Resolution
- Pneumonia
- Pneumothorax
- Heart failure
- Pulmonary embolism
- Lung cancer
Physical Examination
On examination, the patient was found to be afebrile, and he had a pulse rate of 98 beats/min, a respiration rate of 24 breaths/min, and a blood pressure of 142/88 mm Hg. He was alert and oriented. The physician noticed tachypnea when the patient walked from the waiting room to the examination room.
The patient had decreased breath sounds bilaterally with minimal bilateral symmetric wheezing. He had a regular heart rate and rhythm without murmur, rub, or gallop. His abdomen was soft and nontender without rigidity, rebound, or guarding. He had no pain or swelling of the lower extremities.
Resolution
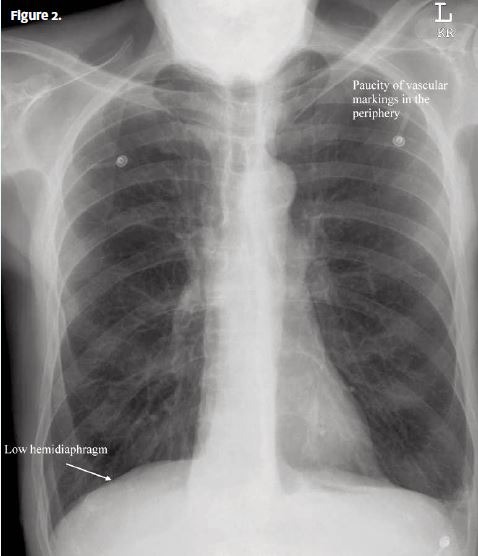
His peripheral pulses were 2+ on a scale of 0 to 4 and were equal in all four extremities. The patient’s chest x-ray had the typical appearance of chronic obstructive pulmonary disease (COPD): large, dark lungs; flattened thoracoabdominal diaphragm; and a small, vertically oriented heart (Figure 2).
Diagnosis
The diagnosis was COPD.
Learnings
COPD affects 30 million Americans and is the fourth leading cause of death in the United States. Airway obstruction is present in 14% of white male smokers, compared with 3% of nonsmokers. COPD classically encompasses several diffuse pulmonary diseases, including chronic asthma, bronchiectasis, chronic bronchitis, cystic fibrosis, and emphysema.
The American Thoracic Society defines COPD as the progressive development of airflow limitation that is not fully reversible.
Most patients with COPD have components of both chronic bronchitis and emphysema. Chronic bronchitis is characterized by a recurrent and productive cough on most days for ≥3 months in 2 consecutive years without another explanation. It is caused by obstruction of small airways. Emphysema results from the destruction of interalveolar septa characterized as having abnormal, permanent enlargement or air spaces distal to the terminal bronchiole without obvious fibrosis. It is caused by enlargement of air spaces and destruction of lung parenchyma, loss of lung elasticity, and closure of small airways.
The medical history should record consideration of fever, cough, dyspnea, chest pain, peripheral edema, and a change from baseline (chronic) symptoms. Inquire about the use of home oxygen and about current or past use of cigarettes.
The physical examination often reveals acute decompensation that is evident when the patient first enters the room, and there is often evidence of tachypnea, diaphoresis, or altered consciousness. Other findings such as the use of home oxygen, pursed-lip breathing, use of accessory muscles, and periorbital cyanosis may indicate impending respiratory failure. The lung examination typically reveals decreased lung sounds with a prolonged expiratory phase, and symmetric wheezing. The extremities should be evaluated for edema and the presence of symmetric pulses.
COPD exacerbations can be safely treated on an outpatient basis with a combination of antibiotics, steroids (inhaled or systemic), and _2-agonist inhalers. Antibiotics decrease the risk of clinical failure.
Immediate referral to an emergency department is necessary if any of the following are present:
- Respiratory distress
- An oxygen saturation of <90%
- Hemodynamic instability
- The possibility of an alternative diagnosis such as pulmonary embolism, pneumonia, pneumothorax, or myocardial infarction