Published on
Download the article PDF: Analysis Of Short Course Systemic Glucocorticoid Prescribing In Urgent And Convenient Care Clinics
Urgent Message: Across a tristate urgent care and convenient care network, systemic steroid use occurred in nearly one-sixth of encounters (15.5%)—72.5% for likely avoidable indications and 66% for acute respiratory infections. The finding highlights the need to establish systemic steroid metrics to drive stewardship efforts.
Paul Hansen, MD; Yang Wang, PhD; Muhammad Naseer, MD
Abstract
Background: The College of Urgent Care Medicine released a position statement advocating for corticosteroid stewardship best practices in 2022, but the extent of avoidable systemic short-course glucocorticoid (SSCG) use in urgent or convenient care clinics is unknown.
Methods: Using data from the electronic medical record, a cross-sectional analysis of in-person or video telehealth encounters occurring from July 2022 through June 2023 of patients without chronic steroid use aged 3 months and older from 55 urgent or convenient care clinics across Missouri, Oklahoma, and Arkansas was completed. Variables related to encounter diagnoses, patient age and location, clinic type, medication prescribed, and provider degree were analyzed to inform data on SSCG use rate, the SSCG use rate for acute respiratory infections (ARIs), and the estimated SSCG use that was likely avoidable using a tier-based diagnosis schema, with 95% confidence intervals (CI), p-values, and univariate odds ratios (ORs) reported when appropriate.
Results: Of the 586,653 encounters analyzed, 15.5% involved SSCG use, with adult encounters receiving SSCGs more often than pediatric encounters (adult SSCG rate 18.5% vs pediatric SSCG rate 8.4%, OR 2.47, CI 2.42-2.51, p <0.001). It was estimated that approximately 7 in 10 (72.5%, CI 72.2%-72.8%) encounters utilizing SSCGs were likely avoidable based on diagnostic tier assignment. The diagnoses that SSCGs were most frequently utilized for were pharyngitis (14,164 SSCG encounters, SSCG use rate 12.1%), acute sinusitis (8,697 SSCG encounters, SSCG use rate 36.0%), and acute upper respiratory infections (5,574 SSCG encounters, SSCG use rate 23.3%). ARI encounters accounted for 66.0% (CI 65.7-66.3%) of SSCG use and represent 77.7% (CI 77.3-78.0%) of likely avoidable (ie, tier 2 and tier 3) SSCG use. Significant geographic and provider variability was noted.
Conclusions: SSCG use was noted in nearly 1 in 6 encounters in a large network of urgent and convenient care clinics from July 2022 through June 2023, often for avoidable indications and ARIs. This highlights the need for monitoring specific SSCG measures to advance corticosteroid stewardship efforts in the urgent and convenient care setting.
Introduction
While systemic glucocorticoids have numerous evidence-based indications in patients of all ages, they are often used for short courses in clinical scenarios when patient benefit is expected to be minimal or absent. This trend, combined with data from the last decade outlining the potential harms of short courses of systemic corticosteroids, clarifies why steroid stewardship efforts are warranted. Steroids are used with increasing frequency, often when they could be avoided, leading to a risk of avoidable harms beyond well-known risks like hyperglycemia, to include risks such as sepsis and gastrointestinal hemorrhage in adults and children, pneumonia in children, and congestive heart failure, venous thromboembolism and fracture in adults.1,2
In August of 2022, the College of Urgent Care Medicine released a position statement advocating for corticosteroid stewardship best practices for adult and pediatric patients in the urgent care setting.3 However, the fraction of systemic corticosteroid use that is avoidable and therefore amenable to reduction is unknown. To our knowledge, there is no recent analysis of outpatient systemic short-course glucocorticoid (SSCG) use in the COVID-19 era, nor is there an overall estimate of avoidable urgent or convenient care SSCG use that considers adults and pediatrics, all conditions that SSCGs are utilized for, or the fraction of overall SSCG utilization for acute respiratory infections (ARI).
The overarching objective of this study was to establish SSCG baseline use data within a large healthcare system, which could inform how best to enact systemic steroid stewardship efforts in urgent and convenient care clinics. Specifically, we sought to establish a baseline of SSCG use rate overall per 100 encounters, by age and diagnoses, to estimate the rate of potentially avoidable SSCG use per 100 encounters and report the percentage of SSCG use for ARIs. We further examined SSCG use based on additional patient, prescriber, and clinic variables outlined below, along with a duration analysis to inform the duration definition for SSCG use in this care setting.
Methods
Study Design, Data Sources, and Study Population
This was a retrospective cross-sectional analysis of in-person and video-telehealth encounters of patients aged 3 months and older occurring at any of the 47 urgent care and 8 convenient care clinics within a large healthcare system across Missouri, Oklahoma, and Arkansas from July 1, 2022, through June 30, 2023. The data source utilized was the electronic medical record (EMR) of our healthcare system (Epic, Madison, Wisconsin), which is integrated across our hospitals and clinics. Encounters not fulfilling the inclusion criteria (eg, orders only or x-ray imaging) or encounters with missing diagnosis data were not included in the dataset. Additional encounters were excluded if they involved a patient with chronic steroid use, defined as any current or previous prescription within the 365 days prior to the index encounter where a supply of 30 days or more was provided for a systemic glucocorticoid, or if an intraarticular steroid injection was administered without concurrent systemic glucocorticoid use. The Mercy Institutional Review Board reviewed the study protocol and determined it met exemption criteria. This study adheres to the Strengthening the Reporting of Observational Studies in Epidemiology recommendations.
