Published on
Download the article PDF: Clinical Challenges June 2025
Differential Diagnosis
- Posterior vitreous detachment (PVD)
- Retinal detachment
- Vitreous hemorrhage
- Retinal tear
- Retinal hemorrhage
- Ocular migraine
- Optic neuritis
- Retinal arterial or venous occlusion
- Diabetic retinopathy
Diagnosis
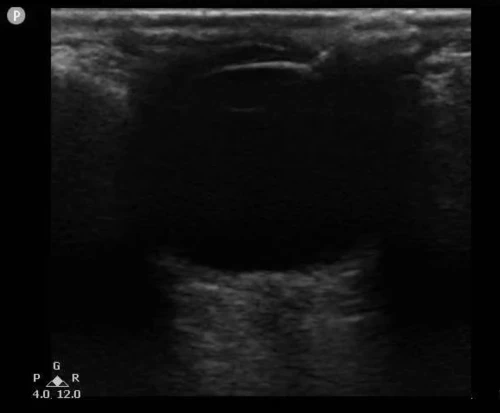
POCUS of the right eye revealed a thin, mobile, echogenic (white) membrane in the vitreous chamber, not tethered to the optic nerve, consistent with PVD. Scattered mobile hyperechoic opacities were also noted—suggestive of vitreous hemorrhage. The unaffected eye showed no such findings.

Based on the POCUS findings—showing no signs of retinal detachment—and the patient’s relatively preserved visual acuity, the provider arranged next-day follow-up with ophthalmology rather than immediate emergency department referral. The ophthalmologist confirmed the diagnosis of PVD with associated vitreous hemorrhage and initiated expectant management with close outpatient monitoring.
Discussion
PVD must be suspected when a patient presents with sudden floaters. The incidence of PVD rises with age, affecting 11–46% of those aged 65–90 years.1 PVD results from the separation of the posterior vitreous cortex from the retina, often due to age-related vitreous degeneration or trauma.2 Although PVD is usually benign, patients are at increased risk for retinal tears or detachment, particularly in the first 6 weeks following symptom onset.3,4 The presence of vitreous hemorrhage or reduced visual acuity (worse than 20/40) elevates this risk.4
POCUS has emerged as a valuable tool for evaluating acute vision changes when direct fundoscopy is inconclusive or technically challenging.5,6 Sonographic findings of PVD include a thin, mobile, hyperechoic membrane seen floating in the vitreous chamber. Unlike retinal detachment, this membrane is not tethered to the optic disc.7 Vitreous hemorrhage appears as swirling, mobile echogenic debris within the vitreous chamber.7,8 A recent meta-analysis found that ocular POCUS performed by emergency physicians had sensitivities of 94% for retinal detachment, 90% for vitreous hemorrhage, and 67% for PVD.9
Rapid POCUS evaluation can help differentiate urgent vision-threatening pathology (eg, retinal detachment) from benign conditions (eg, isolated PVD) that can be managed with outpatient follow-up. For urgent care providers, this distinction is critical in optimizing resource utilization and patient outcomes.
What To Look For
- A mobile, hyperechoic membrane in the posterior chamber not tethered to the optic nerve indicates posterior vitreous detachment
- Hyperechoic particles in the vitreous suggest vitreous hemorrhage
- A ribbon-like flap tethered at the optic disc is consistent with retinal detachment
Pearls for Urgent Care Management
- Ocular POCUS is a simple, accurate tool for evaluating acute visual complaints when ophthalmoscopy is inconclusive
- If retinal detachment is suspected—even with preserved vision—immediate ophthalmology referral is critical10
- Patients diagnosed with posterior vitreous detachment should be educated about the risk of retinal tear/detachment. Advise them to seek prompt care if symptoms worsen or vision deteriorates
References
- Weber-Krause B, Eckardt C. Incidence of posterior vitreous detachment in the elderly. Ophthalmologe. 1997;94(9):619–623.
- Flaxel CJ, Adelman RA, Bailey ST, et al. Posterior Vitreous Detachment, Retinal Breaks, and Lattice Degeneration Preferred Practice Pattern. Ophthalmology. 2020;127(1):P146–P181.
- Hollands H, Johnson D, Brox AC, et al. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302(20):2243–2249.
- Bond-Taylor M, Jakobsson G, Zetterberg M. Posterior vitreous detachment—prevalence and risk factors for retinal tears. Clin Ophthalmol. 2017;11:1689–1695.
- Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002;9(8):791–799.
- Mackay DD, Garza PS, Bruce BB, et al. The demise of direct ophthalmoscopy: a modern clinical challenge. Neurol Clin Pract. 2015;5(2):150–157.
- Baker N, Amini R, Situ-LaCasse EH, et al. Can emergency physicians distinguish retinal detachment from posterior vitreous detachment with POCUS? Am J Emerg Med. 2018;36(5):774–776.
- Lahham S, Shniter I, Thompson M, et al. POCUS in diagnosing retinal detachment, vitreous hemorrhage, and vitreous detachment. JAMA Netw Open. 2019;2(4):e192162.
- Lahham S, Shniter I, Thompson M, et al. JAMA Netw Open. 2019;2(4):e192162.
- Feltgen N, Walter P. Rhegmatogenous retinal detachment—an ophthalmologic emergency. Dtsch Arztebl Int. 2014;111(1–2):12–22.
