Published on
Cathleen DeLaney DNP, MSN-FNP, APRN and Kris Skalsky MSNEd, EdD, RN
Abstract
Background and Purpose: The focus of this project was to determine if an evidence-based educational intervention had an impact on reducing the number of pediatric head injury referrals from the urgent care center to the emergency room. The urgent care center often makes referrals of pediatric head injury patients to the ED, contributing to the overutilization and overcrowding of an already taxed system.
Methods: This was a comparative retrospective pre- and postintervention study, utilizing historical data via retrospective chart review, from the urgent care center regarding pediatric patients with minor head injuries who were sent to the ED. An educational intervention utilizing the Pediatric Emergency Care Applied Research Network (PECARN) guidelines was conducted to improve the knowledge base of the providers within the urgent care center. Data collection during the 4 months prior-to and after the intervention determined if the intervention had an impact.
Findings: A chi-square test for independence (with Yates’ Continuity Correction) indicated that an educational intervention on the PECARN guidelines given to healthcare providers in an urgent care center had no significant association with the number of referrals of pediatric minor head injury patients from the urgent care center to the ED, χ2 (1, 464) = 2.90, p = .09, phi = -.09.
Conclusion: While the results of this study were not statistically significant, there was evidence of improved clinical judgment in referring patients to the ED. Further studies should examine the appropriateness of the referral, thereby demonstrating the effectiveness of an educational intervention utilizing the PECARN head injury guidelines
Introduction
A common scenario that exists in both the primary and urgent care setting is sending minor head injuries to the ED to be evaluated. Many of these patients may leave the ED with nothing more than written and verbal precautions. These nonurgent visits might be avoided if the providers rely on evidence-based practices to make their clinical decisions.
Oman, et al noted that head injuries account for 1 million visits annually to the ED, generating charges from use of computed tomography (CT) of nearly $750 million dollars.1 In the pediatric population, the overuse of CT is more pronounced relative to the difficulty in assessing the neurological status in some age groups.
A 5-year retrospective study of 41 pediatric hospitals by Robertson, McConnel and Green2 examined charges associated with pediatric head injuries. The study acknowledged that head and brain injuries account for one-third of all injury deaths and are the most common cause of pediatric morbidity and mortality (nearly 90% of pediatric injury deaths). An examination of the records from 41 pediatric hospitals over a 5-year period indicated that these injuries accounted almost $1 billion in total charges.2
The Centers for Disease Control and Prevention determined that the rates of traumatic brain injuries in the pediatric population increased for all age groups from 2001 to 2010. However, the largest increase was among children 4 years old and younger; the rate increased >50% from years 2007-2008 to 2009-2010 in those children—nearly twice that of the next largest group (15–24 years of age). This correlates to an increase from 1374.0 to 2193.8 per 100,000 visits to the ED for traumatic brain injury-related related injuries.3
Our study was prompted by the overutilization of the ED for nonurgent medical problems. In particular, the practice of sending minor head injury patients from the urgent care c to the ED for treatment, only to have these patients sent home without any interventions. The practice of sending them to the ED has resulted in increased “left without being seen” numbers, higher dissatisfaction with the hospital system and urgent care center, and increased patient complaints.
An estimated 20 million children seek medical care in pediatric EDs in the United States every year. Consequently, the pediatric ED has become a source of primary care for nonurgent visits.4 Sending these nonurgent patients from the urgent care center to the ED has only increased this problem.
There is little published literature on the number of referrals sent from urgent care centers to the ED in general, even less so when isolated to pediatric minor head injuries. One study by Canares, et al examined perceptions of urgent care providers and concerns when faced with common pediatric conditions. The three scenarios or concerns that challenged providers were: acutely ill infants, minor traumatic brain injury (mTBI), and uncooperative children needing minor procedures. Patients with these concerns were often transferred to the ED for care. The younger the child, the more likely a transfer or referral occurred. mTBI was particularly troublesome for providers due to the concern of missing an intracranial hemorrhage (ICH).5 The study did not mention well-known published mTBI decision-making tools such as the Pediatric Emergency Care Applied Research Network (PECARN) algorithm for low-risk mTBI. Observing the child after injury for a prolonged period of time does not conform to the urgent care center model of “patients in and out quickly,” so, the thinking goes, this is not a feasible option.5
Evidence-based practice guidelines or tools can be crucial in decision-making regarding the level of care that is necessary for patients. Utilizing evidence-based practice guidelines has the potential to improve patient outcomes.6 Utilizing educational interventions to disseminate evidence-based practice guidelines may solve problems or concerns within a healthcare organization. By examining the rationale for the educational intervention and gaps in clinical practice, patient outcomes may be improved.7
The Pediatric Emergency Care Applied Research Network (PECARN) has guidelines for minor head injuries in pediatric patients. These consist of two age-based algorithms to identify children at very low risk for ICH when presenting with mTBI.8 Schonfeld, et al evaluated the performance of the PECARN guidelines in a two-center cross-sectional study with pediatric patients presenting to the ED with mTBI.9 This study accurately identified those at clinically low risk who could safely avoid computerized tomography. Consistent application of the PECARN guidelines in children presenting to an urgent care center with mTBI may change the number of referrals sent to the ED from an urgent care center. Utilizing these guidelines may potentially decrease patient and parent dissatisfaction, overcrowding in the ED, and the number of patients who leave the urgent care center without being seen.
