Differential Diagnosis
- Atrial fibrillation, third-degree AVB
- Atrial flutter, second-degree AVB, acute anterior MI
- First-degree AVB, sinus bradycardia, acute lateral wall MI
- Second-degree AVB, Wellen’s sign, atrial flutter
- Wenckebach second-degree AV block, acute inferior STEMI, low voltage
Diagnosis
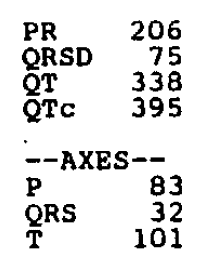
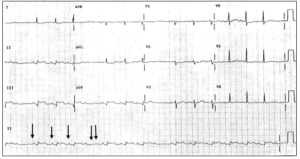
The ECG shows the correct diagnosis to be Wenckebach second-degree AV block, acute inferior MI, and low voltage.
This case illustrates that there are often multiple findings on each ECG. Whereas a quick glance might suggest atrial fibrillation/flutter, a closer inspection would show that there are P waves preceding (almost) every QRS. A look at the “rhythm strip” (which is lead II at the bottom; see arrows) will reveal that there are p waves preceding each QRS, and each of these PR intervals sequentially lengthens then there is a dropped beat (double arrow). This is type 2 AV block (Wenckebach). However, there are other concerning changes on this ECG, including ST elevation in the inferior leads, II, III, and aVF, suggestive of acute inferior STEMI – notice that there are reciprocal changes also, namely ST depression in lead aVL making the ECG even more concerning for ischemia/infarction. Finally, the ECG is suggestive of low voltage, which can simply be from obesity or COPD, but could also be from a pericardial effusion or tamponade.
Learnings/What to Look for
- Having a “cookbook” approach to ECGs, including first assessing rate and rhythm, will avoid confusing an ECGT with a block or multifocal atrial tachycardia (MAT) from atrial fibrillation
- ST changes which are anatomically consistent leads (in this case in the inferior leads II, III, and aVF) should be assessed for elevation or depression
- “Low voltage” is defined as QRS amplitudes of <15 mm in the sum of leads I, II, and III, or 30 mm in the sum of leads V1, V2, and V2
- Low voltage may be from an increased AP diameter, such as in obesity or COPD, but may also be from something more serious such as a pericardial effusion/tamponade or severe hypothyroidism
Pearls for Initial Management and Considerations for Transfer
- Patients with STEMI require emergent care in a facility with the ability to perform procedural catheterization
- Notify the EMS of a STEMI, consider starting an IV, attaching the patient to a monitor, and administering an aspirin
- Though a low-voltage ECG may be from body habitus (obesity) or increased AP diameter (COPD), if due to a pericardial tamponade, this may require emergent drainage; correlate with old ECG and clinical presentation
