Differential Diagnosis
- Normal sinus rhythm (normal ECG)
- Low voltage
- Inferior STEMI
- Sinus bradycardia
- Brugada syndrome
ECG Analysis
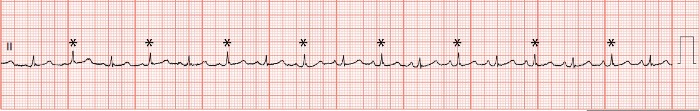
This ECG shows sinus rhythm with a rate of 102 bpm and low-voltage QRS complexes. Low voltage is defined as either 1) all limb lead amplitudes less than 5 mm or 2) all precordial lead amplitudes less than 10 mm.1 This ECG meets the precordial low voltage criteria, as the largest amplitude precordial QRS complex is 7 mm (in V2 and V3). Additionally, the QRS amplitudes in the rhythm strip of lead II can be seen to alternate between larger and smaller complexes, a phenomenon known as electrical alternans. The presence of electrical alternans suggest a pericardial effusion.
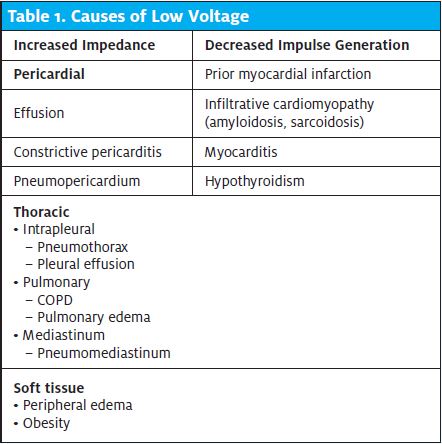
The differential diagnosis of low-voltage QRS can be separated into two categories: increased impedance and decreased impulse generation (Table 1).1
Careful consideration of this patient’s presentation and analysis of the ECG can secure the diagnosis. The presence of clear lungs makes thoracic diagnoses like pulmonary edema, COPD, and pleural effusion unlikely. The presence of electrical alternans (Figure 2) secures the diagnosis of cardiac tamponade. Electrical alternans is defined as alternating QRS amplitude, often resulting from the pendulous-like swinging of the heart inside a fluid-filled pericardium. Other pathologies associated with electrical alternans include Wolff-Parkinson-White, accelerated idioventricular rhythm, and supraventricular tachycardia.2,3
Cardiac tamponade occurs when fluid accumulates in the pericardial space, causing impaired right ventricular filling, and leading to hemodynamic compromise. Signs of tamponade include distended neck veins, muffled heart sounds, and hypotension (Beck’s triad).4
While this patient was normotensive, the presence of tachycardia and tachypnea suggests she is at high risk for hemodynamic collapse and warrants immediate transfer. If the patient is hemodynamically unstable, the urgent care provider should immediately obtain intravenous access and fluid resuscitate, as these patients are preload dependent. Cardiac tamponade is an emergency and patients with suspected tamponade should be immediately transferred to a higher level of care for a pericardiocentesis or a surgical pericardial window.
Learnings/What to Look for
- Low voltage is defined as either 1) all limb lead amplitudes less than 5 mm, or 2) all precordial lead amplitudes less than 10 mm
- Electrical alternans is a phenomenon seen when the heart moves rhythmically inside a fluid-filled pericardium, predictably altering the electrocardiographic voltage
- Exam findings include clear lungs, jugular venous distension, and muffled heart sounds (Beck’s triad)
- If ultrasound is available, tamponade physiology is diagnosed by observing right ventricle collapse during diastole
Pearls for Urgent Care Management
- If cardiac tamponade is considered, immediately obtain intravenous access
- Intravenous fluids may be used to promote right ventricular filling
- Initiate immediate transfer to a facility capable of performing a pericardiocentesis and/or surgical pericardial window
References
- Madias JE. Low QRS voltage and its causes. J Electrocardiol. 2008;41(6):498-500.
- Ingram D, Strecker-McGraw MK. Electrical Alternans. StatPearls. August 11, 2021. Available at: https://www.ncbi.nlm.nih.gov/books/NBK534229/. Accessed January 3, 2022.
- Goyal M, Woods KM, Atwood JE. Electrical alternans: a sign, not a diagnosis. South Medical J. 2013;106(8):485-489.
- Honasoge AP, Dubbs SB. Rapid fire: pericardial effusion and tamponade. Emerg Med Clin North Am. 2018;36(3):557-565.
