Urgent message: Shorter urgent care visits are correlated with higher experience scores. The presence of learners does not negatively impact patient experience scores.
David Skoglund, MD, MS; Brian Lee, PhD, MPH; and Amanda Montalbano, MD, MPH
Citation: Skoglund D, Lee B, Montalbano A. Learner presence does not negatively impact patient experience in pediatric urgent care. J Urgent Care Med. 2021;16(2):30-36.
ABSTRACT
Objective
The number of trainees seeking pediatric educational opportunities in community outpatient settings is increasing. One underutilized and understudied outpatient care location that may help provide these opportunities is urgent care. Urgent care encounters are expected to be convenient and seamless. As learners are incorporated into these sites, their effect on patient experience requires evaluation.
Methods
All patient encounters from a metropolitan Midwestern pediatric tertiary care organization’s three freestanding pediatric urgent care sites in 2018 and 2019 with associated patient experience survey data were included. Encounters were assigned into those with and without learners based on provider shift data. Experience scores were categorized as detractors (scores of 0-6), neutral (7-8), or promoters (9-10). Multivariable regression models examined the relationship between learners and having a promoter experience score, adjusting for imaging performed, medications given, calendar quarter, and standardized length of stay (LOS).
Results
A total of 19,900 encounters were included in the 2-year study period. The prevalence of learners was not significantly different for each experience score category—detractor 4.7%, neutral 5.1%, and promoter 5.3% (p=0.54). A one standard deviation decrease in LOS was associated with greater likelihood of a promoter score (OR 1.35, 95% CI 1.30-1.39; p-value <0.0001). Learner presence did not significantly change this pattern.
Conclusions
Shorter urgent care visits are correlated with higher experience scores. The presence of learners does not negatively impact patient experience scores. Additional work will include stratifying learners by their training level and determining the impact of learners on provider efficiency.
INTRODUCTION
Supervised clinical experience is a critical component of training for all medical professional students. Medical facilities may encounter increasing pressure to provide educational opportunities to host clinical rotations for learners in a variety of fields. Medical school enrollment has increased by 52% since 2002, largely due to the establishment of 29 new accredited medical schools and stimulated by Association of American Medical College (AAMC) encouragement in 2006.1 PA programs more than doubled in number from 57 in 1993 to 120 by 1999, and growth has persisted since then with 210 currently accredited programs.2 Approximately 85% of surveyed medical school deans were concerned about the limited clinical opportunities that were available for their students.1 All medical learners require clinical training, and innovation will be required to increase the number of sites available for clinical training. As medical facilities provide training opportunities, it is necessary to evaluate the impact of those learners on the clinical operations of those facilities.
With nearly half of the projected physician shortage being in primary care, clinical training in this area is especially dire.3 There is a limited number of community sites for pediatric trainees, necessitating innovation in clinical training opportunities. Pediatric urgent care facilities provide care for acute illness and injuries when the medical home is not available or when such care is beyond their scope.4 These facilities are staffed with board-certified pediatricians and advanced-practice providers with pediatric experience.
In a 2016 study of pediatric urgent cares, 94% of facilities reported hosting medical trainees (medical students, residents, and advanced practice provider students).5 While urgent care offers a unique opportunity to provide experience with patient encounters for common complaints, these encounters occur at a fast pace. As patients and families expect to have convenient, quick visits, learner presence at these sites may impact patients’ perceived experience during the encounter.
Few studies have reported how learner presence impacts patient experience scores, and no studies have evaluated the impact of medical trainees in the pediatric urgent care setting. The aim of this study was to determine whether learner presence affected patient experience scores among encounters in three pediatric urgent care sites.
METHODS
Population
This retrospective study included all patient encounters with a completed postencounter patient experience survey in calendar years 2018 and 2019 at a metropolitan Midwestern pediatric tertiary care organization’s three freestanding pediatric urgent care sites.Encounters were excluded if the patient eloped before being seen or refused medical care.
Data
A nationally validated patient experience survey was administered via email, text, or a computerized phone call. Each family received up to three attempts for survey completion. Exclusion rules included patients who received a survey for another encounter from the enterprise within the previous 14 days, patients who had previously requested not to be surveyed, or patients who were not living with a parent or permanent guardian. An overall rating for urgent care was generated from the survey question, “Using a number from 0 to 10, where 0 is the worst visit possible and 10 is the best visit possible, how would you rate this visit?” For this study, experience scores were divided into three groups: 0-6 (detractors), 7-8 (neutral), and 9-10 (promoters).
The provider shift data during our study period includes whether the provider (“preceptor”) was working with a learner during their scheduled shift. Our learner population included residents, medical students, and physician assistant students. Our learners were assigned to a physician preceptor each day. The shift data were then merged with the encounter data, based on the encounter admission date and preceptor as documented in the electronic health record (EHR).
We considered encounters as having learners present if they were seen by a physician on a day when that physician was denoted to be precepting a learner on the shift data.
Lastly, the encounter length of stay (LOS), defined as time between registration and discharge, was calculated and then standardized (mean 0, SD 1). Binary indicators were created to indicate whether imaging (ie, radiographs) was performed, laboratory testing was obtained, or medications were administered.
