Urgent message: The risk in not “doing the math” with a patient’s risk factors is obvious for that patient. However, urgent care providers and operators also run significant legal risk when patients with multiple complaints present and there’s a bad outcome—even if the most pressing complaint is impossible to discern.
Michael B. Weinstock, MD; David A. Farcy, MD FAAEM, FACEP, FCCM; and Ramin Vejdani, DO
[This case was adapted from a chapter in the book Bouncebacks! Critical Care by Michael B. Weinstock, MD; Kevin Klauer, MD; and Scott Weingart, MD. The book is available from www.anadem.com, www.ohacep.org, or www.amazon.com.]
The Patient’s Story
Stacy is a hard worker, at one point working three jobs: cleaning the credit union and Mr. Payroll during the day and working at UPS at night. According to her mother, “She never stopped working. She did whatever anybody needed her to do.”
At the age of 26, Stacy delivers a healthy baby girl, Celina. During the delivery, Stacy suffers a “diabetic stroke” and is told to have a tubal ligation. At this time, she is married to Leo, but the marriage ends badly and she is left to raise Celina on her own; Leo does not provide assistance. Though she does not have much money, Stacy is a wonderful mother, supporting her daughter’s interest in gymnastics and taking her to the beach. Through the years, Celina becomes her “best friend.”
In her early 30s Stacy starts dating a man named Robert. At one point, she walks upstairs after doing laundry and overhears Robert saying, “I don’t want the baby. You might as well do something with it. I don’t want it.” When confronted, he denies the conversation so Stacy calls the woman Robert had been speaking with back and says, “I’ll take the baby. I’ll raise him as my own.” She borrows money for the adoption papers and brings the baby home from the hospital, calling him Matthew.
On October 2, Stacy calls her mother and tells her she is having pains in her chest. “Do you think its indigestion?” her mother asks.
“No.” Stacy replies. “I’ve been taking something for indigestion and it’s not working.”
Stacy decides to be evaluated.
41-YEAR-OLD WOMAN WITH CHEST PAIN
(What follows is the actual documentation, including spelling and punctuation errors.)
NKDA
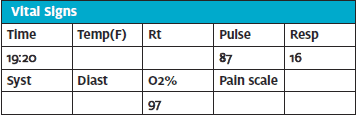
PMH: HTN, CVA, DM
PSH: Choly
SH: Smoker
Meds: Glucophage, Avandia, Norvasc, Accupril – pt out of meds last 3 months
HPI (18:55 – MD note): Pt is a 46-year-old woman with chief complaint of chest pain for the last 1 day or so. Pain is a tightness across the chest and upper arms which is worsened by deep breaths. Radiates to the left arm. PMH of high blood pressure and diabetes. No nausea and vomiting, coughing blood, syncope, feeling of doom, shortness of breath, sweating and palpitations. Nursing notes reviewed. SH Smoker. FH: Hx cardiac disease after the age of 55
PE
General: A&OX3, appears very uncomfortable
Eyes: PERRL
CV: RRR without m/r/g. Normal heart sounds. Good capillary refill. No peripheral edema
Resp: No resp distress. Prolonged splinting and decreased air movement and wheezing.
Abd: Soft and NT throughout, without r/r/g
Back: No CVAT
Skin: Normal without petechiae, vesicles, erythema
CXR (19:11) – WNL. Fingerstick BS= 255
Resp: No resp distress. Prolonged splinting and decreased air movement and wheezing.