SSCG use was defined as an outpatient prescription for or an in-clinic administration of a systemic (ie, oral [PO], intravenous [IV], or intramuscular [IM]) glucocorticoid of less than 30 days duration. Duration of SSCGs was determined from data within the medication order; duration data was utilized when available, and amount of medication dispensed combined with directions for use was utilized to determine the duration (when duration data was unavailable). Glucocorticoids prescribed or administered via non-systemic routes, such as inhaled, topical, intranasal, or ophthalmic were excluded.
Estimating Avoidable Steroid Use
As our healthcare system’s EMR does not require links between diagnoses and medication prescriptions, urgent or convenient care visit diagnoses were classified based on the most likely indication for SSCG use in a tiered fashion, modeled after existing antibiotic stewardship methods.4 Given the clinical versatility of SSCGs, a diagnostic categorization scheme was created that aims to be both comprehensive and nuanced, based on clinical judgment of the lead author. Only perinatal diagnoses codes were not categorized given age restrictions within our study patient population.
- Tier 1 diagnoses were diagnoses for which SSCGs are often indicated as the expected benefits commonly outweigh the risk of harm in the urgent or convenient care setting: asthma, chronic obstructive pulmonary disease (COPD) or gout exacerbations, autoimmune or rheumatologic conditions, contact dermatitis, etc.
- Tier 2 diagnoses were diagnoses for which SSCGs may be indicated in other care settings (eg, inpatient) or depending on the specific clinical circumstance but are usually avoidable in the urgent or convenient care setting: pneumonia, COVID-19, pharyngitis, etc.
- Tier 3 diagnoses were all other diagnoses for which use of SSCGs were avoidable regardless of care setting, where the risk of harm is expected to outweigh the potential benefit, or the indication is unclear given a lack of supporting evidence of guidance: acute upper respiratory infection, bronchitis, non-radicular low back pain, etc.
In assigning each visit a single diagnosis for tier assignment, priority was given to tier 1 diagnoses, then tier 2 diagnoses, then tier 3 diagnoses. If a visit contained multiple diagnoses from a single tier, the first-listed diagnosis was assigned.
Acute Respiratory Infection
Independent of the tier-schema-assigned single encounter diagnosis described above, all encounter diagnoses were screened for ARI diagnoses. While the definition of ARI utilized for this study has been previously defined,5 the subgroupings were modified to fit within the above-described tier schema. Eligible ARI diagnoses included bronchitis, pneumonia, otitis media and other ear complaints, sinusitis, pharyngitis, influenza, COVID-19, croup, cough, laryngitis, and other acute upper or lower respiratory tract infections.
Other Variables
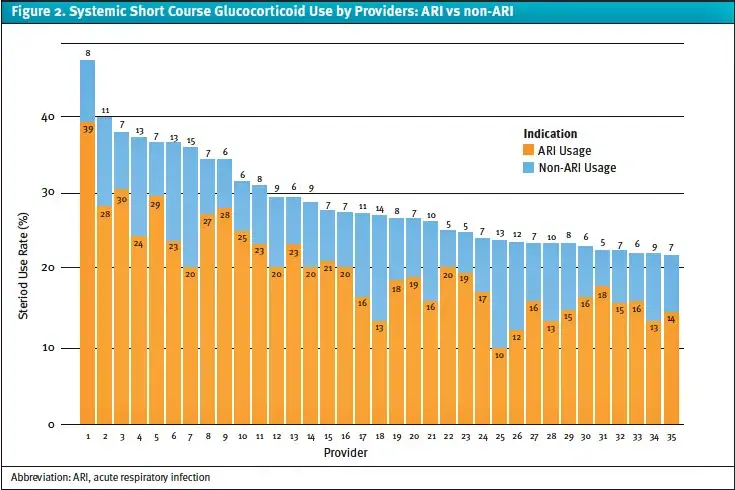
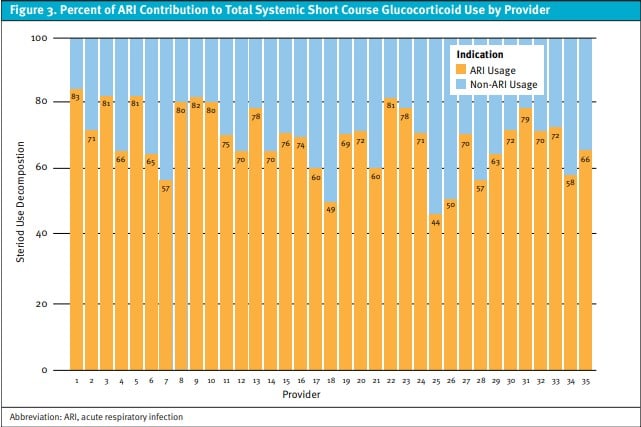
Patient age was categorized by National Institutes of Health recommended age groups (3 months-1 year; 1-12 years, 13-17 years, 18-64 years, ≥65 years)6 with larger groupings reported to summarize pediatrics (3 months-17 years) and adults (18 years or older). Patient variables analyzed in addition to age included biologic sex, state, and ZIP code. Clinic data was categorized into either urgent or convenient care clinics. Ordering provider data was analyzed by provider type (physician, nurse practitioner, or physician assistant), SSCG use quartile among providers with at least 100 encounters, and a selected analysis of the 35 providers with 100 or more encounters who had the highest overall SSCG use rates reported by what percentage of their total use included use in ARI encounters to provide detail on variability of ordering provider use patterns. SSCG variables included systemic glucocorticoid utilized, route of administration, and prescription duration.
