Differential Diagnosis
- Ventricular tachycardia
- Left bundle branch block
- Accelerated idioventricular rhythm
- Supraventricular tachycardia with aberrancy
- Hyperkalemia
Diagnosis
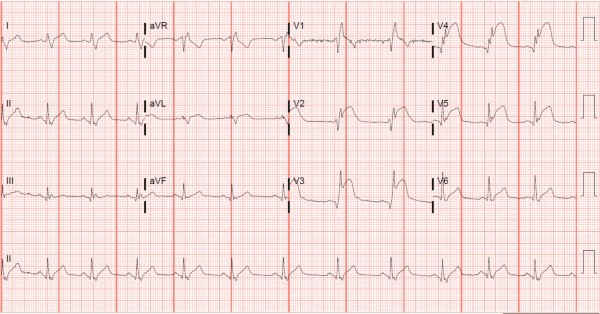
This patient was diagnosed with accelerated idioventricular rhythm. The ECG shows a wide QRS complex (>120 ms) with a regular rhythm at a rate of 90 beats/min. There are no P waves preceding the QRS complexes, suggesting an ectopic impulse-generating focus. This ECG is consistent with an accelerated idioventricular rhythm (AIVR).
AIVR is a rhythm that occurs under conditions of enhanced automaticity. An enhanced ectopic ventricular pacemaker outpaces more superior pacemakers (eg, sinus node) and, thus, becomes the dominant pacemaker. It occurs at a rate faster than ventricular escape, but slower than ventricular tachycardia (ie, between 50 and 110 beats/min). AIVR can occur for many reasons, including electrolyte abnormalities and drug toxicity (eg, digoxin); however, it occurs most commonly in the setting of reperfusion—that is, after myocardial infarction or cardiac arrest. The prognosis is not adversely affected because the ventricular rate is in the normal range.1,2
AIVR is frequently mistaken for ventricular tachycardia since both have wide, regular complexes and can have signs of atrioventricular dissociation (eg, fusion and/or capture beats), especially when only viewed from the telemetry monitor. The feature that distinguishes the two rhythms is the rate:
- AIVR occurs at a rate between 50 and 110 beats/min; rates less than 50 beats/min are consistent with ventricular escape
- Ventricular tachycardia most commonly has a rate greater than 110 beats/min
Fusion and capture beats occur when a sinus-generated beat either fuses with a ventricular complex or gets conducted through the normal pathway, respectively. They suggest atrioventricular dissociation and can be seen in both AIVR and ventricular tachycardia. The distinction between AIVR and ventricular tachycardia is of paramount importance since the management differs significantly.
AIVR is a self-terminating and well-tolerated rhythm that does not require intervention, unlike ventricular tachycardia.3 However, the underlying etiology should be explored. Antiarrhythmics should be avoided due to possible hemodynamic collapse.4
In a patient presenting with AIVR and signs or symptoms consistent with acute coronary syndrome, as with our patient, spontaneous reperfusion of an unstable coronary plaque should be assumed, and the patient should immediately be transferred to a percutaneous coronary intervention-capable (PCI-capable) facility.
The patient here was found to have an anterolateral ST-elevation myocardial infarction on a subsequent ECG (Figure 2), and he was immediately transferred for PCI.
Learnings/What to Look for
- AIVR is a wide, regular rhythm with a rate between 50 and 110 beats/minute
- Capture or fusion beats suggest atrioventricular dissociation and can be seen with AIVR or ventricular tachycardia
Pearls for Urgent Care Management
- In most cases, AIVR represents reperfusion, often after thrombolysis.
- Patients with AIVR should be transferred to a PCI-capable center
- Antiarrhythmics traditionally given in ventricular tachycardia should be avoided due to possible hemodynamic collapse
- Evaluate for other underlying causes, such as electrolyte abnormalities, severe cardiomyopathies, or drug toxicities
References
- Surawicz B, Knilans TK. Chou’s Electrocardiography in Clincal Practice. 6th ed. Philadelphia, PA: Elsevier; 2008.
- Mattu A, Tabas J, Brady W. Electrocardiography in Emergency, Acute, and Critical Care. 2nd ed. Dallas, TX: The American College of Emergency Physicians; 2019.
- Riera ARP, Barros RB, Sousa FD de, Baranchuk A. Accelerated idioventricular rhythm: history and chronology of the main discoveries. Indian Pacing Electrophysiol J. 2010;10(1):40.
- Perron AD, Sweeney T. Arrhythmic complications of acute coronary syndromes. Emerg Med Clin North Am. 2005;23(4):1065-1082.