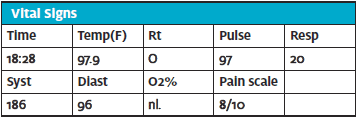
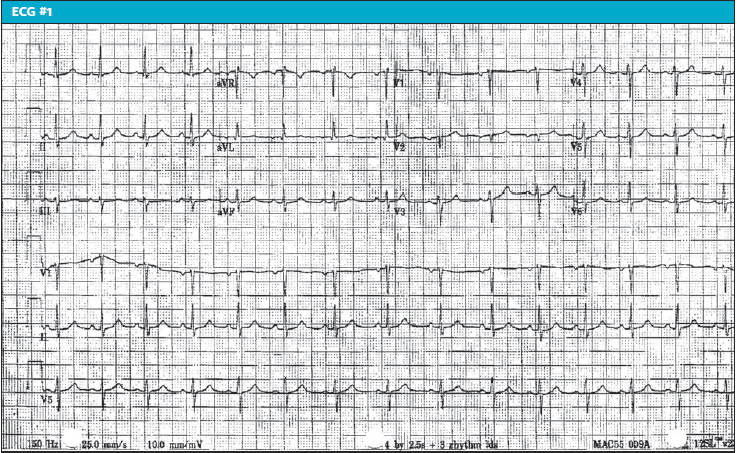
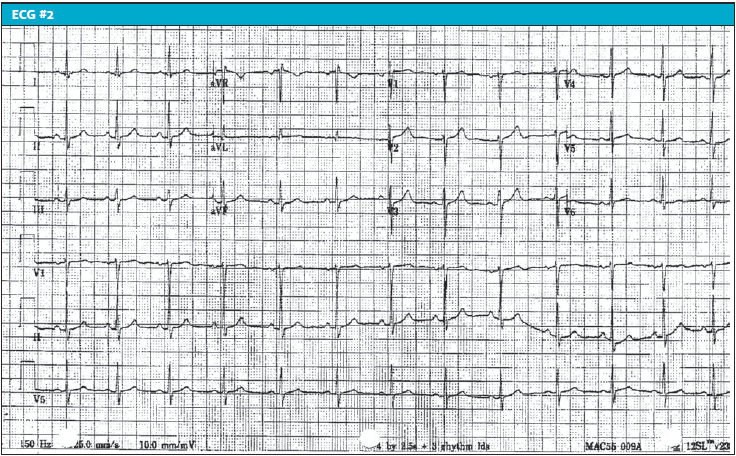
ECG#1 @ 19:20
Vent rate 89 bpm Normal sinus rhythm
PR interval 148 ms Septal infarct, age undetermined
QRS duration 80 ms Abnormal ECG
QT/QTc 368/447 ms
P-R-T axes 62 14 44
Albuterol aerosol #1 (19:20)
Albuterol aerosol#2 (19:31)
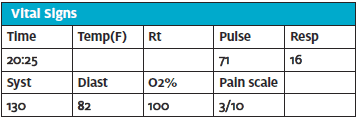
ECG#2 @20:25
Vent rate 79 bpm Normal sinus rhythm
PR interval 148 ms Normal ECG
QRS duration 80 ms
QT/QTc 382/438 ms
P-R-T axes 66 33 56
MDM/ED course: “CXR and ECG’s reviewed. Albuterol aerosol, captopril 25mg PO”
Diagnosis: HTN, bronchospasm
Condition: Stable
Disposition: Home
RN: d/c home with driver. Pt states pain much better. Verbalizes understanding
Discussion of the Initial Visit—Evaluation of Chest Pain, Medical Decision-Making, Documentation, and Patient Safety
This seems a straightforward case of “typical” angina with risk factors that include diabetes (noncompliant), smoker, history of coagulopathy with TIA, and a potential positive family history. Certainly, a more thorough history and work-up could have been performed, as well as better documentation of the medical decision-making process. We believe that the initial physician anchored on the diagnosis of “bronchospasm,” even though the patient did not have a history of asthma or COPD (though she is a smoker). There are five historical factors associated with acute coronary syndrome (ACS),1 including:
- Exertional pain
- Radiation
- Diaphoresis
- Vomiting
- Pain similar to past episodes of ACS
What is the patient’s ‘question’? What is the presentation’s ‘question’?
It is essential that we understand not only the patient’s question, beyond “Am I having a heart attack?” as evidenced here, but also what the patient’s presentation is asking.
In Stacy’s presentation, a wide differential remains, including not only the possibility of a “heart attack” but also pulmonary embolism (she has chest pain which is pleuritic; “…worsened by deep breaths”), as well as aortic dissection (she is at increased risk with her history of hypertension and we don’t know if the pain radiates to the back).
