Urgent message: Atypical chest pain in a young male offers a challenge solved by ordering—and assessment—of the appropriate imaging.
Shannon Dowler, MD
The patient is a 20-year-old white male who presented to urgent care with a two-week history of mild dyspnea, with the onset of chest pain in the prior 24 hours.
He denied wheezing, vomiting, and recent trauma, and reported that he has tried no medications for his symptoms.
Further discussion with the patient revealed the following:
- pain and pressure with breathing, eating, and swallowing
- minimal cough, but no symptoms indicative of upper respiratory infection
- fatigue, but no fever, chills, or weight loss
- “on and off” lifetime history of shortness of breath that was usually self-resolving

The patient reported that he had never experienced such a severe shortness-of-breath episode, though his chief complaint was chest pain. Besides that, he denied any chronic disease and reported no allergies and no current medication use.
Observations and Findings
The patient is thin, uncomfortable, and anxious, but with no acute distress.
FH: Brother with Wolff Parkinson White syndrome (WPW)
SH: Quit tobacco one year ago. Initially denied use of recreational drugs but later admits to history of prior cocaine use (last used five months ago) and current recreational marijuana use. Denied IV drug use. Physical: t 97.5, BP 110/64, HR 59, RR 20, pulse Ox 99%
CV: Bradycardia with rub left upper sternal border; no previous myocardial infarction, no jugular venous distention Lungs: CTAB without w/r/r; no dyspnea apparent, Abd: benign
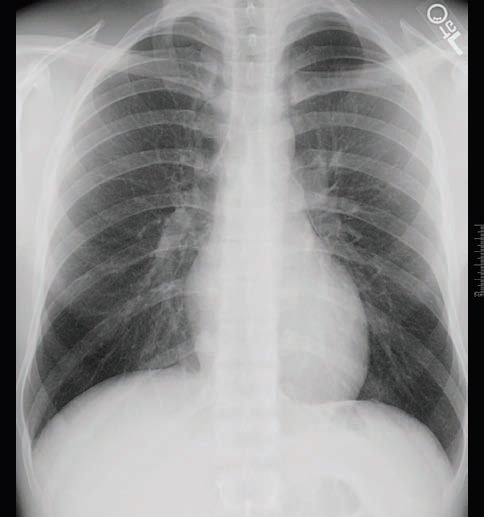
Ext: no LE edema, no evidence of DVT, HEENT: benign, EKG: bradycardia, CXR: free air evident abutting left superior cardiac, border; lungs negative for pneumothorax
Course
The patient was admitted directly to hospital, where a 2D echo was negative for pericarditis or pneumopericardium (Figure 1).
“This case offered the opportunity to investigate a subtle and interesting radiology finding.”
However, a chest CT revealed superior mediastinum air with inferior air tracking along the esophagus (Figure 2); a CT of the neck revealed superior mediastinal air around the upper esophagus, the left lobe of the thyroid, and in prevertebral soft tissues (negative for extravasation of gastrograffin contrast material).
Ultimately, he was discharged with a diagnosis of suspected spontaneous pneumothorax, with extravasation of air into the mediastinum.
Teaching Points
Primary spontaneous pneumothorax is most common in patients with no underlying pulmonary disease, particularly tall, thin males in their 20s. This case offered the opportunity to investigate atypical chest pain presenting in a young male, and to evaluate a subtle and interesting radiology finding.