Statistical Methods
Statistical analyses were performed using R (version 4.4.0) and Python. The overall, tier-based, and ARI-related diagnostic mean rates of SSCG per 100 patient encounters were calculated and analyzed based on the above pre-specified variables (age, gender, etc.). Except for the prespecified ARI group and its subgroupings of diagnoses, diagnoses were grouped based on the individual categorizations outlined in the tiering schema. Descriptive statistics, including proportions and means, were used to summarize encounter characteristics and SSCG utilization across tiers 1 through 3 and ARI diagnoses. For inferential analyses, univariate logistic regression was used to estimate odds ratios (ORs) between groups, along with corresponding 95% confidence intervals (CIs) and p-values to determine statistical significance. When 95% CIs are presented without accompanying p-values, they were calculated using the Wilson score interval. Subgroup analyses were conducted to examine variations in SSCG use across patient age groups, provider types (physicians, nurse practitioners, and physician assistants), clinical settings (urgent vs convenient care), gender (male vs female), and patient states (Missouri, Oklahoma, and Arkansas). Missing data were not handled using complete case analysis; records were included in each analysis if complete data was available for the variables used in that specific model.
Results
There were 616,551 urgent or convenient care encounters involving 419,870 patients. A total of 29,898 encounters from 15,619 patients were excluded, all due to chronic steroid use, leaving 586,653 encounters (87.9% occurring in the urgent care setting) from 404,251 eligible patients (mean age 34 years; female 60.0%). Analysis shows 20.1% of patients received SSCGs from an urgent or convenient care encounter during the study period, which equaled a SSCG encounter rate of 15.6%. SSCG use rates were similar in urgent and convenient care clinics (convenient care OR 0.99, CI 0.97-1.01, p=0.198). Prednisone was the most common SSCG utilized, followed by methylprednisolone, dexamethasone, and triamcinolone (58.8%, 25.5%, 13.0%, and 2.7%), respectively. PO administration was the most common route utilized (79.6% PO, 20.3% IM, 0.03% IV). Among adults, SSCG course median duration was 7 days, with a 5-10 day interquartile range. Extended courses beyond 14 days were uncommon, occurring in only 2.9% of total SSCGs ordered.
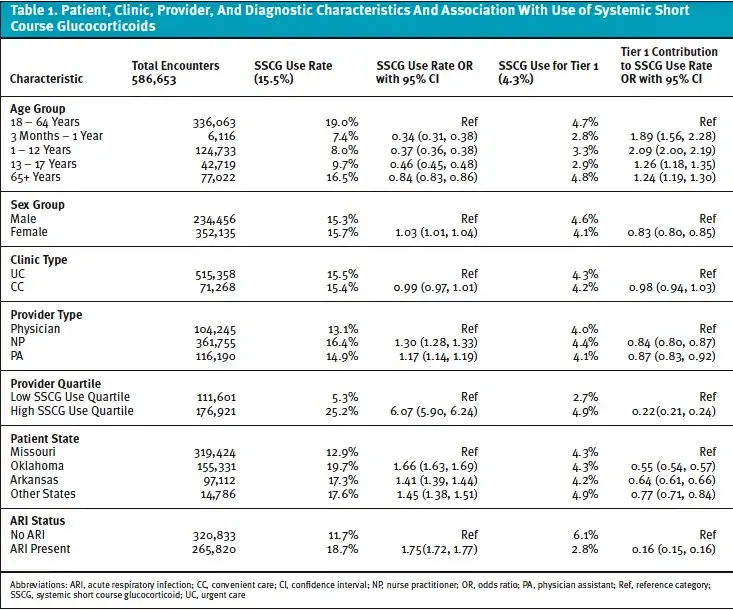
SSCG use varied significantly by age groupings: 8.4% of pediatric (age 3 months through 17 years) encounters vs 18.5% of adult (age 18 years or greater) encounters utilized SSCGs (adult vs pediatric OR 2.47, CI 2.42 – 2.51, p<0.001). Variations noted within each age grouping are summarized in Table 1 with the highest SSCG use rate noted in adults aged 18-64 years (19.0%) and the lowest SSCG use rate noted in patients aged 3 months through 1 year (SSCG use rate 7.4%, OR 0.34, CI 0.31-0.38, p<0.001). Compared with male patients, female patients were slightly more likely to receive SSCGs (OR 1.03, CI 1.01-1.04, p<0.001).
Geographic Variability
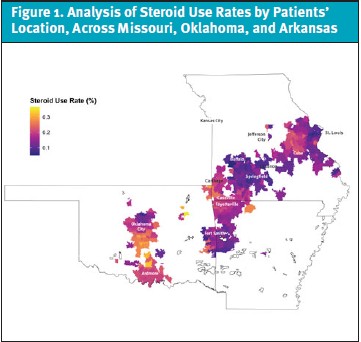
We found significant geographic variability. When analyzing data by state, Oklahoma residents’ encounters were 53% more likely (OR 1.66, CI 1.63-1.69, p<0.001) to involve SSCGs than Missouri residents’ encounters. Intrastate geographic variations in SSCG use were more pronounced when analyzed by patient ZIP code (Figure 1). When comparing the highest and lowest SSCG use rates within a state by patient ZIP code, we found a nearly fourfold higher odds variation of SSCG use within Arkansas (OR 3.73, 95% CI 1.80–7.69, p<0.001), and greater than sevenfold higher odds variation within Missouri (OR 7.58, 95% CI, 2.3–25.0, p<0.001) and Oklahoma (OR 7.87, 95% CI 2.14–28.90, p=0.002).