Do the plaintiff’s attorneys understand this also? Consider the opening statement at Stacy’s trial:
Opening statement by plaintiff attorney
Opening statement by plaintiff attorney:
“Good morning, everybody. One of the major reasons people come to EDs in the U.S. is because of chest pain. Not all of it is fatal. And it’s not always easy to diagnose. And the rule in EDs is that you treat chest pain as a heart attack until you rule it out. That’s the rule. The evidence is going to show that when Stacy left the hospital with her friend Doneen, they were in shock. Doneen regrets to this day that she did not bar the door and say, “No, we’re not leaving. We’re not leaving.”
BACK TO THE CASE – THE DOCUMENTATION
What could have done to keep our patient safer—and to decrease our own medical legal risk?
- Lack of correlation between chief complaint and final diagnosis
Let’s start with the biggest problem with this evaluation—the final diagnosis of HTN, bronchospasm; this has no correlation with the presenting chief complaint (chest pain – pain from above waist to head, neck and arms). Bronchospasm typically presents with an intractable cough and wheezing, though as the bronchospasm worsens, an increased obstruction to air entry might limit the auscultation of audible wheezing secondary to lack of poor air exchange. The patient’s chief complaint is chest pain with a respiratory rate of 20 and normal oxygen saturation; a focused review of systems stated no shortness of breath and the physical exam showed “no respiratory distress. Prolonged splinting and decreased air movement and wheezing.”
In short, nothing in the history or physical exam supports a diagnosis of bronchospasm. There is no cough, accessory muscle use, tachypnea, history of asthma or COPD, or previous history of respiratory problems. The chart does point out chest pain: “Pain is a tightness across the chest and upper arms which is worsened by deep breaths. Radiates to the left arm.”
Is a physician’s gestalt good at predicting the diagnosis and outcome in patients with ACS? Unfortunately not, with multiple studies showing that gestalt alone had little to moderate diagnostic value compared to gestalt plus electrocardiogram (ECG) and troponin.1,2
- Poor history
History taking is an art. We are asking questions not just to meet the billing standard, but to also show consideration of “worst first.” All nontraumatic chest pain patients need to be risk-stratified as either low or high risk. In a 41-year woman with chest pain, our differential includes:
- Acute coronary syndrome (ACS)
- Pulmonary embolism (PE)
- Thoracic aortic dissection (TAD)
- Pneumothorax
Because there is essentially no medical decision making (MDM) section, we need to default to the history, exam, and evaluation to determine what this provider actually considered in the differential. Unfortunately, the chart points only to consideration of ACS (two ECGs were done). One could argue that pneumothorax was considered because a chest x-ray was ordered, though there was not a preliminary EP interpretation specifically addressing pneumothorax. It would have been nice to see an interpretation which stated that “there is no evidence of PTX or a widened mediastinum.”
Do attorneys understand the importance of a good history? Consider this exchange:
Cross examination of defendant physician by plaintiff attorney:
Q. Now, in order to put the pieces of the puzzle together for what is causing chest pain, you need to get an accurate history, don’t you?
A. Yes, sir.
Q. You don’t just take the patient’s words for it. There are criteria for doctors to probe into what exactly the nature of the pain is, isn’t that correct? Those questions should have been asked, correct?
A. Yes, sir, they typically would be asked.
Q. And the reason they need to be asked is because we’re dealing with something that could be missed and you need as much information to put the puzzle together?
A. Yes, sir.
- The ECG
Can an ECG aid in ruling out ACS? The initial ECG has a sensitivity of 20% to 60% for AMI, similar to flipping a coin.3 If the ECG has ST-segment depressions >0.05 mV with or without T-wave inversions, sensitivity increases to about 75% al).4 Unfortunately, the 12-lead has geography limitation, leaving the inferior and posterior wall untraced. Our patient had two ECGs, but if there was sufficient concern for ACS, perhaps a troponin would have aided in the diagnosis, as well as additional data gathering, including risk factors.
