Published on
Download the article PDF: 2025 19815 20 Ortho Case Report
Urgent Message: Rapid identification of Lisfranc injuries in urgent care is critical, as delays in diagnosis can lead to chronic disability. Most patients with Lisfranc fractures or dislocations should be referred directly to the emergency department. Cross-sectional imaging (ie, computed tomography) and orthopedic consultation are time-sensitive, and urgent operative repair is often indicated.
Alexandra Eby, BS; Nicole Meschbach, MD
Questions for the Urgent Care Clinician at the Bedside
- Which injury patterns and historical features are associated with Lisfranc injuries?
- Can the physical exam reliably differentiate between Lisfranc and other midfoot injuries?
- What radiographic findings are suggestive of Lisfranc injuries?
- Which patients with Lisfranc injuries require operative interventions?
- Which patients with suspected Lisfranc injuries require immediate referral to the emergency department?
Abstract
A Lisfranc injury is a tarsometatarsal fracture and/or dislocation that occurs between the medial cuneiform and base of the second metatarsal. Lisfranc injuries typically occur when there is rotational force and axial loading through a hyper-plantarflexed foot. Rapid identification of a Lisfranc injury is important, as delays in diagnosis can lead to chronic disability. Initial imaging involves plain radiographs (XR) of the foot, but these may be normal in some cases. The priorities for urgent care (UC) management in patients with suspected Lisfranc injuries center around properly identifying the patients at risk for such injuries and prompt referral to an appropriate emergency department (ED) where cross-sectional imaging and orthopedic consultation are available.
Clinical Scenario
A previously healthy 38-year-old man presented to UC an hour after he slipped from a ladder and fell 8 feet (~2.5 meters) onto his left foot. He complained of pain centered at the midfoot, which was worse with movement and attempts at weight-bearing. There was minimal associated numbness. A primary and secondary survey indicated the foot trauma was an isolated injury.

On examination, the patient had normal vital signs and appeared relatively comfortable at rest. He had a severely antalgic gait and difficulty bearing any weight on the left foot. There was no ecchymosis of the foot, but there was swelling over the mid-dorsal aspect of the foot. There was tenderness to palpation particularly over the proximal aspect of the 2nd metatarsal. The skin was intact, and he had a normal neurovascular exam with sensation and capillary refill similar to the unaffected side. XR was obtained in UC (Image 1).
Discussion
Midfoot fractures overall encompass 0.4% of all adult fractures,[1] but Lisfranc injuries specifically describe a subset of midfoot injuries, representing 0.2% of all fractures.[2] Lisfranc fracture describes only a subset of such midfoot injuries, however, as it is possible to have an entirely ligamentous Lisfranc injury. For the purposes of this article, we will be discussing predominantly bony Lisfranc injuries (ie, fracture-dislocations).
The eponymous condition is named for French physician Jacques Lisfranc (1790-1847) who served in Napoleon’s army as a field surgeon. He described an injury pattern most frequently encountered among calvary soldiers whose foot became entrapped in their stirrups after falling from horses in battle. He also developed a technique for partial foot amputation through the tarsal-metatarsal joint (TMT), which was simpler as a field surgical procedure than cutting directly through bone.[3]
