The American Medical Association has announced it is taking the first steps towards revising the new Evaluation and Management (E/M) guidelines that the Centers for Medicare and Medicaid Services (CMS) introduced last year to reduce the administrative burden on clinicians with the Patients over Paperwork initiative.1 Effective as early as January 1, 2021, office visit Level 1 E/M code 99201 will be deleted. Additionally, while the history and exam will be required to be reviewed by the provider, they will not be scored as key components for selecting an E/M service level. Instead, providers will select E/M codes based on 1) the level of medical decision making (MDM) involved, or 2) the total time spent performing the service on the day of the visit. Regardless of the method chosen, medical necessity must still be documented to support the charge.
Guidelines for E/M services will restructured into three sections:
- Guidelines common to all E/M services
- Guidelines for office or other outpatient E/M services, to distinguish the new reporting guidelines for the office or other outpatient services codes 99202-99215
- Guidelines for hospital observation, hospital inpatient, consultations, emergency department, nursing facility, domiciliary, rest home or custodial care, and home E/M services
The guidelines will be revised to ensure there is no conflicting information between the different sets. The AMA states they will also be adding an MDM table and definition of terms associated with the elements of MDM that will be applicable to codes 99202 through 99215.
You can also expect to see new definitions related to medical decision making such as:
- “Number of Diagnoses or Management Options” is changed to “Number and Complexity of Problems Addressed”
- “Amount and/or Complexity of Data to be Reviewed” is changed to “Amount and/or Complexity of Data to be Reviewed and Analyzed”
- “Risk of Complications and/or Morbidity or Mortality” is changed to “Risk of Complications and/or Morbidity or Mortality of Patient Management”
Also approved was a revised definition of time associated with E/M codes 99202 through 99215, from “typical face-to-face time” to “total time spent on the day of the encounter,” eliminating the need to calculate how much of the time spent with the patient was directed towards counseling and coordination of care. The total time values associated with each office/outpatient E/M code will be redefined, as well. The AMA has also proposed to add guidelines for reporting time when more than one individual performs distinct parts of an E/M service.
While the E/M updates will relieve providers of the burden of duplicating documentation, it also comes with modifications to how services for new and established office/outpatient visit Levels 2 through 4 will be reimbursed. Table 1 represents the latest payment model from CMS in a presentation of the 2019 Final Rule.2
Table 1.
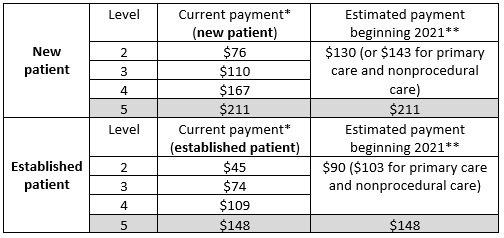
*Current payment for CY 2018
** Estimated payment based on the CY2019 finalized relative value units and the CY2018 payment rate
It would be beneficial to review revenue generated from each E/M level to determine how this change will affect your practice.
Several groups have opposed pairing this restructuring of payment rates with the documentation reduction. The American Hospital Association (AHA) submitted comments to CMS on the proposed rule last year stating, “By reducing payments for many providers, the proposal to collapse the payment rates for E/M visits devalues providers’ time, increasing the already heavy pressure they face to maximize the number of patients they see each day.”3
The American Medical Group Association (AGMA) agrees, stating that CMS is confounding two separate issues.
While CMS does not expect all specialties to experience a loss in revenue, they have proposed new add-on codes with reimbursement to be billed with codes 99202 through 99215 to help mitigate some of the effects of the new E/M payment structure. To date, CMS has proposed primary care add-on codes GPC1X “Visit complexity inherent to evaluation and management associated with primary medical care services that serve as the continuing focal point for all needed health care services” and GCG0X, “Visit complexity inherent to evaluation and management associated with endocrinology, rheumatology, hematology/oncology, urology, neurology, obstetrics/gynecology, allergy/immunology, otolaryngology, or interventional pain management-centered care.”
Prolonged services codes 99354 and 99356 will be revised to exclude reporting for “office or other outpatient setting” in order to make room for new prolonged services codes yet to be determined, to report prolonged service in the office and outpatient setting. CMS has proposed add-on code GPRO1, “Prolonged evaluation and management or psychotherapy service(s) beyond the typical service time of the primary procedure in the office or other outpatient setting requiring direct patient contact beyond the usual service; 30 minutes”; that is also expected to go into effect on January 1, 2021.
As these changes take effect as anticipated over the next few years, you can expect a substantial disruption to how E/M services are documented, coded, and billed. These changes in coding will apply across all payers. However, private payers will likely take some time to implement changing fee schedules for these codes.
References
- American Medical Association. CPT editorial summary of panel action February 2019. Available at: https://www.ama-assn.org/system/files/2019-03/february-2019-summary-panel-actions_0.pdf. Accessed May 10, 2019.
- Centers for Medicare and Medicaid Services. Calendar year (CY) 2019 Medicare physician fee schedule (pfs) final rule. Available at: https://www.cms.gov/About-CMS/Story-Page/CY-19-PFS-Final-Rule-PPT.pdf. Accessed May 10, 2019.
- American Hospital Association. AHA Comments on physician fee schedule proposed rule for CY 2019. Available at: https://www.aha.org/news/headline/2018-09-07-aha-comments-physician-fee-schedule-proposed-rule-cy-2019. Accessed May 10, 2019.