- Risk factors
Since gestalt combined with an ECG is not much help in ruling out ACS, what should we do? An assessment of risk factors originally came from the Framingham study group, which looked at the risk of developing cardiovascular disease over 10 years. A patient with no risk factors does not eliminate the possibility of ACS, but does decrease the risk.5,6 However, one study showed that in patients less than 40 years of age with a very high-risk factor burden (4 to 5 risk factors), the likelihood of ACS was increased by >20-fold.7
Do attorneys know about the importance of obtaining risk factors?
The plaintiff’s attorney was clever and did not leave anything to chance; there is only one way to answer their questions. Consider this exchange:
Plaintiff attorney to the defendant physician Q. Let’s count the risk factors. One, diabetes, right?
Defendant physician: A. Yes, sir.
Q. Two, smoking, correct?
A. Yes, sir.
Q. Three, hypertension or blood pressure, correct?
A. Yes, sir.
Q. Four, stroke?
A. Yes, sir.
Q. Correct? Five, age over 40, correct?
A. Yes, sir.
Q. Six, family history?
A. Yes, sir.
Q. It’s a bunch, isn’t it?
A. Yes, sir.
- Decision tools
The HEART score, originally developed in 2009 and validated in 2013, predicts a very low rate of a major adverse cardiac event (MACE) at 4-6 weeks for low-risk patients.5,6 We do not have any indication that the HEART score or any other decision tool was considered—and in fact, without obtaining a troponin, it would have not been possible to calculate.
H – History
E – ECG
A – Age
R – Risk factors
T – Troponin
Additionally, a multicenter study by Weinstock, et al looked at over 45,000 chest pain patients with interpretable and nonischemic ECGs, nonconcerning vital signs, and two negative troponins, finding an exceedingly low rate of a clinically relevant adverse cardiac outcome (CRACE).8 Our patient did not have any troponin testing done.
- Poor documentation of medical decision-making (MDM)
Historically, clinicians over-document the catastrophic case, thinking they may be involved in a lawsuit. However, it is rarely those cases that come back to haunt us; rather, it’s the cursory evaluation and discharge. In our case, there is no MDM, just a statement: “CXR and ECGs reviewed. Albuterol aerosol, captopril 25 mg PO.”
Hard stop your MDM!
In patients with diagnostic uncertainty about a potentially life-ending complaint (like ACS, PE, or TAD in this case), “hard stop” your MDM; prior to discharge, ensure that it has been discussed why serious life-threatening diagnoses are not occurring. If you find that there is not enough information to make this decision (as in this case), go back to the bedside and obtain additional data. Before the patient leaves, ask if they would be comfortable explaining your care to the patient’s family or friends; if not, reassess and re-explain in the MDM.
If there is an adverse outcome, “experts” can argue at your disposition/trial, but not against your thinking; even if there is a bad outcome, your decision-making process is well-described and sound, which is defensible.
Of note, the considerations of PE (in a patient with pleuritic pain who is over the age of 35 and who is a smoker on oral contraceptives) and TAD (in a patient where there is no specific exclusion of pain radiating to the back) have still not been appropriately explored or excluded. Unfortunately, during the initial visit, the physician seems to have come to premature closure and anchored on a diagnosis of bronchospasm.9
- Women with ACS present differently than men This patient’s age and medical history alone give her four significant risk factors, which puts her in a high-risk category. To add to the complexity, women experience significant differences in their presentation of ACS, leading to higher morbidity and delay in diagnosis of ischemic heart disease compared to men.10-12
- Tips to evaluating a multiple-complaint patient
Unfortunately, multiple-complaint patients take longer, but it is essential to maintain an appropriate differential and ensure that our evaluation is logical. Instead of viewing the patient as difficult, try to determine their underlying reason for presentation. This approach will provide insight into their main concern.
Bringing It All Together
Now let’s go back and look at our patient, who had a chief complaint and many associated complaints. There was a poorly obtained history and an inadequate attempt to correlate the complaints into a cohesive story. Just considering her history of noncompliance puts her in a higher risk category. (Spoiler alert: the actual diagnosis was not “HTN, bronchospasm.” Something big was missed. At trial, the plaintiff’s attorney focused on inadequate gathering of data, specifically risk factors, and lack of consideration of life-threatening causes of chest pain.
