In primary care medicine, patients’ symptoms are approached from the “front door;” what are the most likely causes?
Urgent care medicine often starts with a “back door” approach; think “worst first,” then proceed backward through the differential after excluding life threatening causes. Urgent care does not have the luxury of an established patient relationship or defined return visit we often have only one chance to get it right!
The differential for an urgent care patient with headache starts with evaluation for meningitis, subarachnoid hemorrhage, tumor, and carbon monoxide poisoning. This is usually possible through history and physical alone. Conversely, the primary care physician may start with a differential including migraine, tension, or cluster headaches.
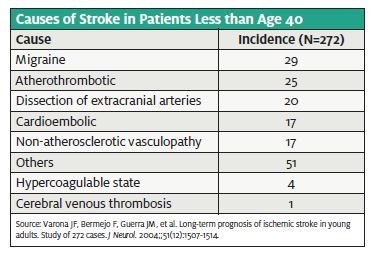
The practice of empiric medicine allows for an accurate diagnosis after cursory evaluation most of the time; unfortunately, however “most” is not often enough. For example, empiric medicine will be wildly inaccurate without factoring in the age of the patient; while uni- lateral weakness and numbness in a 76-year- old is often from a stroke, what are the most likely reasons in a 37-year-old woman?
If the differential does not include the diagnosis, then appropriate and timely therapy will not occur. This case will add one more item to the differential diagnosis of headaches.
Initial Visit
(Note: The following, as well as subsequent visit summaries, is the actual documentation of the providers, including punctua- tion and spelling errors.)
CHIEF COMPLAINT (at 08:54):
Flu-like symptoms
VITAL SIGNS
Time Temp (F) Rt. Pulse Resp Syst
08:57 97.8 T 76 18 141
11:19 97.3 O 88 16 120
Diast Pos O2 sat O2% Pain scale
94 S
70 S 4
HISTORY OF PRESENT ILLNESS (at 09:12):
The patient presents with a spontaneous onset of a se- vere, sharp frontal headache that began gradually today at 6AM. The symptoms are constant and 8/10 in sever- ity. She did have vomiting which beg. 3 hours ago. She did use Tylenol which was minimally effective. She does not have a history of headaches. Patient com- plains of photophobia. She denies, fever, rash, confu- sion, loss of consciousness, weakness of the extremities, slurred speech, vertigo, myalgias, diplopia or blurred vi- sion, cough, rhinorrhea, facial pain, neck stiffness, light- headedness, nausea/vomiting, or abdominal pain.
PAST MEDICAL HISTORY/TRIAGE:
Allergies: NKDA Medications: Tylenol PMH: None
PSH: None
Social history: No smoking, alcohol or drugs
Family history: Heart disease, HTN. No CA, DM, CVA.
PHYSICAL EXAM (at 09:17):
General: Well-developed, well-nourished, poorly- hydrated
Eyes: Pupils are equal, round and reactive to light. The extraocular muscles are intact. Fundoscopic exam is normal.
Neck: There is no cervical lymphadenopathy. No masses or thyromegaly, no JVD.
Cardiovascular: The heart has a regular rate and rhythm without m/r/g.
Respiratory: The lungs are clear to auscultation and per- cussion bilaterally.
GI: There is no pain with palpation.
Musculoskeletal: There is full ROM with movement. Integumentary: The skin appears normal for age and race. It is warm and dry.
Neuro: Patient is alert and oriented to person, place, and time. Cranial nerves II-XII are intact. Sensory and mo- tor functions are intact. Finger to nose is WNL. Grasp is equal bilaterally. The gait is normal.
ORDERS (at 09:17): Demerol 50mg IVP, Phenergan 12.5mg IVP. IV fluids NS 2 L bolus
RESULTS (results at 10:53):
Test Flag Value Units Ref. Range
WBC 13.1 K/uL 4.6-10.2
HGB 13.4 G/DL 13.5-17.5
PLT 254 K/uL 142-424
Test Flag Value Units Ref. Range
NA 136 MMOL/L 135-144
K 3.9 MMOL/L 3.5-5.1
CL 102 MMOL/L 98-107
CO2 28 MMOL/L 22-29
BUN 12 MG/DL 7-18
CREAT 0.8 MG/DL 0.6-1.3
Test Flag Value Units Ref. Range
CK H 233 U/L 21-232
CKMB H 5.9 NG/ML 0.0-5.0
RELIND 2.5 0.0-4.0
TROPI .06 NG/ML .00-.27
Urine: Urine pregnancy results are negative. Urine dip
– WNL.
PROGRESS NOTES (at 11:57):
Patient is feeling much better. Patient is ready to go home. Spinal tap was discussed with the patient and her husband, but they refused, promising to return if fever, stiff neck, weakness, paralysis, or sensory loss.
RADIOLOGY:
UNENHANCED BRAIN CT: Negative
DIAGNOSIS (at 11:58):
Gastroenteritis, Cephalgia
DISPOSITION (12:26): The patient was discharged to Home ambulatory with spouse. Follow with the PCP on call (she is given name and number) if not improved in 3-4 days. Aftercare instructions for gastroenteritis and headache. Prescriptions for Phenergan and darvocet.