Analysis
The distribution of experience score groupings (ie, detractors, neutral, promoters) was calculated by learner presence, imaging/lab tests, medications provided, and calendar quarter and compared using Pearson’s chi-square test. The distribution in standardized LOS was compared between experience scores using the Kruskal-Wallis test. A multivariable logistic model was run to calculate the odds of a promoter score (9-10) based the presence or absence of learners after adjusting for imaging, labs, medication, calendar quarter, and standardized LOS. Postestimation marginal effects were used to calculate predicted probabilities of a promoter score and associated confidence intervals. Promoter score was used to best highlight the preferred experience score outcome. All analyses were completed using SAS 9.4 software (Cary, NC).
This study was deemed nonhuman subjects research by the Institutional Review Board at Children’s Mercy Kansas City.
RESULTS
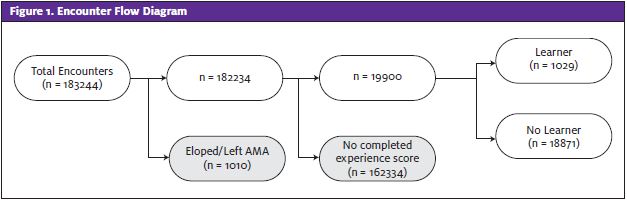
From January 1, 2018 through December 31, 2019 there were 19,900 encounters with associated patient experience scores, representing 10.9% of all encounters (182,234) during this period. Relatively few encounters in the study sample had learners present, (1,029, 5.2%) (Figure 1). There were more encounters with learners in the winter and fewer in the summer (calendar Q1 225, 3.78%; Q2 177, 3.73%; Q3 281, 6.39%; Q4 346, 7.21%; p<0.0001).
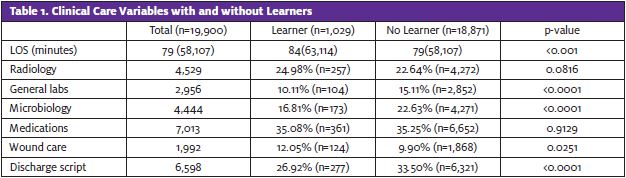
When a learner was present, a significantly lower proportion of encounters had labs, microbiology orders, and written discharge scripts. These encounters had significantly more wound care orders. In-house medication administration and radiology orders did not differ significantly based on whether a learner was present or not (Table 1).
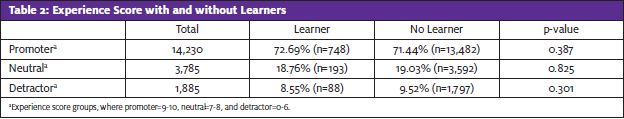
Overall, patient experience scores were mostly promoters (71.5%). The prevalence of learners was not statistically different among the experience score groups—detractor (4.7%), neutral (5.1%), or promoter (5.3%; p=0.54). In general, neutral and promoter scores had higher prevalence of medications given during the encounter (30.0% detractor, 35.8% neutral, 35.8% promoter) and imaging performed (19.2% detractor, 23.5% neutral, 34.2% promoter encounters), respectively.
There was an inverse linear relationship between LOS and probability of a promoter score. Shorter LOS was associated with a greater likelihood of promoter experience score (OR 1.35, 95% CI 1.30-1.39, p-value <0.0001). When LOS and learner presence were modeled as an interaction term, the coefficient was not significant (p=0.465), suggesting that the presence of a learner did not significantly modify the relationship between LOS and promotor scores (Figure 2).
The presence of a learner did not result in significantly different odds of having a promoter score (OR 1.06; 95% CI 0.92, 1.22; p =0.393) when compared with encounters where learners were absent. After adjusting for LOS, calendar quarter, imaging, and medications, the presence of a learner continued to be nonsignificant (adjusted OR 1.09; 95% CI 0.94, 1.26; p=0.235).
DISCUSSION
This study identifies that learners in an urgent care system in a large Midwestern metropolitan area have no significant impact on patient experience scores (see Table 2). For a healthcare system in need of primary care providers and a medical education system in need of training sites, it is important to identify clinical venues within which to expand medical education. Practically, these venues will need to do so without significant changes to their typical operations or impact on patient care. This study suggests that learners can be integrated into urgent care systems without negative impact on patient perception of the care experience.
Previous literature has also documented that the presence of learners does not detract from the rating of patient experience. Medical student involvement in a Labor and Delivery unit was found to have a not-significant impact on patient satisfaction.7 As students in a neurology clerkship saw more patients, they experienced greater educational value and the clinic became more productive.8 Medical student participation in an emergency room setting had no impact on satisfaction scores or patient measures of quality of care.9 Medical student involvement also had no effect on patient satisfaction in a family medicine clinic setting.10 A systematic review of patient attitudes regarding medical student participation found that, while patient satisfaction is not affected by their participation, this does not necessarily mean that these patients prefer medical student involvement in their care.11 While these care sites did not show impact on patient satisfaction, it was not clear if the high-pace environment and expectations of timeliness and convenience may result in different findings in pediatric urgent care.