A Lisfranc injury can occur by direct or indirect forces to the foot. Direct injuries generally involve high-energy mechanisms such as car accidents, crush injuries, or falls from height. Indirect mechanisms of injury occur with strong rotational forces, often with a hyper-plantarflexed foot with axial loading, resulting in injury to the TMT joint.[4] High energy mechanisms are not required for Lisfranc injuries to occur. In fact, a study done by Stødle et al. in 2019 showed that low-energy trauma and sports injuries were the most common cause of Lisfranc injury in the population studied.[5] Yu et al. examined 80 patients with a TMT joint fracture-dislocation and found 41% of cases resulted from motor vehicle collisions, 30% involved a fall from a height, and 16% occurred after a crush injury.[6]
Lisfranc injuries may be clinically subtle and as much as 20% of injuries are initially misdiagnosed.[7] Delays in diagnosis have consequence with many patients developing chronic foot pain,[8],[9] and they are commonly missed on the initial XR.5
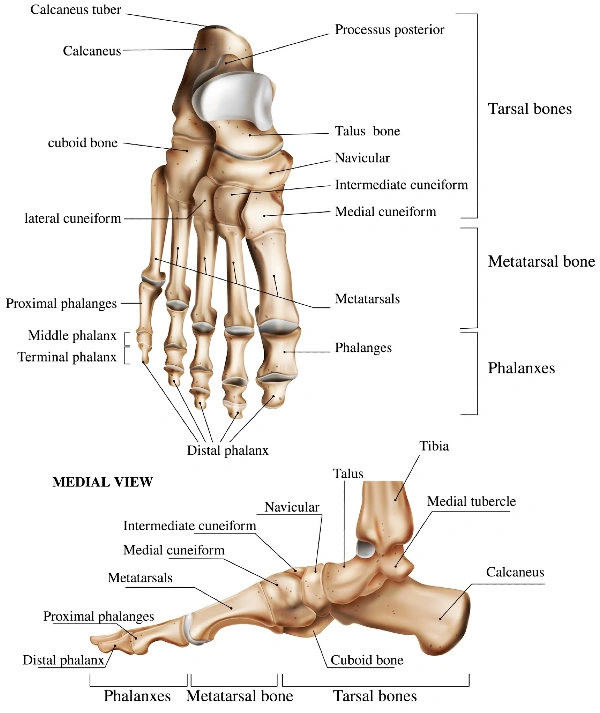
Understanding the Anatomy
The foot is divided into the hind foot (ie, talus and calcaneus), midfoot (the cuneiforms, cuboid, and navicular bone), and the forefoot (involving the proximal aspect of the metatarsals and extending distally through the phalanges). The junction of the midfoot and the forefoot is termed the “Lisfranc joint.”
The Lisfranc joint complex is comprised of (Figure 1):
- Medial, intermediate, and lateral cuneiform
- Cuboid bone
- The base of the 5 metatarsals
Typically, a Lisfranc injury indicates a fracture of 1 of these structural elements. The TMT joint is also held together by a ligamentous capsule structure known as Lisfranc’s ligament, which travels between the base of the second metatarsal and the medial cuneiform. The Lisfranc ligament serves to increase the strength of the joint. This allows for stability of the midfoot and is critical in maintaining the arch of the foot for push off during the gait cycle. The bases of the lateral 4 metatarsals are secured by strong ligaments, however, no transverse ligament exists between the first and second metatarsal bases, thereby creating an area of structural vulnerability.8
History
As with any musculoskeletal injury, begin with inquiry about the mechanism of injury. Lisfranc injury might be considered in cases with midfoot pain after a motor vehicle collision, direct impact, or a fall from height.4 Lisfranc injuries may also occur from seemingly minor mechanisms, such as a twisting motion during sport; in older patients, lower mechanism injuries can result in Lisfranc injuries with relative frequency.[10] Pain from a Lisfranc injury is often severe with attempts at weight-bearing but may be minimal at rest. Many patients with Lisfranc injuries will be entirely unable to bear weight.
Physical Examination
Review the vital signs and the patient’s general appearance. Expose and examine the entire lower leg, from the distal femur to the toes. Palpate for the site of greatest tenderness. If the point of maximal tenderness is at the dorsal midfoot near the TMT joint complex, this should raise suspicion for the possibility of Lisfranc injury. Evaluate for swelling, erythema, ecchymosis, and deformity. Occasionally, bruising may only be evident on the plantar aspect of the foot, so it is important to inspect beyond the dorsum of the foot. Ensure the skin is intact and there is no concern for open fracture. Include an assessment for range of motion of the knee and ankle.
