Published on
What diagnosis explains the widened QRS?
This patient has a left bundle branch block (LBBB), which occurs when the left bundle no longer conducts, and the signal must pass to the left ventricle via myocyte-to-myocyte conduction. This pattern of conduction is slower than via the specialized conduction system, and results in a wide QRS complex (>120 ms). Conduction disturbances, like bundle branch blocks, result from structural abnormalities of the His-Purkinje system caused by necrosis, fibrosis, calcification, infiltrative disease, electrolyte disturbances, or impaired vascular supply. When conduction is impaired to both left ventricular terminals (the left anterior and posterior fascicles), the result is a LBBB.
What are the electrocardiographic criteria for making this diagnosis?
The criteria are:
- QRS >120 ms
- Dominant S wave in V1
- Broad monophasic or notched R wave in lateral leads (I, aVL, V5, V6)
- +/- left axis deviation axis deviation.1–3
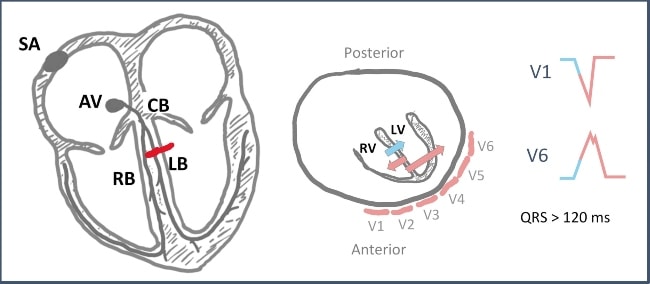
Depiction of depolarization in left bundle branch block. The septum first depolarizes from right to left (blue arrow) followed by near simultaneous depolarization of the right and left ventricles (pink arrows). The resultant vector leads to a negative deflection in V1 and a positive deflection in V6. SA, sinoatrial node; AV, atrioventricular node; RB, right bundle; LB, left bundle; CB, common bundle; RV, right ventricle; LV, left ventricle; red dash represents a block of the left bundle. (Illustration courtesy of Benjamin Cooper, MD, MEd, FACEP.)
What rule(s) can help diagnose acute myocardial infarction with an ECG like this?
The Sgarbossa criteria, or modified Sgarbossa criteria, can help diagnose acute myocardial infarction in presence of LBBB.4,5 Concordance describes ST changes in the same direction as the QRS complex and is a powerful predictor of myocardial infarction in the symptomatic LBBB; it is an indication for emergent reperfusion. The modified Sgarbossa criteria are:
- Concordant ST elevation of ≥1 mm
- Concordant ST depression of ≥1 mm in V1, V2, or V3, or
- Excessively discordant ST elevation defined as the ST/S ratio greater than 0.25
- The modified criteria are more sensitive and specific than the original criteria.
- See the video provided by ECG Stampede for detailed analysis.
Pearls for Urgent Care Management
- LBBB is an indicator of conduction disease, but generally does not require immediate attention in the acute setting
- Transfer to a higher level of care is indicated in the setting of instability, syncope, or chest pain or anginal equivalent
- The presence of Sgarbossa criteria suggests acute myocardial infarction and warrants immediate transfer to a cath-capable facility
References
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients with Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;140(8):e382-e482.
- Costa D Da, Brady WJ, Edhouse J. Bradycardias and Atrioventricular conduction block. Br Med J. 2002;324(March):535-538.
- Surawicz B, Childers R, Deal BJ, Gettes LS. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram. Part III: Intraventricular Conduction Disturbances a Scientific Statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. J Am Coll Cardiol. Published online 2009.
- Sgarbossa EB, Investigators G 1. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med. 1996;334(8):481-487.
- Meyers HP, Limkakeng AT, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: A retrospective case-control study. Am Heart J. 2015;170(6):1255-1264.
