Urgent message: While alarming to parents, febrile seizures in children typically are benign and self-limited. However, the possibility of a life-threatening etiology mandates that the urgent care provider determine the type of seizure and employ appropriate assessments based on factors specific to each case.
Tiffany Addington, MD
CASE
A previously healthy 3-year-old boy presented to urgent care after having a seizure at home. He had a fever that morning and was given ibuprofen. His mother also reports he had one loose stool. While resting on the floor watching television, his whole body stiffened and began jerking in a rhythmic pattern. This continued for 2-3 minutes before subsiding. Following the event, the child was minimally responsive and limp. His mother loaded him in the car and headed to the urgent care. On physical examination, he had a temperature of 38.9°C, blood pressure 88/45 mmHg, heart rate 132 beats/min, and respiratory rate 36 breaths/minute. His overall general and neurologic exams were unremarkable by the time he arrived.
CONDITION OVERVIEW
Febrile seizures are the most common type of epileptic event in children.1 The American Academy of Pediatrics defines febrile seizure as convulsions in febrile children between the ages of 6 months and 60 months who have no identified intracranial or metabolic cause or afebrile seizure history.2-4 Febrile seizures occur in 2%-5% of children under the age of 5, with the peak incidence at 18 months. They occur slightly more in males than in females.1-4 The specific cause of febrile seizure remains unknown.5
DIFFERENTIATING SEIZURE TYPE BY HISTORY/EXAM
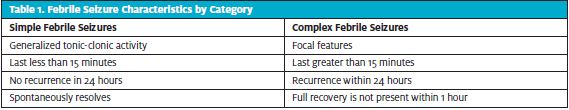
The history and physical exam are critically important for the urgent care provider in differentiating a seizure that carries little risk from a seizure or other movement episode that requires further evaluation. Diagnosis of febrile seizure requires detailed history-taking with close attention to the length of the event, nature of the jerking movements, illness symptoms, recent vaccinations, family history of seizures (with or without fever), and patient’s medical history.1,3-6 Febrile seizures can be categorized as simple or complex.
Simple febrile seizures account for two-thirds of pediatric febrile seizures.3,5 They are defined as occurring for less than 15 minutes, with seizure activity characterized as generalized convulsions with no return of seizure activity within 24 hours and no neurologic disease.2-4,7 While alarming for parents, they are generally benign, and a majority of children have an excellent prognosis.5
Complex febrile seizures are focal, prolonged (occur for greater than 15 minutes), and associated with a postictal neurologic abnormality and/or return of seizure activity within 24 hours.3,4 (See Table 1 for differentiating characteristics.) There is a subset of complex febrile seizures called febrile status epilepticus, defined as a complex febrile seizure lasting more than 30 minutes; these account for approximately 5% of febrile seizures.1,3 Prognosis for each of these categories will be discussed later.
In addition to an accurate description of the seizure to differentiate seizure-type, a thorough history and physical exam are important to help localize a possible source for the fever.4,5 History of recent vaccinations is also important to ascertain because certain vaccines carry a risk of postvaccination febrile seizure.3,6 With respect to that, families need to receive education about the significant risk for morbidity in children who are not immunized against the diseases a vaccine is intended to prevent.6,8
Physical Examination
Patients presenting with febrile seizure often have or have had a fever greater than 38°C.4 Completing a full physical examination can help identify the underlying illness, such as upper respiratory infection, otitis media, pneumonia, gastroenteritis, roseola, or influenza. Fever source is often unidentified.3 Physical examination for these patients should include assessment for meningeal signs, as well as serial neurologic evaluations; these will be valuable throughout the child’s medical care.3,7
DIAGNOSTICS
Bloodwork
Routine serum diagnostic testing is discouraged in evaluation of children with simple febrile seizures, and there are no evidence-based guidelines for complex febrile seizures in an otherwise healthy child. Therefore, studies such as CBC, BMP, Ca, Mg, and glucose levels after simple febrile seizure in patients over 6 months of age are of limited value unless there are history or physical exam findings which lead to concern about investigating these values.1,2 Afebrile seizure, children with symptoms of intracranial infection, first complex febrile seizure for an infant less than 1 year of age, or children with an illness associated with significant vomiting or diarrhea are a few examples of when these studies may need to be completed.1,5 Generally, serum testing is unnecessary in the evaluation of febrile seizures.
