholecystitis in pregnancy. Clin Obstet Gynecol. 2009;52(4):586–596.
- Lahham S, Becker BA, Gari A, et al. Utility of common bile duct measurement in ED point of care ultrasound: a prospective study. Am J Emerg Med. 2018;36(6):962–966.
- Villar J, Summers SM, Menchine MD, et al. The absence of gallstones on point-of-care ultrasound rules out acute cholecystitis. J Emerg Med. 2015;49(4):475–480.
- Committee Opinion No. 723 Summary. Obstet & Gynecol. 2017;130(4): 933–934.
- Lee RH, Chung RT, Pringle Prenosnik R, et al. Diseases of the liver, biliary system, and pancreas. In: Creasy RK, Resnik R, Iams JD, et al, eds. Creasy and Resnik’s Maternal Fetal Medicine: Principles and Practice. 7th Philadelphia, PA: Elsevier; 2019:1173-1191.
Chelsea M. Burgin, MD, FAAFP is the Medical Director of MD360 Boiling Springs and the Director of MD360 Ultrasound, Prisma Health and Assistant Clinical Professor, University of South Carolina School of Medicine Greenville. Meaghan A. Standridge is a medical student at the University of South Carolina School of Medicine Greenville. Kacey Y. Eichelberger, MD is the Chair of the Department of Obstetrics and Gynecology, as well as site Principal Investigator for the National Institute of Child Health and Human Development (NICHD)’s Maternal-Fetal Medicine Unit (MFMU) Network trials.


