Resolution
Physical Examination
On examination, the patient had a temperature of 99.7°F (37.6°C), a pulse rate of 138 beats/min, a respiration rate of 40 breaths/min, and a blood pressure of 72/43 mm Hg. He was alert and oriented, sweaty, panicky, and tachypneic. On examination of his lungs, he had decreased lung sounds on the left and clear on the right. He had tachycardia, and his heart had a regular rhythm, without murmur, rub, or gallop. His abdomen was slightly distended, soft, and nontender, without rigidity, rebound, or guarding. He was profusely diaphoretic. He had no swelling or pain in his extremities and no calf muscle pain, and his peripheral pulses were weak and thready.
Differential Diagnoses
- Pneumonia
- Hemothorax
- Lung cancer
- Cardiac tamponade
- Free air under the diaphragm
Tests
Testing for uncomplicated cases involves a chest x-ray performed during inspiration. The conventional wisdom is that an x-ray during forced expiration may show the pneumothorax, but one study found equal rates of visualization for inspiratory films and for expiratory films. Patients with chronic obstructive pulmonary disease (COPD) and bullous changes may mistakenly be diagnosed with pneumothorax. Careful review of the chest x-ray and comparison with previous x-rays is important to prevent unnecessary transfer to an emergency department (ED) or placement of a tube thoracostomy, which might worsen the patient’s condition.
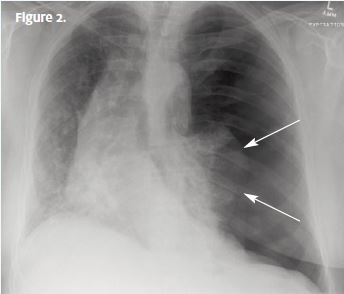
A chest x-ray (Figure 2) was performed, which revealed a tension pneumothorax. Note the compressed left lung, the lack of lung markings on the left, deviation of the trachea to the opposite (right) side, and deep sulcus (costophrenic angle) on the left.
Resolution
Diagnosis
The patient has tension pneumothorax, which is a medical emergency.
Learnings
A pneumothorax can occur from trauma or spontaneously. A primary spontaneous pneumothorax occurs in patients without lung disease, whereas a secondary spontaneous pneumothorax occurs in patients with a history of known lung disease such as COPD or a history of previous pneumothorax.
The visceral pleura (outer lining of the lung) approximates against the parietal pleura (the inner lining of the thoracic cavity). When air enters the space between the visceral and parietal pleura, it will be evident on chest x-ray as a dark, air-filled cavity; that is a pneumothorax. The most common underlying causes of spontaneous pneumothorax are COPD and tuberculosis. A proposed mechanism of spontaneous pneumothorax is rupture of subpleural bullae into the pleural space (the space between the visceral and parietal pleura).
Patients with pneumothorax usually report chest pain, shortness of breath, or both. The acuity of onset in nontraumatic pneumothorax may be rapid, during an episode of negative pressure within the intrathoracic cavity, as can occur with inhalation of a cigarette or when inhaling from other types of smoking devices, or it may be gradual with a smaller pneumothorax. Patients typically localize the site of pain to the affected side.
Treatment
- For patients with spontaneous pneumothorax who are hemodynamically stable, observation with a repeat chest x-ray the next day is an appropriate therapy. This should be coordinated with a thoracic surgeon or pulmonologist.
- For patients with a large pneumothorax or one causing symptoms of shortness of breath or hemodynamic instability, the patient should be transferred to an ED for decompression, either with a valve or chest tube.
- If there is evidence of tension, emergency medical services (EMS) should be promptly activated.
- If the patient is hemodynamically unstable and the wait for EMS will be prolonged, needle decompression should be performed in the second intercostal space, midclavicular line, with an 18-gauge catheter placed over the rib. When a rush of air is obtained, remove the needle and leave the catheter in place.
Indications for Transfer to an Emergency Department
- With a small, nonacute pneumothorax in the presence of hemo dynamic stability, the patient can be transferred by a private vehicle.
- If the patient is hemodynamically unstable, as evidenced by significant tachycardia, tachypnea, and hypotension, then transfer should be done by EMS.
- With signs of tension pneumothorax, the patient should be decompressed before transfer.
Figure 1 from Brims F. Tension pneumothorax—an alternative view [2014 August 22]. Life in the Fast Lane [blog]. Available from: http://lifeinthefastlane.com/tension-pneumothorax-an-alternative-view/. Figure 2 is a modified version of Figure 1. (Used with permission under a Attribution-NonCommercial-ShareAlike 4.0 International license:
http://creativecommons.org/licenses/by-nc-sa/4.0/.)
