RESOLUTION
Differential Diagnosis
- ST-Elevation MI (STEMI)
- Brugada pattern
- Diffuse subendocardial ischemia
- Hyperkalemia
- Long QT
Diagnosis
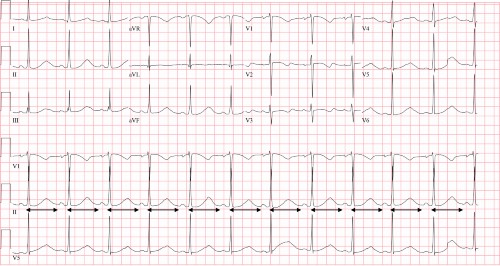
Long QT. The ECG reveals a regular, narrow-complex, sinus rhythm at a rate of 72 beats per minute. There is a normal axis and normal PR and QRS intervals. The QT interval is prolonged. There are no signs of acute ischemia. This ECG is neither consistent with ST-elevation MI nor diffuse subendocardial ischemia. There are no findings of hyperkalemia (ie, peaked T waves, widened QRS), and the ECG does not demonstrate the Brugada pattern (ie, coved ST-segment in lead V1 >2 mm or > 1mm in V1-V3 followed by a negative T-wave).
Measuring the QT interval
The QT interval is measured from the start of the Q wave through the end of the T wave (or U wave if present) and represents the time from ventricular depolarization through ventricular repolarization.1 The QT interval is inversely proportional to the heart rate—meaning the QT interval will shorten with faster heart rates, and lengthen at slower heart rates.
In order to standardize for heart rate, multiple formulas are available for a corrected QT interval (QTc), including the Bazett, Framingham, and Fridericia, among others.
A normal QTc is typically described as less than 440 msec in men, and 460 msec in women. The easiest way to remember risk associated with prolonged QT is an interval greater than 500msec, which is associated with an increased risk of ventricular dysrhythmias, particularly torsades de pointes (TdP), a type of polymorphic ventricular tachycardia.
Causes of prolonged QT
There are many causes of prolonged QT intervals, including:2
- hypokalemia
- hypomagnesemia
- hypocalcemia
- hypothermia
- congenital long QT syndrome
- myocardial ischemia
- elevated intracranial pressure
- medications
Management
Management is focused on the prevention of syncope and sudden cardiac death.3 Emergency treatment typically involves electrolyte repletion/treating the underlying cause and removal of the offending agent if medication- or drug-induced. Overdrive pacing is also a treatment option as the QT interval is inversely proportional to the heart rate (meaning the paced tachycardia is protective in patients with long QT).4
Syncope in the setting of a long QT should be viewed as secondary to a ventricular dysrhythmia until proven otherwise; patients should be admitted for telemetry monitoring.
The patient in the clinical scenario described here was determined to have a prolonged QT interval secondary to multiple medications she was taking—ondansetron, metoclopramide, and amiodarone.
Learnings/What to Look for
- A prolonged QT interval is associated with an increased risk of ventricular dysrhythmias, particularly TdP
- A prolonged QT can be caused by many different etiologies
- History and medication list review is imperative in patients with long QT
- Patients with syncope in the setting of a long QT should be admitted for telemetry monitoring and treatment of the underlying cause
Pearls for Urgent Care Management and Considerations for Transfer
- In patients with syncope, obtain an ECG and look specifically for a QTc >500ms, Wolff-Parkinson-White (WPW), Brugada, hypertrophic cardiomyopathy, ischemia, or findings associated with electrolyte abnormalities
- Patients with long QT should be placed on telemetry and monitored for ventricular dysrhythmias
- Identify and initiate treatment of the underlying cause
- Patients with symptoms which could be attributed to a prolonged QT interval (eg, syncope) should be transferred to a facility capable of providing telemetry monitoring
References
- Postema P, Wilde A. The measurement of the QT interval. Curr Cardiol Rev. 2014;10(3):287-294.
- Diercks DB, Shumaik GM, Harrigan RA, et al. Electrocardiographic manifestations: electrolyte abnormalities. J Emerg Med. 2004;27(2):153-160.
- Shah SR, Park K, Alweis R. Long QT syndrome: a comprehensive review of the literature and current evidence. Curr Probl Cardiol. 2019;44(3):92-106.
- Charlton NP, Lawrence DT, Brady WJ, et al. Termination of drug-induced torsades de pointes with overdrive pacing. Am J Emerg Med. 2010;28(1):95-102.