Urinalysis
Urine studies are to be completed depending on gender, age, and standard guidelines for urinary tract infection evaluation.3
Lumbar Puncture
The American Academy of Pediatrics (AAP) developed specific guidelines for lumbar puncture following simple febrile convulsions for children 6 months to 60 months of age.2 Regardless of patient age, the AAP recommends lumbar puncture for any patient who presents with meningeal signs/symptoms or whose history or exam is concerning for meningitis or central nervous system infection.2 See Table 2 below for additional guidelines.
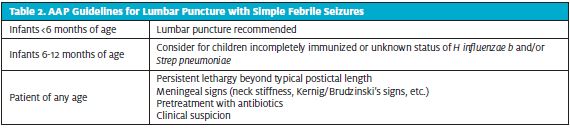
The recommendation to consider lumbar puncture for children ages 6 months to 12 months with incomplete Haemophilus influenzae or Streptococcus pneumoniae vaccination or with unknown immunization status is founded in the high morbidity and mortality of bacterial meningitis in this population if it is not treated.2 Clinicians should also consider lumbar puncture for children with fever and seizure who were recently exposed to systemic antibiotics to evaluate for partially treated meningitis.2 The extent of this impact relates directly to the specific antibiotic and would include dosage, form of administration, central nervous system penetration, and underlying infectious cause of the meningitis.2,3
These guidelines do not apply to patients with complex febrile seizures, history of afebrile seizures, central nervous system abnormalities, or neurologic injury.2 While no specific AAP guidelines for a lumbar puncture following complex febrile seizure exist, a lumbar puncture could be considered for patients with prolonged mentals status change, critically ill patients, or symptoms of an infection of the central nervous system.2
Neuroimaging
Since there is an extremely low likelihood of finding an underlying structural cause of simple febrile seizures, the role of neuroimaging is very limited. Plain skull x-rays are of no value and the AAP does not support routine CT or MRI imaging for patients with simple febrile seizures.1,2 Since CT imagining results in significant radiation exposure, and because MRI imaging often requires sedation, there may be more risk to performing these procedures than not.2 CT imaging should be considered when there is risk of trauma or evidence of increased intracranial pressure.1 MRI scans may have a role for children with complex febrile seizures after consultation with a neurology specialist.1
EEG
Routine EEG is not indicated for assessment of healthy patients with simple febrile seizure because it does not assist in diagnosis or management, nor does it help determine recurrence or epilepsy risk.1,2 There are no specific guidelines on the value of routine use of EEG in the evaluation of children with complex febrile seizures, but this can be considered in consultation with a neurology specialist.3
MANAGEMENT
For simple febrile seizures where the child is back to their neurologic baseline, the main priorities are to look for a potential cause of fever and to provide reassurance and education for the family. Intervention is rarely necessary since most febrile seizures are self-limited.1
Providers can consider benzodiazepine medication management for seizures that do not resolve within 5 minutes.1,3,8 Diazepam or lorazepam can be administered IV or IM. Diazepam can also be administered rectally. Midazolam can be administered by buccal or intranasal route with similar efficacy.1,3 If the first dose of these medications is ineffective, status epilepticus treatment protocol initiation is recommended.1
Consultation with a neurologist or referral to a pediatric emergency department may be a consideration for children who present with complex febrile seizures by history.