THE STORY CONTINUES (extracted from trial testimony)
When Stacy returns home from the hospital, she tells her daughter she is feeling better. As everything seems fine, Celina goes to bed around 10 pm, only to be awoken around 2 am by the sounds of her mother moving around the kitchen. According to Celina, “I went in there to see what was going on and [my mom] went outside to smoke a cigarette, so I went out there and sat [on the front steps] with her. She told me that she loved me and that everything was going to be OK and she was sorry if she ever did anything to hurt me or my brother.
“I told her I loved her, too and that it was OK. She gave me a hug and kiss and then I went back to bed.
“[The next thing I remember is] my mother’s boyfriend Steve waking me up screaming and crying because my mom is on the floor and she is not talking to him. I called 911 and they told me to give CPR. I tried it but nothing helped.”
ED Return (early the next morning):
CC: Cardiac arrest
EMS (summary-time of arrival on scene 04:21; verbatim from handwritten notes; see Figure 1): 41 yo F apneic and pulseless according to family. Pt was up making coffee and collapsed. They stated she has been c/o chest pain for a couple of days. Pt unresponsive CPR and BVM assist with 100% O2. ET tube 7.5 25cm @ lip. Tube secured. BX X4 clear. IV. Epi 1:10000 1mg ivp. Pt rhythm changed to v-fib. Pt shocked 200 biphasic. Vasopressin 40 units IVP. Rhythm still v-fib. 300J shock biphasic. Amiodarone 300mg ivp. No change. CPR continues. Pt transported to hospital without incident or change. Report given to staff. Pt placed in hospital bed.
Figure 1. Handwritten EMS Sheet
ED Documentation
HPI (physician): Presents via EMS w witnessed arrest by husband. Pt had complained of chest pain prior to arrival. EMS information reviewed. Pt is unable to give additional information secondary to medical condition of cardiac arrest
PE
GENERAL: Unresponsive, CPR in progress
EYES: Pupils dilated and unresponsive
Neck: Normal
CV: No spontaneous heart tones
LUNGS: Clear with equal breath sounds with bagging
ABD: Slightly distended
Ext: Normal
ED course
EMS arrival on scene 04:21
Pt arrives in ED @ 0500 in full arrest:
ED Code Sheet (verbatim from the actual ED document)
EMS stated they arrived and found pt pulseless and apneic @0421.
EMS arrived at ER at 0500.
0500 Arrival and attached to cardiac monitor
BS checked and confirmed
ETT 7.5 @ 22cm lip
0502 CPR continued
Epi 1mg
Atropine 1mg
Bicarbonate 50mEq
0508 Shock, 150J
PEA, CPR continued
Lidocaine 100mg
0509 Epi 1mg
CPR held, Wide complex Bradycardia
2nd IV initiated at R AC (20ga), blood drawn
Dopamine @ 20mcg/kg/min (at weight – 80 kg
BG – 343
The resus continues:
0519 – Pulse check reveals no pulses. CPR is continued
0520 – Vfib
Shock 150J
Atropine 1mg
0522 – CPR held – no pulse
0523 – CPR started
Epi 1mg IVP
Shock 150J
0526 – Epi 1mg IPV
0527 – Bicarbonate 50mEq
0531 – CPR held, pulses present.