This study did highlight the association of LOS with overall rating of experience in pediatric urgent care. While it would seem that integrating a learner into the workflow of an urgent care would increase overall length of stay, we did not see an impact on overall rating between learner presence or absence when controlling for LOS. In fact, while not statistically significant, the data suggest that presence of learners may mitigate the negative effects on rating of experience even with increasing lengths of stay.
Similarly, increased use of resources (imaging and labs) would likely extend LOS; however, promoters were more likely in encounters using these resources. Therefore, while LOS has a high correlation with experience scores, this association may be mitigated if the family feels their increased time was well spent (eg, extra set of eyes on the patient by a learner, a more thorough examination or use of studies, etc.). While the expectation of a pediatric urgent care is to be efficient, families clearly also value efficacy, safety, and thoroughness.
LIMITATIONS
This study has limitations that should be stated. Our data were from a single Midwestern academic pediatric urgent care center, which may limit the generalizability of the outcomes to general urgent care centers, nonacademic facilities, or other regions of the country. As our data include <11% of encounters at the studied sites, generalizability may be further limited. While the total number of included encounters was high, the number of those encounters with learners was fairly small. Completion of the experience survey is voluntary, so there may be selection bias in which families opt to submit a completed survey.
To fully categorize the effect of learners on an urgent care system, further study will be needed to determine their impact on LOS, care delivery, and provider efficiency. Additionally, with increased number and diversity of learners, investigating learner presence in urgent care should be stratified by learner type. Not to be overlooked, the value of training in urgent care as determined by the learners themselves should also be investigated.
Acknowledgments: The authors wish to thank the Children’s Mercy Kansas City Division of Urgent Care for their devotion to furthering the education of all of our learners.
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Previous presentations: Poster presentation at the Society for Pediatric Urgent Care conference in Fort Worth, TX in 2019. National webinar on 12-12-19 for the Society for Pediatric Urgent Care. Poster presentation at the Pediatric Urgent Care Conference in Los Angeles, California in 2020. National webinar on 9-3-20 for the Academic Pediatric Association and the Society for Pediatric Urgent Care.
REFERENCES
- AAMC. U.S. Medical School Enrollment Surpasses Expansion Goal | AAMC. Association of American Medical Colleges Press release. July 25, 2019. Available at: https://www.aamc.org/news-insights/press-releases/us-medical-school-enrollment-surpasses-expansion-goal. Accessed August 20, 2020.
- Cawley JF, Jones PE, Miller AA, Orcutt VL. Expansion of physician assistant education. J Physician Assist Educ. 2016;27(4):170-175.
- Association of American Medical Colleges. 2014 Physician Specialty Data Book. Washington DC; 2014. Available at: https://members.aamc.org/eweb/upload/Physician Specialty Databook 2014.pdf. Accessed May 19, 2017.
- Conners GP, Kressly SJ, Perrin JM, et al. Nonemergency acute care: when it’s not the medical home. Pediatrics. 2017;139(5:e20170629
- Montalbano A, Montgomery E, Lee B. Organization for Urgent Care Health 2017 Data. Society of Pediatric Urgent Care Infographic. Available at: https://www2.urgentcarepeds.org/members/OUCH-2017-Infographic.pdf. Published 2018. Accessed August 20, 2020.
- Co JPT, Sternberg SB, Homer CJ. Measuring patient and family experiences of health care for children. Acad Pediatr. 2011;11(3 Suppl):S59-S67.
- Malhotra T, Thomas S, Arora KS. Impact of medical students on patient satisfaction of pregnant women in labor and delivery triage. Matern Child Health J. 2019;23(11):1467-1472.
- Tanner JA, Rao KT, Salas RE, et al. Incorporating students into clinic may be associated with both improved clinical productivity and educational value. Neurol Clin Pract. 2017;7(6):474-482.
- Bernard AW, Martin DR, Moseley MG, et al. The impact of medical student participation in emergency medicine patient care on departmental Press Ganey scores. West J Emerg Med. 2015 Nov;16(6):830-838.
- Speicher MR, Sterrenberg TR. Students do not reduce patient satisfaction in a family medicine clinic as measured by a nationally used patient satisfaction instrument. Fam Med. 2015;47(3):227-230.
- Vaughn JL, Rickborn LR, Davis JA. Patients’ attitudes toward medical student participation across specialties: a systematic review. Teach Learn Med. 2015;27(3):245-253.
Author affiliations: David Skoglund, MD, MS, University of Missouri-Kansas City School of Medicine; University of Kansas School of Medicine; Division of Urgent Care at Children’s Mercy Kansas City. Brian Lee, PhD, MPH, University of Missouri-Kansas City School of Medicine; Division of Health Services and Outcome Research at Children’s Mercy Kansas City. Amanda Montalbano, MD, MPH, University of Missouri-Kansas City School of Medicine; University of Kansas School of Medicine; Division of Urgent Care, Children’s Mercy Kansas City; Patient and Family Engagement, Children’s Mercy Kansas City.