Assess and document neurovascular status. Patients with a Lisfranc injury may have a dorsalis pedis artery injury, as it is susceptible to disruption in severe dislocations and should be evaluated in the initial assessment.8 With a crush injury, there may be evidence of swelling, ecchymosis and bruising. If the patient is able to tolerate it, the clinician can examine for pain on forced pronation and abduction; this is specific for TMT injury.10
Examine the patient’s tolerance to bear weight. If the patient is weight-bearing, they may have significant pain in the “push-off” phase of the gait cycle as well as a limping gait and reduced walking speed. The patient will struggle to stand on their toes on the injured foot.[11]
Diagnostic Testing
Plain radiography is the initial imaging study of choice for midfoot injuries where Lisfranc injury is suspected (Images 2-4). Views obtained should include anterior posterior (AP), lateral, and 45-degree internal oblique views.[12] Note that the XR appearance in patients with Lisfranc injuries may demonstrate findings ranging from fracture, dislocation, both, or may even appear normal.

Typical findings on XR when a TMT dislocation/fracture is present include:
- Loss of the normal anatomy with displacement of the proximal metatarsal bones relative to the distal aspect of the 3 cuneiform bones and the cuboid[13]
- Widening at the base of the 1st and 2nd metatarsals > 2.5mm13
- Widening between the cuneiform bones
- Presence of a “flake” fracture (previous called a “fleck sign”), which is a fracture at the base of the 2nd metatarsal or cuneiform10,[14]
- Impaction fractures of the cuboid, medial cuneiform, or navicular bone[15]
In cases of reasonable clinical suspicion, clinicians should have a low threshold to obtain a computed tomography (CT) scan of the foot. If this cannot be achieved expediently from UC, immediate ED referral is recommended.
A CT of the foot without contrast is used not only to assess the extent of the injury but is also useful for preoperative planning.14 Advanced imaging should be guided in conjunction with specialist consultation.
Indications for Referral to the ED
Patients with confirmed or suspected Lisfranc injury on foot XR will be sent to the ED for cross-sectional imaging and orthopedic or podiatry consultation.
Other indications for ED referral include:
- Evidence of neurovascular compromise
- Clinical suspicion for compartment syndrome as evidenced by the “5 Ps”:[16]
- Pain out of proportion to exam findingsParesthesiaPallorPulselessness
- Paralysis
Management of Suspected Lisfranc Injury in Urgent Care

In patients where XR confirms a Lisfranc injury, the patient should be made strictly non-weight-bearing and splinted in a short leg splint. If immediate consultation from UC with podiatry or orthopedic clinicians is possible, they can guide appropriate follow-up and need for additional imaging. In cases where immediate consultation is not possible, then immediate ED referral where appropriate specialist coverage is available is recommended.
In cases with severe midfoot pain and/or swelling with a suggestive mechanism, but negative XR imaging, it is most prudent to splint the foot as if there were a Lisfranc injury. Ensure the patient is non-weight-bearing and referred immediately to an ED where CT imaging is available.
Surgery is occasionally performed emergently based on specialist level decision making. However, in cases of vascular compromise or compartment syndrome, emergent operative repair is generally required. In the absence of these emergent complications, most cases are operatively repaired within several weeks and may require up to 4 months of immobilization.10
Operative techniques are injury dependent and include closed reduction and internal fixation, open reduction and internal fixation, or arthrodesis (reserved for severely comminuted fractures).15

Red Flags and Legal Pitfalls
- Without a high index of suspicion, it is easy to miss a Lisfranc injury. Missed Lisfranc injury can result in significant medicolegal risk for clinicians.[17]
- Many Lisfranc injuries have initially normal XR.[18]
- Compartment syndrome of the foot is a known complication of Lisfranc injuries and should be suspected with severe pain at rest/without weight-bearing16
- Recommendations to avoid missing Lisfranc injuries include:7
- Have a low threshold to obtain XRs in patients with midfoot pain and swelling after trauma
- If a fracture is seen at the proximal metatarsal, suspect Lisfranc injury
- If edema persists for 10 days after the injury, suspect Lisfranc injury
Clinical Scenario Conclusion
The patient’s XR initially appeared non-diagnostic. A foot sprain/contusion was diagnosed and treated. The patient was sent home with a hard-soled shoe but continued to have significant pain. He made an appointment to follow up with an orthopedist the next day. The orthopedist interpreted the XR as diagnostic for Lisfranc fracture/dislocation and subsequently obtained CT imaging of the foot, which confirmed the diagnosis. The patient ultimately underwent operative repair and had a relatively good functional outcome with minimal chronic foot pain.