The purpose of this quantitative comparative before and after study using retrospective data was to determine the impact an educational intervention of the PECARN guidelines had on the number of referrals of pediatric minor head injury patients from the urgent care center to the ED.
Summary of Methods and Procedures
Permission to conduct the study at the urgent care center in Texas was received from the American Sentinel University (ASU) Institutional Review Board (IRB). The study utilized a purposive sampling of records of the patients from birth to 18 years presenting with minor head injuries to the urgent care center over a 4-month period prior to an educational intervention (January, February, March, and April 2016) and a 4-month period after the educational intervention (June, July, August, and September 2016).
Evaluation of the ED records guided the necessary evidence-based practice intervention. Patient outcomes in the ED records included one of the two following scenarios:
- The patient was sent home with no interventions
- There were interventions needed, such as CT scans, intravenous fluids, and medications or admission to the hospital.
After the authors reviewed the de-identified data for the months of January, February, March, and April 2016, an educational intervention utilizing evidence-based practice was provided to all providers, registered nurses, paramedics, and medical assistants at the urgent care center. The intervention was designed to effect a practice change regarding which head injury patients need to be sent to the ED.
Summary of Sample and Setting Characteristics
The setting for this study was a pediatric urgent care center associated with a pediatric hospital in a large urban center in Texas. This was a freestanding facility two blocks away from Children’s Hospital in Texas, and the main pediatric ED. The facility operated between the hours of 7 am until midnight, 7 days a week, with physician and advanced practice provider coverage. The facility has 19 patient rooms and averages 180 to 220 patients a day during the busy winter season and 130 to 150 patients in the off season/summer.
The total number of patients presenting to the urgent care center with head injuries in the 4-month period (January, February, March, April 2016) prior to the educational intervention was 223, with 51 patients (22%) sent to the ED for evaluation.
In the 4-month period (June, July, August, September 2016) after the educational intervention, a total of 241 patients with head injuries presented to the urgent care center; of those, 39 patients (16%) were sent to the ED for evaluation (Figure 1).
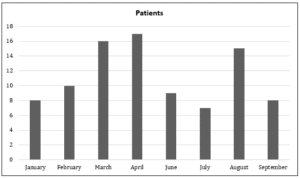
Figure 1. Patients with diagnosis of head injury
Major Findings
A chi-square test for independence (with Yates’ Continuity Correction) was used to analyze the data in this study. Results showed no statistically significant change (p >.05) in the total number of ED referrals of pediatric minor head injury patients, the total number of ED referrals of pediatric minor head injury patients who did and did not require any interventions, or the total number of ED referrals of pediatric minor head injury patients aged <23 months and >24 who did and did not require any interventions after the educational intervention on the PECARN guidelines.
Implications
This study utilized evidence-based practice guidelines on pediatric head injuries in an educational intervention with providers; there was not a resultant statistical decrease in the number of patients sent to the ED for head injuries. This raises the question of evidence-based practice as the standard of care when there is no significant statistical improvement.
Chang and Crowe noted that evidence-based practice (EBP) has been utilized as an ideal method in providing cost-effective care and improving patient outcomes.10 Kin, et al, in a descriptive study acknowledged the role of EBP in healthcare and the influence on the decision-making process and the achievement in quality patient outcomes.11 While there was no significant statistical change in the number of patients referred to the ED in our study, there was a clinical change. Specifically, there was a decrease in the number of patients that had been referred to the ED and sent home without any further interventions or treatments. Thus, the use of EBP guidelines in these studies demonstrates that there can be changes in providers’ behavior and practice norms, thereby improving the patient care experience.
Recommendations
With the rising number of urgent care centers across the United States (in particular, those involving the pediatric population), more studies are needed to investigate the rate of referrals from these organizations to EDs. There is little published literature on the number of referrals sent from urgent care centers to the ED, even less when isolated to pediatric minor head injuries. One study by Canares, et al examined perceptions of urgent care center providers and concerns when faced with common pediatric conditions.5 The most common referrals were head injury, acutely ill infants, and children requiring procedures—interestingly, the younger the child the more likely a referral was made. The paucity of studies regarding pediatric patients in urgent care centers is an area ripe for research and quality improvement.