Steroid Use Rate by Diagnoses and Tier
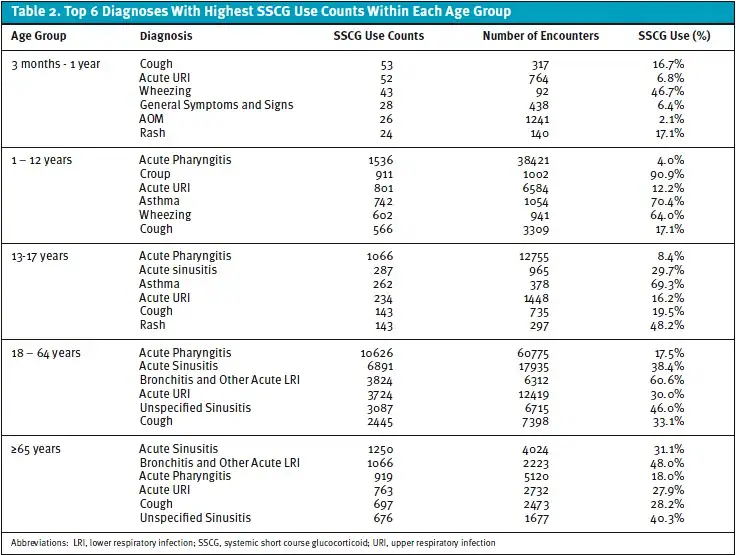
The top 3 diagnoses with 100 or more encounters associated with the highest SSCG use rates were croup (SSCG use rate 90.3%), contact dermatitis (SSCG use rate 80.4%), and anaphylaxis or allergic reaction diagnoses (ie, adverse events not elsewhere classified, SSCG use rate 76.2%), all of which are tier 1 diagnoses. However, when ranking the top 3 diagnoses by total SSCG use encounters, SSCGs were most frequently utilized for likely avoidable (tier 2 or 3) indications involving ARIs: pharyngitis (tier 2, 14,164 SSCG encounters, use rate 12.1%), acute sinusitis (tier 2, 8,697 SSCG encounters, use rate 36.0%), and acute upper respiratory infections (tier 3, 5,574 SSCG encounters, use rate 23.3%). Common indications for SSCGs varied by age grouping, as summarized in Table 2.
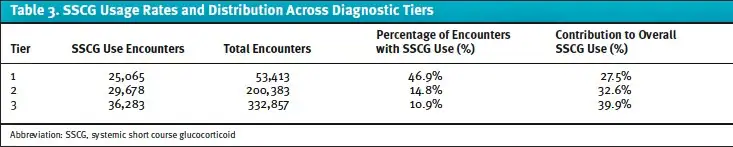
SSCG use rates and distribution across diagnostic tiers are summarized in Table 3. As expected, tier 1 encounters had the highest SSCG use rate (46.9%, CI 46.5%-47.4%). However, it only accounted for 27.5% of overall SSCG use, suggesting more than 7 in 10 (72.5%, CI 72.2%-72.8%) encounters utilizing SSCGs were likely avoidable (tier 2 32.6%, CI 32.3%-32.9% and tier 3 39.9%, CI 39.5%-40.2%).
Acute Respiratory Infections
ARI encounters were treated with SSCGs 18.7% of the time vs 11.7% for non-ARI encounters (OR 1.75, CI 1.72–1.77, p<0.001). As shown in Table 1, only 2.75 percentage points of the total 18.7% SSCG use for ARI encounters were for tier 1 indications, compared to 6.1 percentage points of the total 11.7% SSCG use for non-ARI encounters. The odds ratio for tier 1 contribution to total steroid use in ARI encounters was 0.16 (CI 0.15–0.16, p<0.001), indicating that SSCG use in ARI encounters was more likely to be avoidable. ARI encounters accounted for 66.0% (CI 65.7-66.3%) of SSCG use and represent 77.7% (CI 77.3-78.0%) of all non-tier 1 SSCG use (tier 2 89.1% [CI 88.7-89.4%] and tier 3 68.3% [CI 67.9-68.8%]).