Takeaway Points
- Lisfranc injury is a high-risk injury and should be suspected in any patient with significant pain and/or swelling of the midfoot, especially after a crushing or twisting mechanism of injury.
- Lisfranc injuries may be bony (ie, fracture), ligamentous, or both.
- A normal XR does not exclude possible Lisfranc injury. CT imaging is considered the definitive imaging modality in cases with negative XRs and ongoing clinical suspicion.
- Delays in diagnosis can result in chronic pain. In cases of reasonable suspicion, immediate podiatry or orthopedic specialist consultation or ED referral is recommended.
- Compartment syndrome of the foot can occur secondary to Lisfranc injuries and should be suspected in patients with increasing foot pain at rest.
Manuscript submitted March 19, 2025; accepted March 29, 2025.
References
- [1]. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691-697.
- [2]. Davis ET. Lisfranc joint injuries. Trauma. 2006;8:225-231.
- [3]. Martin MP 3rd, Patel AH, Cole MW, Gadinsky NE, Collins L, Sherman WF. A rare case of a Lisfranc ligament transection. Orthop Rev (Pavia). 2023;15:56664.
- [4]. Wynter S, Grigg C. Lisfranc injuries. Aust Fam Physician. 2017;46(3):116-119.
- [5]. Stødle A. Lisfranc injuries: Incidence, mechanisms of injuries and predictors of instability. Foot Ankle Surg. 2019. doi:10.1016/j.fas.2019.06.002.
- [6]. Yu X, Pang QJ, Yang CC. Functional outcome of tarsometatarsal joint fracture dislocation managed according to Myerson classification. Pak J Med Sci. 2014;30(4):773-777.
- [7]. Englanoff G, Anglin D, Hutson HR. Lisfranc fracture-dislocation: A frequently missed diagnosis in the emergency department. Ann Emerg Med. 1995;26:229-233.
- [8]. Davis ET. Lisfranc joint injuries. Trauma. 2006;8:225-231.
- [9]. Saab M. Lisfranc fracture-dislocation: an easily overlooked injury in the emergency department. Eur J Emerg Med. 2005;12:143-146.
- [10]. Myerson MS. The diagnosis and treatment of injury to the tarsometatarsal joint complex. J Bone Joint Surg Br. 1999;81-B:756-763.
- [11]. van Hoeve S, Stollenwerck G, Willems P, Witlox MA, Meijer K, Poeze M. Gait analysis and functional outcome in patients after Lisfranc injury treatment. Foot Ankle Surg. 2018;24(6):535-541. doi:10.1016/j.fas.2017.07.003.
- [12]. Grewel U, et al. Lisfranc injury: A review and simplified treatment algorithm. The Foot. 2020. doi:10.1016/j.foot.2020.101719.
- [13]. Wright M. Lisfranc injuries. BMJ. 2013;347:f4561.
- [14]. Boutefnouchet T, et al. Metatarsal fractures: A review and current concepts. Trauma. 2014;16:147-163.
- [15]. Mulier T, et al. The treatment of Lisfranc injuries: Review of the current literature. Eur J Trauma Emerg Surg. 2010;36:206–216.
- [16]. Marchesi M, Marchesi A, Calori GM, et al. A sneaky surgical emergency: Acute compartment syndrome. Retrospective analysis of 66 closed claims, medico-legal pitfalls and damages evaluation. Injury. 2014;45 Suppl 6:S16-S20. doi:10.1016/j.injury.2014.10.017.
- [17]. Ring J, et al. Clinical negligence in foot and ankle surgery. Bone Joint J. 2014;96-B:1510–1514.
- [18]. Sherief TI, Mucci B, Greiss M. Lisfranc injury: how frequently does it get missed? And how can we improve? Injury. 2007;38:856–860.
Author Affiliations: Alexandra Eby, BS, Lincoln Memorial University Debusk College of Osteopathic Medicine. Nicole Meschbach, MD, Adena Regional Medical Center. Authors have no relevant financial relationships with any ineligible companies.