Limitations
This project was limited by the access to data, inability of the researcher to obtain more specific data, and how the data were obtained. Data collection from the urgent care center relied on paper recording and evaluation by several advanced practice providers, all at different levels of comfort in evaluating data. The advanced practice providers examined the referrals and determined what was considered an ED intervention. An improvement in data collection and retrieval that relied on specific characteristics, rather than subjective criteria, would increase result credibility. The aggregate de-identified data received from the hospital had several errors noting other injuries as possible head injuries. Another area problematic for this study is that scalp lacerations or facial lacerations were not included as head injuries, thereby affecting the data totals.
Discussion
While the results of this study were not statistically significant, there was evidence of improved clinical judgment in referring patients to the ED. When examining the number of patients recorded as referrals from the urgent care center to the ED, there appears to be a change in the number of patients sent that did not require ED interventions. In the 4-month period prior to educational intervention, 51 pateints were sent; in the 4-months posteducation intervention, a total of 39 patients were referred. Review of the data from the urgent care center referral log revealed that the number of patients in the age group of ≥24 months decreased, while there was an increase in the <23-months age group.
In this particular study, the use of aggregate data may have not allowed for a full picture in terms of the number of patients seen in the urgent care center for head injuries. There is the possibility the urgent care center kept a greater number of under the age of 23 months for evaluation, rather than sending to the ED. Another scenario may be that the head injuries that were sent to the ED needed to be sent in greater numbers, with influence from the PECARN guidelines in the manner based on the algorithm. This scenario would indicate that the PECARN guidelines were successful in that the head injuries that needed to go to the ED were referred and ones that did not need referral stayed in the urgent care center. Future studies in this area would also need to evaluate the seasonal aspect of head injuries, as more pediatric head injuries may occur over the summer months due to different activities, thereby showing an increase in the proportion sent to the ED.
Conclusion
While this study did not show a statistically significant change in the number of head injury patients sent to the emergency department after the evidence-based intervention, it is unclear whether the findings are able to be generalized to all urgent cares. Since this study did not specifically evaluate “appropriateness” of referrals, we recommend further study.
Citation: Delaney C, Skalsky K. The effect of PECARN guidelines on minor head injury referrals from the urgent care center to the emergency room. J Urgent Care Med. June 2018. Available at: https://www.jucm.com/the-effect-of-pecarn-guidelines-on-minor-head-injury-referrals-from-the-urgent-care-center-to-the-emergency-room/.
References
- Oman J, Cooper R, Holmes J, et al. Performance of a decision rule to predict need for computed tomography among children with blunt head trauma. 2015;117(2):238-246.
- Robertson BD, McConnel CE, Green S. Charges associated with pediatric head injuries: a five year retrospective review of 41 pediatric hospitals in the US. J Inj Violence Res. 2013;5(1):51-60.
- Centers for Disease Control and Prevention. Rates of TBI-related Emergency department visits by age group—United Sates, 2001-2010. 2014. Available at: http://www.cdc.gov/traumaticbraininjury/data/rates_ed_byage.html. Accessed May 11, 2018.
- Strum J, Hirsh D, Wesselman B, Simon H. Reconnecting patients with their primary care provider: an intervention for reducing nonurgent pediatric emergency department visits, Clin Pediatr. 2014;53(10):988-994.
- Canares T, Brown L, Slotkin R, Garro A. Treating children at urgent care centers: a qualitative study to determine how providers perceive managing pediatric patients. R I Med J. 2015;98(1)48-53.
- Varnell G, Haas B, Duke G, Hudson K. Effect of an educational intervention on attitudes toward and implementation of evidence-based practice. Worldviews Evid Based Nurs. 2008;5(4):172-181.
- Olson SA, Bakken LL. Evaluations of education interventions: getting them published and increasing their impact. J Contin Educ Health Prof. 2013;33(2):77-80.
- Kuppermann N, Holmes J, Dayan P, et al. for the Pediatric Emergency Care Applied Research Network. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170.
- Schonfeld D, Bressan S , Da Dalt L, et al. Pediatric Emergency Care Applied Research Network head injury clinical prediction rules are reliable in practice. Arch Dis Child. 2014;99(5):427-431.
- Chang A, Crowe L. Validation of scales measuring self-efficacy and outcome expectancy in evidence-based practice. Worldviews Evid-Based Nurs. 2011;8(2):106-115.
- Kin Y, Mordiffi S, Liang S, et al. Nurses’ perception towards evidence-based practice: a descriptive study. Singapore Nurs J. 2013;40(1):34-41.
Cathleen DeLaney DNP, MSN-FNP, APRN practices at Cook Children’s Urgent Care Clinic in Hurst, TX. Kris Skalsky MSNEd, EdD, RN is a professor at American Sentinel University. The authors have no relevant financial relationships with any commercial interests.