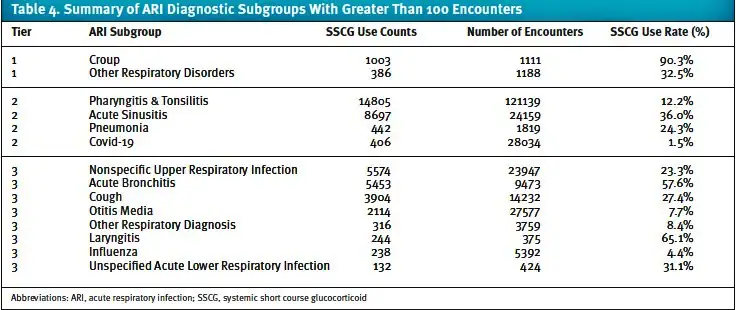
SSCG rates by tier assigned diagnoses for croup, pharyngitis, sinusitis, and URIs were previously discussed. As noted in Table 4, the SSCG use rates for many ARI diagnoses from tier 2 or 3 neared or exceeded 25%. Laryngitis and bronchitis were treated with SSCGs more than half of the time (laryngitis rate 65.1%, CI 60.1-69.7% and bronchitis rate 57.6%, CI 56.6-58.6%), while other lower acute respiratory infections, cough, and pneumonia, received SSCGs 31.1% (CI 26.9-35.7%), 27.4% (CI 26.7-28.2%), and 24.3% (CI 22.4-26.3%), respectively. Conversely, only other respiratory diagnoses, (rate 8.4%, CI 7.6 – 9.3%), otitis media (rate 7.7%, CI 7.4 – 8.0%), influenza (rate 4.4%, CI 3.9-5.0%), and COVID-19 (rate 1.5%, CI 1.3-1.6%) had SSCG use rates below 10%.
Provider Analysis
Compared to physicians, nurse practitioners (NPs) had 30% higher odds (OR 1.30, CI 1.28–1.33, p<0.001) and physician assistants (PAs) 17% higher odds (OR 1.17, CI 1.14-1.19, p<0.001) to utilize SSCGs. This trend was also observed in SSCG use rates for ARI encounters, which were 15.2%, 19.1% (OR 1.32, CI 1.28-1.36, p<0.001), and 19.7% (OR 1.37, CI 1.33-1.40, p<0.001) for physicians, PAs, and NPs, respectively. Tier analysis revealed that tier 1 use contributed a larger percentage of overall SSCG use for physicians than their advanced practice provider (APP) colleagues. Tier 1 SSCG use was 30.5%, 27.7% (OR 0.87, CI 0.83,0.92, p<0.001), and 26.8% (0.84, CI 0.80-0.87, p<0.001) for physicians, PAs and NPs, respectively.
After excluding providers with fewer than 100 encounters, comparing providers in the upper vs lower quartile of SSCG use rates revealed striking differences. Odds that an encounter involving providers in the highest quartile of SSCG use were 6 times higher that SSCG would be used than their peers in the lowest quartile (25.2% vs 5.3% OR 6.07, CI 5.90-6.24, p<0.001). Providers in the highest SSCG use quartile accounted for 30.4% of the total encounter volume within the study yet were responsible for nearly half (49.3%, CI 49.0-49.6%) of the SSCG use. Tier analysis shows that tier 1 use accounted for more than half (52.0%) of the overall SSCG use among providers in the lowest SSCG use quartile vs only 19.4% (OR 0.22, CI 0.21-0.24, p<0.001) of the SSCGs in the highest use quartile. Analysis of individual providers with at least 100 encounters revealed the highest SSCG use rate noted was 46.4%. Additionally, 21 of the 277 providers with 100 or more encounters had SSCG use rates exceeding 25%. Among the 35 providers with the highest SSCG use rates, the proportion of SSCG use associated with ARI encounters ranged from 44.2-83.3% (Figure 2,3).
Discussion
This study describes SSCG use during urgent care and convenient care visits in a large healthcare system from July 2022 through June 2023. This is the first study to focus on SSCG use in the urgent or convenient care setting or to describe SSCG use since the COVID-19 pandemic. Overall, nearly 1 in 6 (15.5%) of these visits were associated with SSCG use, with higher rates seen in adult vs pediatric age groups and slightly higher rates seen in female vs male patients. The majority were likely avoidable based on tier-assigned (tier 2 or tier 3) diagnostic indication. Widespread, increasing SSCG use for avoidable indications has been suggested in several previous publications from locations throughout the world.1-2,7-8 In a U.S. nationwide study of steroid use in acute respiratory tract infections (ARTIs) from 2007 through 2016, the systemic steroid use rate increased from 10.5% to 16.3%, with urgent care clinics identified as the care setting with the highest use rate.9 While that study also noted a higher steroid use rate for ARTIs in urgent care vs walk-in retail clinics, we did not note a similar difference in urgent vs convenient care clinics’ overall SSCG use within our healthcare system. This may be due to differences in walk-in retail clinics (where care may be driven by standing treatment protocols) vs convenient care clinics in our healthcare system—which primarily differ from our urgent care clinics by a lack of on-site x-ray.
In our analysis, children received SSCGs less than half as often as adults. This relative reduction in SSCG use for pediatric patients appeared roughly consistent for ARI and non-ARI encounters. Furthermore, when SSCGs were utilized for pediatric patients, they were more commonly used for tier 1 indications—a trend that was stronger in our younger age brackets relative to adolescents (Table 1). This differs from previous literature where use rates were similar between adult and pediatric patients.1-2 The etiology for this difference is unknown. It may be that acute care providers are more cautious to utilize SSCGs in younger children unless indicated given concerns pediatric adverse effects.10, 11 The reasons behind the differential SSCG use rate warrant further exploration, as it may inform how to best tailor provider education on corticosteroid stewardship efforts.