For infants or children who are post-ictal, it is important to provide supportive care and ensure the child returns to their neurologic baseline. If the child has more seizures, has focal deficits, or does not return to their neurologic baseline, then further evaluation is necessary.8 Other concerning signs that require hospitalization include meningeal signs, high risk of seizure recurrence, respiratory distress, persistent neurologic findings (ie, Todd’s paresis), petechial or purpuric rash, or possible serious infection.5
Antipyretics can be utilized to treat fever in children who have symptoms associated with their fever.5 These medications do not decrease recurrence rates and should not be administered routinely or preventatively. It is essential for medical providers to explain the antipyretic is not to control or prevent the seizure but to address symptoms of pain or fussiness associated with fever.3,5
Healthcare professionals must also recognize that febrile seizures are overwhelming and terrifying for parents to witness.5 It is extremely important to educate and reassure families about the overall benign nature of simple febrile seizures.3 In addition, counseling parents about the value of first aid during seizure activity can empower families to effectively keep the child safe during the event. Medical providers can also provide information to the family about when to contact their physician and when to take the child to the emergency department.1,5
Long-term/continuous treatment with antiepileptic medications in prevention of recurrent febrile seizures is not recommended due to the risk of adverse reactions associated with these medications being greater than its benefit in this population.3,5,7,8
Home Education
All families should receive education in case a seizure recurs with this or a future illness. Family management of febrile seizures at home involves keeping the child safe during seizure activity, as well as knowing when to contact emergency services or the primary care physician.5
Families can keep children safe during seizure activity by positioning the child on their side at the level of the floor, removing any sharp objects. Do not place anything in the child’s mouth. Expert consensus counsels on providing rectal diazepam to families for home administration for febrile seizures lasting more than 5 minutes.3 Medical professionals may consider prescribing rectal diazepam for emergency use at home if the child is at high risk for prolonged or multiple febrile seizures or the family does not live near a medical facility.1
PROGNOSIS
Simple febrile seizures are generally benign in nature, without lasting effects.1,2 They are often self-limited and will stop without intervention. 1,5 Simple febrile seizures do not cause intellectual disabilities and they are not an indication of epilepsy.2
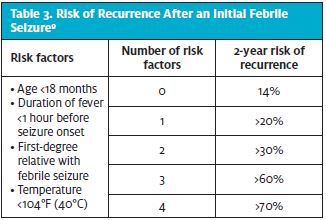
Understanding both risk of recurrence and risk of epilepsy following a febrile seizure can assist medical professionals in effectively educating families at time of discharge from medical care. The rate of recurrence for a second febrile seizure is between 30% and 40%, with risk decreasing to 10% for a third or more subsequent febrile seizure.1-4,6 Risk of recurrence is higher in those children who have a shorter duration of fever before seizure (<1 hour), lower peak temperature, family history of simple febrile seizures, or first febrile seizure occurring at less than 1 year of age.1,3 (See Table 3.) Family history of simple febrile seizures is the only risk factor for both initial febrile seizure and risk of febrile seizure recurrence.1
The risk of a child developing epilepsy after a simple febrile seizure is comparable to the risk of epilepsy in the general population (estimated to be around 2%-3%).1,3-4 Patients at risk for epilepsy include those with a family history of epilepsy, those who have a complex febrile seizure/febrile status epilepticus, recurrence of simple febrile seizure at less than 1 year of age, and those who have neuromotor developmental abnormalities at baseline.1,3
CASE CONCLUSION
This patient’s fever and fussiness improved with ibuprofen during his urgent care visit. His activity had returned to baseline and physical exam remained unremarkable. No diagnostic testing was required, and he did not have any clinical symptoms or signs requiring inpatient management. He was diagnosed with simple febrile seizure, with fever cause likely due to viral gastroenteritis. He was discharged home with instructions on first aid for febrile seizures, supportive care for viral gastroenteritis, and fever management.
REFERENCES
- Shinner S, Glauser TA. Febrile seizures. J Child Neurol. 2002;17(1-suppl):S44-52.
- American Academy of Pediatrics Subcommittee on Febrile Seizures. Clinical Practice Guideline—Febrile Seizures: Guideline for the Neurodiagnostic Evaluation of the Child with a Simple Febrile Seizure. Pediatrics. 2011;127:389-394.
- Kimia AA, Bachur RG, Torres A, Harper MB. Febrile seizures: emergency medicine perspective. CO-Pediatrics. 2015;27(3):292-297.
- Renda R, Yüksel D, Yavuz Gürer YK. Evaluation of patients with febrile seizure: risk factors, recurrence, treatment and prognosis. Pediatric Emerg Care. 2020; 36(4):173-177.
- Laino D, Mencaroni E, Esposito S. Management of pediatric febrile seizures. Int J Environ Res Pub Health. 2018;15(10):2232.
- Duffy J, Weintraub E, Hambidge SJ, et al. Febrile seizure risk after vaccination in children 6 to 23 months. Pediatrics. 2016;138(1):e20160320.
- Bashiri FA. Childhood epilepsies: what should a pediatrician know? Neurosciences. 2017;22(1):14-19.
- Patel AD, Vidaurre J. Complex febrile seizures: a practical guide to evaluation and treatment. J Child Neurol. 2013;28(6):762-767.
Author affiliation: Tiffany Addington, MD, Children’s Mercy Urgent Care East; University of Missouri-Kansas City School of Medicine; University of Kansas School of Medicine.