Discussion of Documentation and Risk Management
Issues at Initial Visit
Error #1: Incompletely documented progress note.
Discussion: The patient presented with a severe new- onset headache, which should be concerning for subarachnoid hemorrhage. Brain CT has a sensitivity of 91% in patients without focal neurologic symptoms; lumbar puncture is mandatory if the CT is negative.
The progress note documents discussion and refusal of LP, but not that the patient was apprised of the risks of missed subarachnoid hemorrhage and a rebleed rate of about 30%, with likely permanent neurologic impairment. No one wants to have a needle inserted into their back, but when faced with a poor outcome and possible admission to an extended-care facility and loss of independence, most will choose short-term discomfort to avoid serious long-term consequences.
Patients have every right to refuse the LP, but when the implications of missed diagnosis are so extreme, risks need to be documented and patients should be asked to repeat back those risks to ensure understanding.
Teaching point: The patient can only give informed refusal of a given procedure when the risks and benefits are discussed and understood completely. When patients do not accept your advice, document specifics of the discussion, including risks of missed diagnosis
Error #2: One set of cardiac markers without an EKG. Discussion: One would assume acute coronary syndrome (ACS) was considered, as a troponin was ordered. This does seem a bizarre evaluation with this presentation. If this diagnosis were being considered, an EKG and (at the least) a review of symptoms (ROS) including chest pain would be needed. The troponin excludes acute myocardial infarction (AMI) ranging from six hours previous to one week previous, but does not exclude a more recent AMI or angina (which would not cause a change in troponin). Her symptoms started three hours prior to presentation, so we would not expect the first troponin to be elevated even with AMI.
Teaching point: One set of cardiac enzymes drawn three hours after onset of symptoms without an EKG does not rule out ACS or AMI.
Error #3: Conflicting documentation and inappropriate discharge diagnosis.
Discussion: One of the patient’s discharge diagnoses was gastroenteritis. There was mention of vomiting in the HPI, but no diarrhea; ROS says no vomiting and also has no mention of diarrhea.
The documented symptom complex and exam findings should support the diagnosis. Discrepancy between doctor and nurse documentation can be the death knell of a legal defense; discrepancy within a physician’s documentation causes the observer to question the accuracy of the entire chart. If there is diagnostic uncertainty, bet- ter to not guess at a diagnosis.
Additionally, this chart leaves a strange feeling that something is being left out. Why was so much done on a routine headache patient (e.g., blood work with less than three hours of vomiting, cardiac enzymes)? Was there something else about the patient not noted in the record?
Teaching point: Gastroenteritis is a garbage diagnosis probably seen on more malpractice charts than any other. If there is no diarrhea, the patient does not have gastroenteritis. If there is uncertainty, this should be dis- cussed with the patient and reflected in the chart.
Error #4: Ineffective medication prescription.
Discussion: If you want to treat pain use effective pain medications such as hydrocodone (Vicodin) or oxycodone (Percocet). Medications such as propox- yphene (Darvocet) or acetaminophen plus codeine (Tylenol #3) are no more effective against pain than plain acetaminophen, but they are more effective at causing vomiting, sedation, and falls.
Teaching point: If you want to treat pain, then use effective medications.
Error #5: Inadequate follow-up instructions.
Discussion: Aftercare instructions need to be time- and action-specific. The patient presented with an undiffer- entiated and incompletely worked up high-risk complaint. The patient was told to see her primary care physician if not improved in three to four days; the natural histo- ry of a sentinel bleed from subarachnoid hemorrhage is improvement followed by sudden catastrophe with rup- ture of the aneurysm. If this was the physician’s chief con- cern, how would the follow-up ensure the diagnosis was not missed? It is also reasonable to tell the patient to re- turn immediately for any new or worsening symptoms.
Teaching point: Patients need to know exactly when to return and why to return.
SUMMARY OF ED VISIT 2 (THREE DAYS LATER)
- 18:34: ED return (3 days later) with complaint of left arm numbness and weakness
- 21:21: is seen with history confirming intermittent HA and neck pains for 4 days. Initial set of vital signs are normal. Neuro exam documents left upper and lower extremity weakness
- Brain CT repeated at 21:27 is again normal
- 22:40: Progress note documents administration of pain meds for right neck pain radiating to occiput
- 23:08: Lumbar puncture done with WBC = 0 and RBC =1
- 23:23: Nurse notes sudden change of condition; pt. incontinent of urine and right eye is deviated to the right. cannot move body in coordinated fashion.