We utilized a tier schema for SSCG use similar to existing tier categorizations for antibiotic use; however, the expected and appropriate use rates by tier are significantly different given key distinctions. First, we note that the determination of whether a SSCG is avoidable for both tier 1 and tier 2 indications may rely on severity of presentation not captured in diagnosis data more so than antibiotic tier categorizations. As an example, for tier 1 antibiotic indications (eg, non-viral pneumonia, pertussis, urinary tract infection, syphilis), the expected antibiotic use rate would approach 100%,4 whereas the SSCG use rates for tier 1 encounters (46.9% overall, 54.8% and 30.7% for providers in the highest and lowest SSCG use quartiles, respectively) was much lower. This highlights that, although tier 1 SSCG use was likely appropriate for these indications, it does not necessarily mean that all tier 1 SSCG use was unavoidable. This assumption likely results in underestimation of avoidable SSCG use for certain tier 1 indications such as contact dermatitis, which may be amenable to topical rather than systemic therapy, or acute gout exacerbation, which can also be treated with non-steroidal anti-inflammatory drugs (NSAIDs) or colchicine. Second, we utilized a simplified approach relative to existing 3-tier antibiotic schema: tier 1 SSCG use was deemed likely appropriate, whereas tier 2 or 3 SSCG use was likely avoidable. While it is true that a small percentage of the tier 2 SSCG use may have been appropriate on a case-by-case basis (eg, severe pharyngitis), most tier 2 SSCG use observed was likely avoidable in the urgent or convenient care setting. This assumption means that the estimated inappropriate antibiotic use rates for tier 2 antibiotic indications such as sinusitis, pharyngitis, and acute otitis media would be much lower than the expected avoidable SSCG use for tier 2 SSCG indications in the urgent or convenient care setting.
Regarding the optimal definition for SSCG use, our study utilized a duration of less than 30 days, as variable durations from 14-30 days have been noted in the literature.1,2,8,12 Our data indicates that a duration of 14 or fewer days captures greater than 97% of SSCG use in urgent or convenient care clinics within our healthcare system. Though this data may be useful for future research, healthcare systems or clinics interested in implementing corticosteroid stewardship efforts would need to recognize that inclusion of any steroid duration cap within the definition of a potential corticosteroid stewardship metric may inadvertently lead to longer steroid courses than indicated.
The variable practice patterns we observed in our geographic and provider analyses, which were similar to a previously published nationwide analysis on systemic steroid use for ARTIs in the United States from 2007 through 2016,9 suggest that patient expectations and local culture likely play a role in noted regional differences, as does provider training. Similar to previous studies, urgent or convenient care visits among patients living in Oklahoma were 53% more likely to have SSCGs utilized vs visits in Missouri, with more pronounced local geographic differences noted on intra-state patient ZIP code analysis.
Likewise, our analysis of urgent and convenient care APPs also found a similar provider type trend. In our analysis, APPs had higher SSCG use rates and utilized SSCGs more often for non-tier 1 indications than physicians, a trend that is very similar to available data on systemic steroid use for ARTIs9 and antibiotic use.13 It is important to highlight that the differing medication use rates by provider training seen in our study and others9,13 are expected to have a larger impact in the urgent and convenient care clinics given the typical medical provider staffing ratios utilized in these care settings. In our study, APPs accounted for just over 80% of the total patient encounters. The data suggests that educational interventions for medication stewardship may be more impactful if specific content is tailored to APPs, and that opportunities exist to support APP participation and leadership within medication stewardship programs in this APP-predominant care setting.
While patient age, geographic variability, and provider training may all impact SSCG use, one of the strongest predictors of SSCG overuse appears to be the individual provider’s practice pattern. As noted, the highest SSCG rate noted by an individual provider neared SSCG use for nearly half (46.4%) of that provider’s 4,561 encounters. Among the 277 providers with at least 100 encounters, the 5 providers with the highest SSCG rates accounted for just over 10% of all the SSCG use noted within our study of over half a million patient encounters. This striking variability in provider practice patterns noted in our study, while not unique to SSCGs,14 highlights why it is important to monitor SSCG use at the individual provider level, as it allows for SSCG overuse to be appropriately identified and addressed via targeted educational efforts.
A substantial amount of SSCG overuse was driven by use in ARI encounters. With the notable exception of croup in pediatric patients—where a SSCG such as a single dose of dexamethasone is the first line treatment given evidence of reduction in symptoms and the rate of return visits15—there is very little evidence supporting the routine use of SSCGs for ARIs, and their use in outpatients is not routinely recommended by clinical guidelines. For pharyngitis, which accounted for 15.5% of SSCGs utilized in our study, data have shown that SSCGs may shorten the duration of this self-limited illness by about 11 hours.16 Given the limited expected benefit and inconclusive benefit to harm ratio, most major organizations do not recommend the routine use of SSCGs.3,17-19 Similarly, minimal benefit of SSCGs in acute sinusitis seen in studies may be attributable to attrition bias or secondary care settings in which the studies were performed.20 Acute sinusitis clinical practice guidelines (CPG) recommend intranasal corticosteroids rather than SSCGs.21, 22 For pneumonia and COVID-19, while SSCGs may be indicated for patients with severe illness requiring inpatient level care, they are not indicated for outpatients.23-29 Moreover, although SSCG use for tier 3 ARIs was common, the research and guidelines available for bronchitis,30 laryngitis,31 otitis media,32 URIs,33 and influenza34 recommend against SSCG use.
