Differential Diagnosis
- Benign early repolarization (BER)
- Acute pericarditis
- Evolving inferior ST-elevation myocardial infarction (STEMI)
- Non-ST-elevation myocardial infarction (NSTEMI)
- Posterior myocardial infarction
Diagnosis
This patient was ultimately diagnosed with an inferior ST-elevation myocardial infarction (STEMI), seen here in the early stage of evolution.
The rhythm is sinus with a rate of 50 beats per minute, the axis and intervals are normal. The astute provider will recognize the subtle ECG changes that predict inferior myocardial infarction including ST-straightening in the inferior leads, hyperacute t waves in the inferior leads, and reciprocal changes in aVL, V3, and V4 (Figure 2). The patient’s symptoms together with this ECG suggesting early inferior infarct are worrisome for acute coronary syndrome and pending inferior STEMI. A repeat ECG performed 20 minutes later confirm inferior STEMI (Figure 3).
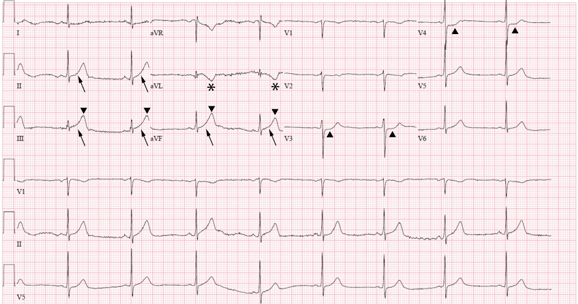
Figure 2. The initial ECG shows ST straightening in the inferior leads II, III, aVF (arrows) where the ST segments lose their normal concavity and start to “straighten.” The t waves in the inferior leads, while not large at first glance, are relatively large (or hyperacute) when compared to the size of their associated QRS complexes (). Often, the first reciprocal finding of an inferior myocardial infarction is a t-wave inversion in aVL (asterisks). Lastly, subtle reciprocal ST depressions can be seen in the precordial leads V3 and V4 ().
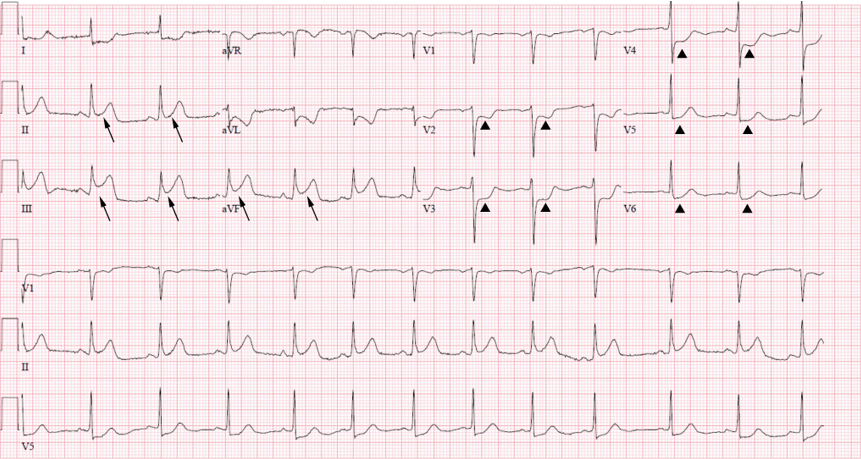
Figure 3. ECG performed 20 minutes later confirming the presence of an inferior MI. There is contiguous ST elevation in the inferior leads II, III, and aVF (arrows) with reciprocal ST depressions in aVL, and V2 through V6 ().
An inferior STEMI is present when at least two contiguous inferior leads (II, III, AVF) demonstrate >1 mm ST-segment elevation. Between 80% and 90% of inferior myocardial infarctions are due to occlusion of the right coronary artery, while the remainder are due to occlusion of the left circumflex artery.1 Often, the atrioventricular node can be involved as it generally shares the blood supply with the inferior wall, which can manifest clinically as atrioventricular blocks. Large inferior infarcts can also involve the right ventricle or extend to the posterior wall.1 Right ventricular involvement is often reflected as concomitant ST elevation in V1, the most rightward-oriented precordial lead, and can be further supported by application of right sided leads with ST elevation in V4R being the most sensitive.1 ST elevation in lead III greater than ST elevation in lead II can also suggest right ventricular involvement.1 This is prognostically significant, since right ventricular involvement implies a larger lesion and is associated with higher mortality rates.