0532 – Rhythm strip shows:
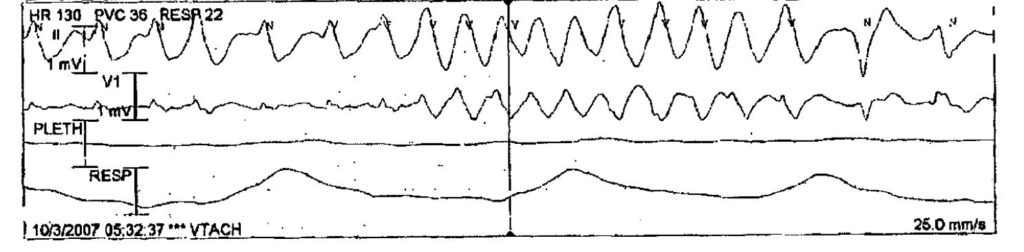
0534 –
Shock 150J
Shock 150J
Wide complex sinus rhythm – heart rate is 143. Pulse ox 72%
0537 – Amiodarone 150mg
Shock 150J
0538 – Levophed 4mg/250ml wide open. Heart rate is 90. Sat is 72%. Summary: Dopamine and levophed are running
0539 – Pulse check = no pulses. CPR is continued
0540 – V fib
Shock 150J
Shock 150J
0542 – Pt apneic and pulseless
0543 – Code called
0619 – Numerous family and friends arrive and are taken into the room by the chaplain to view the body
An autopsy reveals:
Acute myocardial infarction
Severe atherosclerotic involvement of the circumflex and the right coronary artery
Patchy fibrosis of the myocardium
Medical history of hypertension, diabetes mellitis and prior cerebrovascular accident
CAUSE OF DEATH: Acute myocardial infarction due to severe atherosclerotic heart disease.
THE LEGAL
Shortly after Stacy’s untimely death, a malpractice action was entered, proceeding to discovery, depositions, and eventually a trial, some of which was reproduced here. Allegations of malpractice are entered not only against the initial treating physician, but against the hospital and nursing staff. As it turns out, the hospital had recently rewritten its procedure for triage with a recommendation to assign a triage category of 2 for chest pain patients, but Stacy had only been assigned a category of 3, in direct contradiction of the hospital’s own policy.
The Plaintiff Strategy
Stacy collapsed at her home just over 7 hours after ED discharge. The pathologist who performed the autopsy testified that Stacy had severe atherosclerosis of the circumflex coronary artery and the right coronary artery. The left anterior descending artery had moderate atherosclerosis. A discolored region along the lateral side of the left ventricle indicated an acute MI.
The plaintiff’s expert on emergency medicine testified that the hospital’s nurses contributed to Stacy’s death, partly because they assigned an incorrect triage category. They further suggested that the proper treatment for unstable angina is to first make the diagnosis by assessing myocardial function, performing a cardiac perfusion study, or taking the patient directly to cardiac catheterization or CT angiography. Based on these findings, a decision would be made as to angioplasty and stenting or a bypass. The expert did not believe that either the doctor or the nurses intentionally harmed Stacy, but Stacy presented with symptoms that were very consistent with unstable angina and myocardial infarction. In his opinion, with her significant risk factors of hypertension, smoking, and diabetes, the possibilities of myocardial infarction and unstable angina were not adequately evaluated.
The Defense Strategy
Though there was a delay in obtaining the ECG, there was no reason to believe that doing so earlier would have changed the management. The chart reflects the presence of multiple risk factors for coronary artery disease; however, Stacy exhibited no associated symptoms—nausea and vomiting, coughing blood, syncope, feeling of doom, shortness of breath, sweating, palpitations. A physical examination of her cardiovascular system—regular rate/rhythm, no murmur, no gallop, no friction rub, pulses full/equal—presented in normal range. She was not cyanotic, diaphoretic, or pallid. There were two “ECGs with a whole day of pain, not having acute changes.” Because his impression was that Stacy’s chest pain was of non-cardiac origin, the doctor did not order cardiac enzyme tests. According to the doctor, the level 3 triage assigned to Stacy provided more than enough time for him to make the correct decision.
The discharge nurse told Stacy to return to the emergency room if the pain returned or worsened. The doctor instructed Stacy to set up an appointment the following day with her doctor to address her high blood pressure. The discharge instructions informed Stacy to call sooner if she thought it was necessary, and to return immediately if her symptoms worsened.
THE TRIAL: An unexpected twist
Some of the trial testimony was detailed earlier in the article, but sometimes there is an unexpected twist! When the plaintiff attorney gets the defendant physician on the stand, he tries to shame him into admitting he is wrong and that his care led to the death of the patient:
Plaintiff attorney examination of defendant physician:
Q. Wouldn’t it be nice to learn from a traumatic experience? Wouldn’t it be nice to learn from somebody’s death and be willing to say, “You know what? Maybe let’s go back and retrace our steps. Do we want this to happen again?”