Our data on SSCG use stratified by tier based diagnostic indication vs SSCG use in ARI encounters may inform future corticosteroid stewardship clinical quality metrics needed to advance steroid stewardship efforts. As an example, for our healthcare system’s network of urgent and convenient care clinics, an approach that focused solely on reducing SSCG use in ARIs would identify most opportunities to reduce avoidable steroid use but would have missed more than 1 in 5 (or 14,731 encounters) opportunities for improvement. However, understanding that the level of support will vary by institution and that SSCG use for ARI varies considerably by geographic location, we would recommend collecting baseline data of SSCG use rates overall and for ARI encounters then utilizing that data to implement a corticosteroid stewardship program that excludes tier 1 diagnoses.
Limitations
Our study has important limitations to consider. First, though our sample size is robust, it is limited to urgent or convenient care clinics located in 3 states and may not be generalizable to other geographic locations, given the known geographic variations.9 Second, while some may view the limited exclusion criteria as a limitation, we felt that limited exclusions provide a fuller picture of how SSCGs are being used in this setting and controlled against selection bias. Third, our analysis did not consider all covariates that may impact SSCG use or severity of illness data, which could further inform whether the SSCG use was appropriate. A covariate warranting further analysis in future studies is SSCG use in video telehealth vs in-person encounters. Fourth, the lack of a diagnostic indication requirement for all medication orders in our electronic medical record means that, despite our best efforts to infer the diagnostic indication in the tiered fashion described, our analyses are at risk for misclassification bias and may be limited by a lack of diagnostic specificity. Fifth, the tier schema developed for this study, which, to our knowledge, is a novel approach for SSCG analysis, was created by the lead author rather than a clinical consensus. Sixth, the limitations of our method to estimate the percentage of avoidable SSCG use based on tiered categories discussed previously likely result in offsetting errors in our estimation. Finally, the design of our study did not seek to identify SSCG overuse by other means, namely dose or duration analysis by diagnostic indication, or SSCGs ordered outside of urgent or convenient care encounter types meeting inclusion criteria, which likely results in further underestimation of SSCG overuse.
Despite these limitations, our findings that SSCGs were utilized in 18.5% of adult and 8.4% of pediatric urgent or convenient care encounters from July 2022 through June 2023 in a large healthcare system, and that approximately 7 in 10 of the SSCGs used may have been avoidable, highlight the need to establish specific SSCG measures to advance corticosteroid stewardship efforts in the urgent and convenient care setting.
View the Supplementary Material
Manuscript submitted April 15, 2025; accepted July 17, 2025.
References
- Yao TC, Huang YW, Chang SM, Tsai SY, Wu AC, Tsai HJ. Association Between Oral Corticosteroid Bursts and Severe Adverse Events : A Nationwide Population-Based Cohort Study. Ann Intern Med. 2020;173(5):325-330. doi:10.7326/M20-0432
- Yao T, Wang J, Chang S, et al. Association of Oral Corticosteroid Bursts With Severe Adverse Events in Children. JAMA Pediatr. 2021;175(7):723–729. doi:10.1001/jamapediatrics.2021.0433
- College of Urgent care Medicine Position Statement: Corticosteroid Stewardship. Published 2022 Aug 18. Accessed March 25, 2025.
- Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011. JAMA. 2016;315(17):1864–1873. doi:10.1001/jama.2016.4151
- Develop and Improve Antibiotic Stewardship Activities in Your Practice. Content last reviewed October 2022. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/antibiotic-use/ambulatory-care/improve/index.htm. Accessed March 25, 2025.
- National Institutes of Health. NIH Style Guide: Age. National Institutes of Health website. https://www.nih.gov/nih-style-guide/age. Accessed March 31, 2025.
- Bénard-Laribière A, Pariente A, Pambrun E, Bégaud B, Fardet L, Noize P. Prevalence and prescription patterns of oral glucocorticoids in adults: a retrospective cross-sectional and cohort analysis in France. BMJ Open. 2017;7(7):e015905. Published 2017 Jul 31. doi:10.1136/bmjopen-2017-015905
- Waljee A K, Rogers M A M, Lin P, Singal A G, Stein J D, Marks R M, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ. 2017;357:j1415 doi:10.1136/bmj.j1415
- Lin KJ, Dvorin E, Kesselheim AS. Prescribing systemic steroids for acute respiratory tract infections in United States outpatient settings: A nationwide population-based cohort study. PLoS Med. 2020 Mar 31;17(3):e1003058. doi: 10.1371/journal.pmed.1003058.
- Wolthers OD, Pedersen S. Short term linear growth in asthmatic children during treatment with prednisolone. BMJ. 1990 Jul 21;301(6744):145-8. doi: 10.1136/bmj.301.6744.145. PMID: 2202451; PMCID: PMC1663512.
- Fuhlbrigge AL, Kelly HW. Inhaled corticosteroids in children: effects on bone mineral density and growth. Lancet Respir Med. 2014 Jun;2(6):487-96. doi: 10.1016/S2213-2600(14)70024-4. Epub 2014 Apr 8. PMID: 24717638.
- Head K, Chong L, Hopkins C, Philpott C, Burton MJ, Schilder AGM. Short-course oral steroids alone for chronic rhinosinusitis. Cochrane Database of Systematic Reviews. 2016, Issue 4. Art. No.: CD011991. DOI: 10.1002/14651858.CD011991.pub2
- Hersh AL, Shapiro DJ, Sanchez GV, Hicks LA. Comparison of antibiotic prescribing between physicians and advanced practice clinicians. Infection Control & Hospital Epidemiology. 2024;45(1):117-119. doi:10.1017/ice.2023.175
- Shively NRBuehrle DJ, Clancy CJ, Decker BK 2018. Prevalence of Inappropriate Antibiotic Prescribing in Primary Care Clinics within a Veterans Affairs Health Care System. Antimicrob Agents Chemother. 62:10.1128/aac.00337-18. https://doi.org/10.1128/aac.00337-18
- Aregbesola A, Tam CM, Kothari A, Le M-L, Ragheb M, Klassen TP. Glucocorticoids for croup in children. Cochrane Database of Systematic Reviews 2023, Issue 1. Art. No.: CD001955. DOI: 10.1002/14651858.CD001955.pub5.