Clinically, these patients are preload-dependent and may warrant intravenous fluid administration if hypotensive. It is key to avoid nitrates in this subset of patients as these are known to decreased preload.2
Posterior involvement is reflected electrocardiographically by horizontal ST depression in V1-V3, upright T waves, and tall R waves (late finding).3 Like right ventricular involvement, posterior extension implies larger infarctions, which carry a higher mortality rate.4 The ST depressions in V2-V6 manifested in the second ECG (Figure 3) may indeed represent posterior extension.
Benign early repolarization (BER)
Benign early repolarization is an ECG finding characterized by diffuse, fixed, concave-up ST-segment elevations without reciprocal changes, and notching of the terminal QRS complex.5 This finding is noted in 10%─15% of individuals presenting to emergency departments with chest pain and is considered as a nonpathologic normal variant. It is more prevalent in young, healthy individuals under the age of 50, and is relatively uncommon in those over the age of 50.5
Pericarditis
The pain associated with pericarditis is often described as sharp and pleuritic, relieved by sitting forward, and worsened by lying back. ECG findings of pericarditis include diffuse ST elevation, absent reciprocal changes, PR-segment depression, and sometimes a down-sloping ST segment known as “Spodick’s sign.” Like benign early repolarization, the ST segments of pericarditis are concave up, contrasting with the ST segment of STEMI which is often flat or concave down. It is important to note, however, that while morphology is suggestive, it is only a guide to interpretation and should not be considered in isolation when differentiating STEMI from other causes of ST elevation.6
Non-ST-elevation myocardial infarction
NSTEMI is diagnosed specifically by evidence of acute myocardial injury via elevated cardiac biomarkers (troponin I or troponin T).7 Though this patient’s initial ECG did not meet criteria for STEMI (owing to <1 mm ST elevation) and his initial troponin was not elevated, it is highly suggestive of an occlusive myocardial infarction. The subsequent ECG did meet STEMI criteria.
Learnings/What to Look for
- A new t-wave inversion in aVL can be the first electrocardiographic sign of inferior myocardial infarction
- Consider serial ECGs in patients for whom there is a suspicion for acute coronary syndrome, especially when presenting early in their course
- With inferior infarction, consider concomitant right ventricular involvement and avoid nitrates
Pearls for Urgent Care Management and Considerations for Transfer
- Administration of aspirin has a mortality benefit; administer 160-325 mg chewable aspirin with STEMI
- Immediate transfer to a percutaneous coronary intervention-capable facility is indicated in patients with suspected STEMI
- When transfer to a percutaneous coronary intervention-capable facility is unavailable or will results in delayed care (> 120 minutes), the urgent care physician should consider thrombolysis if possible8
References
- Zimetbaum PJ, Josephson ME. Use of the electrocardiogram in acute myocardial infarction. N Engl J Med. 2003;348(10):933-940.
- Ferguson JJ, Diver DJ, Boldt M, Pasternak RC. Significance of nitroglycerin-induced hypotension with inferior wall acute myocardial infarction. Am J Cardiol. 1989;64(5):311-314. d
- Morris F, Brady WJ. ABC of clinical electrocardiography: acute myocardial infarction—part I. BMJ. 2002;324(7341):831-834.
- Tiefenbrunn AJ, Chandra NC, French WJ, et al. Clinical experience with primary percutaneous transluminal coronary angioplasty compared with alteplase (recombinant tissue-type plasminogen activator) in patients with acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI-2). J Am Coll Cardiol. 1998;31(6):1240-1245.
- Brady WJ. Benign Early Repolarization: Electrocardiographic Manifestations and Differentiation from Other ST Segment Elevation Syndromes. Vol 16. Philadelphia, PA: WB Saunders; 1998.
- Morris F, Brady WJ. ABC of clinical electrocardiography: acute myocardial infarction—Part I. BMJ. 2002;324(7341):831-834.
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618-e651.
- O’gara P, Kushner F, Aschei D, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. Circulation. 2013;127(4):e362-e425.