A. No sir, I think about this every day, I do not want it to happen again. This is very emotional for me. Do you know why I am a doctor? When I was 16…
Q. Your honor, can I have the witness instructed to…
A. I’m answering your question
Q. Your honor, can I have the witness instructed to…
A. It’s important for me to let this out. You asked me a question.
Q. Your honor…
The court:
Just a minute everybody, listen very carefully. Doctor, you will have a full opportunity to give your side of the story when counsel questions you. At the juncture, please answer the plaintiff’s questions. I understand it’s emotional for you and you want the jury to understand. You will have your opportunity, at this juncture, simply answer his question.
Defense attorney examination of defendant physician:
Q. Doctor, you’ve been on the stand for a few hours. While you were giving testimony a few moments ago, you started to say something about why you became a physician and the plaintiff counsel stopped you. Would you like to share that with the jury?
A. Yes sir, he had asked if I understand what they’re going through. When I was 16 I took a chemistry test and the secretary came and told me, “You’re to go right home.” I drove home. My mother had died of a heart attack at age 42. I understand what they’re going through. This is a horrendous case for me. When they subpoenaed the documents, I mean, I literally sat down and sobbed, that—that—that I—all of those risk factors and everything is on there. And if the nurses mistriaged it, it’s my job to do that. And even there is enough information there, that I missed this. I don’t know how I missed this. But I understand very well what they’re going through. I go through it every day, I think about this case because it’s almost an ironic mirror image of what happened. My mom had had some chest pains. Her doctor thought she was just an anxious housewife that drank too much sherry and it turns out she dropped dead of a heart attack at 42. So I’m very much aware of what they’re going through. This is a very emotional case. And, again, I’m—I’m sorry that I am reacting this way, but this is—I understand what they’re going through
Q. Thank you for sharing that, doctor.
What follows next is truly astounding. The physician, besieged by genuine guilt and self-doubt, admits that he was wrong. One a side note, there were two legal actions: one against the physician, and the other against the hospital. Read on.
Defense attorney examination of defendant physician:
Q. You know what I’m getting at. At the hospital, worst-case scenario, her chances are tremendously better than in a trailer park? You checked that she was stable when she left the hospital, correct?
A. I appear to be in error about her being stable.
Q. Whoa. Wait, wait. What did you just say?
A. I appear to be in error in checking she’s stable. History has shown the fullness of time, she apparently had unstable angina, and so was not stable at discharge.
Q. So, you –
A. I was in error. I made a mistake. The nursing staff didn’t make a mistake. The hospital didn’t make a mistake. I made a mistake. I had a lady that had many risk factors. I thought I had answered her complaint with her BP and her bronchospasm and the two EKGs that didn’t have evolving change. I thought she was stable. I was wrong. I failed her.
TRIAL OUTCOME
Jury sides with plaintiff. According to the newspaper report, “The jury hit the hospital with a $1.4 million verdict Thursday, concluding that the hospital nurses were negligent in their treatment of the late Stacy.” The hospital appeals, as in Texas there is a very high standard of malpractice saying the physician’s actions need to be “Willful and Wanton.”
VOTE ON APPEAL
“We hold that the evidence of deviation from the standard of care by [the hospital’s] nursing staff is legally insufficient to support the jury’s finding that the willful and wanton negligence of the hospital was a proximate cause of Stacy’s death,” the opinion states. Accordingly, we reverse the trial court’s judgment and render a take-nothing judgment.”
Take-home points, medical and legal
The approach to finding negligence with the initial doctor and hospital is simple, as our patient was a walking disaster when she entered the hospital. First, there is no relationship in the documentation between the chief complaint and the diagnosis; this is a mountain which is difficult to climb. Second, she is high-risk with multiple risk factors. Third, the ECG was not normal. Exactly when her infarct took place is difficult to determine, but considering all factors, this woman should be considered to have acute coronary syndrome. Confusing a jury with whether she should have been a category 2 or a category 3 is useless. She had a concerning presentation; that’s enough! The triage category would not have changed the work-up. But the larger picture is clear. She has just about every risk factor, and we do not have another explanation for her chest pain.