- Aertgeerts B, Agoritsas T, Siemieniuk R A C, Burgers J, Bekkering G E, Merglen A et al. Corticosteroids for sore throat: a clinical practice guideline BMJ. 2017; 358 :j4090 doi:10.1136/bmj.j4090
- de Cassan S, Thompson MJ, Perera R, Glasziou PP, Del Mar CB, Heneghan CJ, Hayward G. Corticosteroids as standalone or add-on treatment for sore throat. Cochrane Database of Systematic Reviews. 2020, Issue 5. Art. No.: CD008268. DOI: 10.1002/14651858.CD008268.pub3.
- Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55(10):e86-e102. doi:10.1093/cid/cis629
- Centers for Disease Control and Prevention. Clinical Guidance for Group A Streptococcal Pharyngitis. 2024. Available from: https://www.cdc.gov/group-a-strep/hcp/clinical-guidance/strep-throat.html. Accessed March 27, 2025.
- Venekamp RP, Thompson MJ, Hayward G, Heneghan CJ, Del Mar CB, Perera R, Glasziou PP, Rovers MM. Systemic corticosteroids for acute sinusitis. Cochrane Database of Systematic Reviews 2014, Issue 3. Art. No.: CD008115. DOI: 10.1002/14651858.CD008115.pub3. Accessed 31 March 2025.
- Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72-e112. doi:10.1093/cid/cis370
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update). Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1-S43. doi:10.1177/0194599815574247
- Dequin PF, Meziani F, Quenot JP, et al; CRICS-TriGGERSep Network. Hydrocortisone in severe community-acquired pneumonia. N Engl J Med. 2023;388(21):1931-1941. doi:10.1056/NEJMoa2215145.
- RECOVERY Collaborative Group, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021 Feb 25;384(8):693-704. doi: 10.1056/NEJMoa2021436. Epub 2020 Jul 17.
- Stern A, Skalsky K, Avni T, Carrara E, Leibovici L, Paul M. Corticosteroids for pneumonia. Cochrane Database of Systematic Reviews 2017, Issue 12. Art. No.: CD007720. DOI: 10.1002/14651858.CD007720.pub3. Accessed 31 March 2025.
- Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, Cooley LA, Dean NC, Fine MJ, Flanders SA, Griffin MR, Metersky ML, Musher DM, Restrepo MI, Whitney CG. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67. doi: 10.1164/rccm.201908-1581ST. PMID: 31573350; PMCID: PMC6812437.
- Bhimraj A, Morgan RL, Shumaker AH, Lavergne V, Baden L, Cheng VC, Edwards KM, Gandhi R, Muller WJ, O’Horo JC, Shoham S, Murad MH, Mustafa RA, Sultan S, Falck-Ytter Y. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Clin Infect Dis. 2020 Apr 27:ciaa478. doi: 10.1093/cid/ciaa478. Epub ahead of print. PMID: 32338708; PMCID: PMC7197612.
- Bradley MC, Perez-Vilar S, Chillarige Y, et al. Systemic Corticosteroid Use for COVID-19 in US Outpatient Settings From April 2020 to August 2021. JAMA. 2022;327(20):2015–2018. doi:10.1001/jama.2022.4877
- Centers for Disease Control and Prevention. Updated Information on Availability and Use of Treatments for Outpatients with Mild to Moderate COVID-19 Who are at Increased Risk for Severe Outcomes of Covid-19. CDCHAN-00463. Accessed March 27, 2025.
- Hay AD, Little P, Harnden A, et al. Effect of Oral Prednisolone on Symptom Duration and Severity in Nonasthmatic Adults With Acute Lower Respiratory Tract Infection: A Randomized Clinical Trial. JAMA. 2017;318(8):721–730. doi:10.1001/jama.2017.10572
- Stachler RJ, Francis DO, Schwartz SR, et al. Clinical practice guideline: hoarseness (dysphonia) (update). Otolaryngol Head Neck Surg. 2018;158(1_suppl):S1-S42. doi:10.1177/0194599817751030
- Hayward G, Thompson MJ, Perera R, Del Mar CB, Glasziou PP, Heneghan CJ. Corticosteroids for the common cold. Cochrane Database of Systematic Reviews 2015, Issue 10. Art. No.: CD008116. DOI: 10.1002/14651858.CD008116.pub3
- Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical practice guideline: otitis media with effusion (update). Otolaryngol Head Neck Surg. 2016;154(1_suppl):S1-S41. doi:10.1177/0194599815623467
- Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis. 2019;68(6):e1-e47. doi:10.1093/cid/ciy866
Author Affiliations: Paul Hansen, MD, Mercy GoHealth Urgent Cares, St. Louis, Missouri. Yang Wang, PhD, Mercy Health, St. Louis, Missouri. Muhammad Naseer, MD, Mercy Hospital, St. Louis, Missouri.