- Doctor orders neck CT
- 01:35: Only minimal use of left side, mental status gross- ly decreased with ability to follow simple commands only
- 02:02: Radiologist calls with CT results: Right carotid artery dissection
- Admission: Inpatient MRI demonstrates large right middle cerebral artery infarct with edema and subfalcine herniation and brainstem infarct. No flow in the right internal carotid artery
Two days later: is unresponsive with fixed pupils, no purposeful movements. EEG shows brain death. Pt. extubated and expires
Final diagnosis: Carotid artery dissection
Discussion of Carotid Artery Dissection and Documentation Points
Of the 1 million headache visits to ED every year, less than 4% will have a serious cause. Carotid artery dissec- tion is fairly rare, with an incidence of 2.5 to three cases per 100,000. It may be spontaneous in origin or second- ary to trauma, ranging from high-speed multisystem traumas to seemingly benign manipulations in a physi- cian or chiropractor’s office.
This brings us to the most important learning point of this case: stroke symptoms in young patients need an expanded differential compared with older patients. The initial ED evaluation had some bizarre aspects within the documentation and evaluation, but the diagnosis was not able to be made at that time. When the patient returned to the ED she had headache, neck pain, and stroke symptoms. In a 37-year-old woman without cardiac disease, hypertension, or atheroscl rotic disease, an embolic stroke remains in the differential, along with other possibilities. The initial “cook- book” evaluation including head CT and lumbar puncture did not seem to be pursued initially, which delayed diagnosis for about five hours.
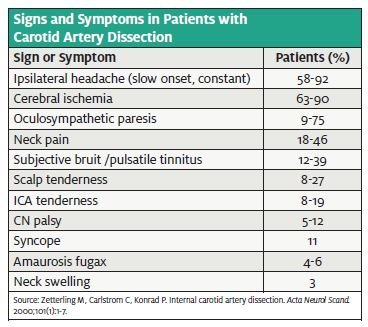
The initial presentation of carotid dissection is often non- specific, as the only initial symptom may be pain—often, a severe headache or pain to the ipsilateral face, orbit, or neck. Physical exam may reveal a carotid bruit on auscultation. Many patients later develop an ischemic cerebral event, usually due to distal embolization from the dissecting vessel. These patients often will present with headache plus a focal neuro deficit such as cranial nerve palsy or Horner’s syndrome.
While this is true in the patient discussed here, an initial consideration of the differential diagnosis appears to be lacking. Head CT scan was ordered almost two hours after presentation, and while it may have been appropriate for initial screening, it fails to target the most likely diagnosis.
The initial diagnostic work-up to evaluate for carotid dissection often starts with a CT scan of the head and neck. Those with a normal CT and high pre-test prob- ability should have MRI/MRA of the head and neck.
The mainstay of therapy is systemic anticoagulation to prevent ischemia due to thromboembolic events, unless contraindications, such as the following, exist:
- large infarct with associated edema and mass effect
- infarction hemorrhagic transformation
- intracranial aneurysm
- intracranial dissection
In these circumstances, the alternative therapy is usually antiplatelet agents. For those who fail medical management, alternative therapies include angioplasty, intraarterial thrombolysis, or stenting.
Summary
Initially, the patient presented with new-onset severe headache and vomiting, a collection of nonspecific and incredibly common symptoms encountered on a daily basis. Unfortunately, she had no other hard findings to point toward carotid artery dissection, and missing the diagnosis on the initial visit may actually be considered the standard of care.
As Greg Henry noted in Bouncebacks!, “There will be, once in your career, a case such as this and there is noth- ing you can do to prevent it. If every patient with a nor- mal exam and a headache were admitted to the hospi- tal…, we would hurt more people than we help.”
The real opportunity to help was when she returned with headache, neck pain, and neurological symptoms. Adding carotid dissection to our differential will help prevent such catastrophic outcomes.
Resources and Suggested Reading
- Edlow JA, Panagos PD, Godwin SA, et Clinical Pol- icy: Critical Issues in the Evaluation and Management of adult Patients Presenting to the Emergency De- partment with Acute Headache. Ann Emerg Med. 2008;52:407-436. Available at: www.acep.org/workarea/- downloadasset.aspx?id=8802.
- Fisher The headache and pain of spontaneous carotid dissection. Headache. 1982;22:60-65.
- Zetterling M, Carlstrom C, Konrad Internal carotid artery dissection. Acta Neurol Scand. 2000;101:1-7.
- Kirsch E, Kaim A, Engelter S, et MR angiography in in- ternal carotid artery dissection: Improvement of diagno- sis by selective demonstration of the intramural haematoma. Neuroradiology. 1998;40:704-709.
- Lyrer P, Engelter Antithrombotic drugs for carotid ar- tery dissection. Stroke. 2004;35:613-614.
- Muller BT, Luther B, Hort W, et Surgical treatment of 50 carotid dissections: Indications and results. J Vasc Surg. 2000;31:980-988.
- Varona JF, Bermejo F, Guerra JM, et Long-term prog- nosis of ischemic stroke in young adults. Study of 272 cases. J Neurol. 2004;51(12):1507-1514. Ramirez-Lassepas M, Espinosa CE, Cicero JJ, et al. Pre- dictors of intracranial pathologic findings in patients who seek emergency care because of headache. Arch Neurol. 1997;54(12):1506-1509.