Defending the Physician(s)
There is no question that being a defense expert for the first treating physician would be extremely difficult. Juries like cases which are simple and easy to understand. They don’t want to have to balance multiple people who have made multiple errors.
Hospital Liability
It is interesting to note that the 9th Circuit Court of appeals found the evidence legally insufficient for juries to find against the hospital. This usually means the hospital personnel—ie, the nurses. Although the initial verdict included everyone, the court was essentially also focused on the first visit. It is also interesting that the initial EM doctor settled for $150, 000, while the hospital opted to take its chances in court. The attorney for the initial physician was very wise. The fact that the initial judgement was reduced from $1.2 million to $330,000 does say something about the legal system. It is also noted that the 9th Circuit Court issued an opinion finding in favor of the hospital, saying, “We hold the evidence of deviation from the standard of care by nursing is legally insufficient to support the jury’s finding that willful and wanton negligence of the hospital was a proximate cause of this death.” The court therefore gave to the hospital essentially a “take nothing” judgement, meaning they got themselves out of the case.
Was It Fair?
The “willful and wanton” negligence, now the standard in the state of Texas, certainly had an impact on the results. Instead of coming away with $1.4 million, the patient’s family comes away with $150,000, a small amount to provide for parentless children, especially after attorney fees are deducted. Fairness is difficult to judge.
Citation: Weinstock M, Farcy D, Vejdani. A 41-Year-Old Woman with Multiple Complaints. J Urgent Care Med. September 2020. Available at:
References
- Fanaroff AC, Rymer JA, Goldstein SA et al. Does this patient with chest pain have acute coronary syndrome? The rational clinical examination systematic review. JAMA. 2015;314(18):1955-1965.
- Dezman ZD, Mattu A, Body R. Utility of the history and physical examination in the detection of acute coronary syndromes in emergency department patients. West J Emerg Med.2017;18(4):752-760.
- Speake D, Terry P. Best evidence topic report: first ECG in chest pain. Emerg Med J. 2001;18:61–62.
- Forberg JL, Green M, Björk J, et al. In search of the best method to predict acute coronary syndrome using only the electrocardiogram from the emergency department. J Electrocardiol. 2009;42:58–63.
- Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013;168(3):2153–2158.
- Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16(6):191-196.
- Han JH, Lindsell CJ, Storrow AB, et al. The role of cardiac risk factor burden in diagnosing acute coronary syndromes in the emergency department setting. Ann Emerg Med. 2007;49(2):145–152, 152.e1.
- Weinstock MB, Weingart S, Orth F, et al. Risk for clinically relevant adverse cardiac events in patients with chest pain at hospital admission. JAMA Intern Med. 2015;175(7):1207-1212.
- Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med. 2002;9(11):1184-1204.
- Canto JG, Rogers WJ, Goldberg RJ, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. 2012;307(8):813-822.
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non ST-elevation acute coronary syndrome: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e344-426.
- Crea F,Battipaglia I, Andreotti F. Sex differences in mechanisms, presentation and management of ischaemic heart disease. Atherosclerosis. 2015;241(1):157-168.
Author affiliations: Michael B. Weinstock, MD, Adena Emergency Medicine Residency, Adena Health System; Department of Emergency Medicine, Wexner Medical Center at The Ohio State University; Emergency Medicine Reviews and Perspectives (EM RAP); The Journal of Urgent Care Medicine; Urgent Care Reviews and Perspectives (UC RAP); Ohio Dominican University Physician Assistant studies program. David A. Farcy, MD FAAEM, FACEP, FCCM, Department of Emergency Medicine, Emergency Medicine Critical Care, Mount Sinai Medical Center;
Department of Emergency Medicine & Critical Care, Herbert Wertheim College of Medicine,
Florida International University; American Academy of Emergency Medicine. Ramin Vejdani, DO, Mount Sinai Medical Center.

