Published on
Urgent message: Embedding a clerical component within a relationship-based care approach has been shown to improve both financial outcomes and patient satisfaction.
Noel Clinton, BS
Introduction
When we hear the term “relationship-based care,” we tend to think first about the relationship between the clinical staff and the patient. However, a prospective program as Bassett Healthcare in Cooperstown, NY has shown that positive patient care and improved financial outcomes are also a result of developing a “bedside” business relationship.
Bassett Healthcare Network is a system of physicians, providers, and hospital community health centers covering 5,000 square miles in eight New York counties. Around the region, the network provides primary, preventive, and outpatient care at 28 health centers – including urgent care at facilities in Herkimer and Oneonta, NY – and operates 13 school-based health centers.
The Emergency and Trauma Services Department for Bassett is responsible for providing the professional staff for this entire network, and implemented a process in which clerical staff imitate contact with patients at specific points during a visit.
Background
Significant growth within the network led to the addition of a management position whose mandate was to carry the department’s patient care approach to the operation level. The primary focus for this individual, initially, was to deal directly with patient complaints. The ability to listen to patients in a non-judgmental manner and “getting to ‘yes’” was the building block for learning about patient expectations.
Consistent and visible support helped establish trust and respect with the individual affiliates’ leadership teams, paving the way for processes to be standardized.
Historic and internal data from a callback program and patient complaints illuminated inroads to improving the patient experience. The network manager assembled a multi-location team to review that data and investigate opportunities to improve processes within patient flow.
A nursing and business representative was asked to participate in a series of meetings that resulted in the “Fantasy Flow Workgroup.”
Care Delivery
Planning began with defining individual and unique needs and responsibilities for each unit, while mapping out the overall common themes needed for the patients.
The “deep dive” on the data showed the following:
- Patients felt staff was not spending adequate time with them.
- Arrival rates, patient volumes, and increased acuity were having significant impact on length of service time and nursing ratios.
- The urgent care location faced increased demand – up to 17% new growth each year.
- Less than 48% of patients followed discharge instructions.
- Patients were choosing to not fill their prescriptions or schedule the recommended follow-up appointment at an unacceptable rate.
This information was highly relevant to quality of care, and raised several important questions:
- If there was more time to be spent with a patient, where would it be best spent?
- How do we install in our patients the value of following our instructions?
- How can we assist the patient in being compliant?
Billing and cost of care were primary themes of complaints that we heard. however, once we really listened, we learned that in addition to the fear of inability to pay, patients were uncertain how to navigate the healthcare system for follow-ups (e.g., appointments, prescriptions, insurance referrals.).
Resources
Once the Fantasy Flow Group began mapping out the patients’ experiences, it became evident quickly that the missing link in our patient’s experience was with our clerical staff.
Historically, the “regular” check-in process was public, rushed, and impersonal. The checkout process at some of our locations was nonexistent.
Rather than simply instructing clerical staff members to interact with patients during a visit, the nursing representatives coached them on how to relate to a patient at bedside. This was a new approach to our interactions with patients – and a cultural change for both staff and patients. This truly was our department’s first experience with the relationship-based care model in action.
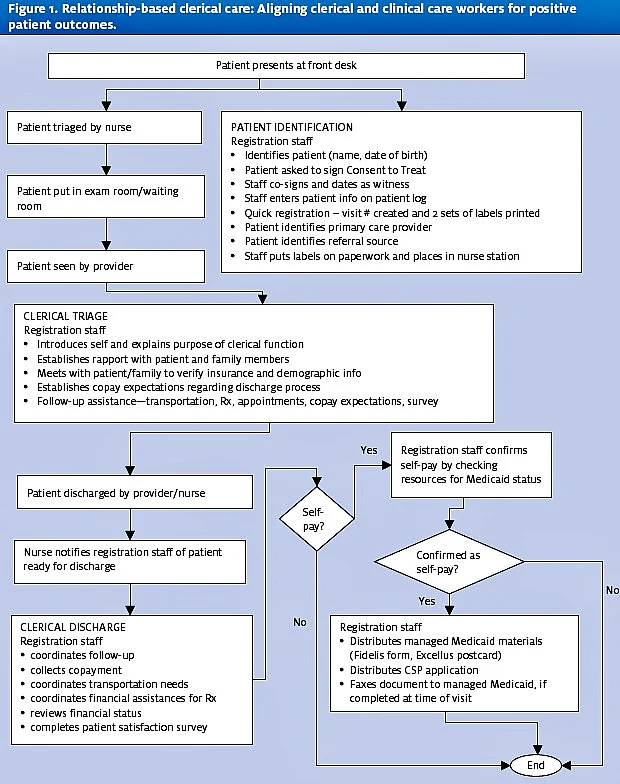
Our location all fall under Emergency Medical Treatment and Active labor (EMTALA), so we targeted the “clerical triage” to occur after the medical screening examination.
The initial interaction between the patient and the urgent care representative focused on introduction and setting expectations. Confirming demographics and insurance were weaved into the process. The patient was given a verbal outline of what assistance would be provided to them at the end of the visit and a commitment to be there with them, either literally or symbolically, throughout the process.
it is in the discharge process that full customer service and attention is placed in the hands of the representative. That process included scheduling follow-up appointments, making transportation arrangements, offering financial programs for prescription, collection of copayments, review of financial insurance status, and completion of a patient satisfaction survey.
The entire process is outlines in Figure 1.
The network manager tested the mapped process by filling the role a staff member would play over a three-month period, cycling through different days and times of the week. Time studies were conducted on all aspects of the expectations for this role, and then tasks were prioritized. A job description was written, graded, and approved through the human resources department. Senior leadership approved a temporary position and recruitment began. A successful candidate was hired and trained by the network manager.
Outcomes
Key indicators – outcome measures, to use a clinical research term – that would reflect a positive impact on the patient’s experience needed to be determined for this newly created bedside business relationship. These indicators needed to have the ability to motivate senior leadership to grant the position full-time status.
The best way to report results to administration is to use the tool they created, the Annual Operating Plan. The reference points outlined for the bedside clerical relationship were designed to fit into the corresponding matrix (Table 1).
The implementation of this new bedside process brought the patient relationship full circle. The concentrated focus on the clerical triage and clerical discharge process resulted in decreased billing complaint rates and high satisfaction scores (defined as meeting/exceeding expectations), and facilitated service excellence.
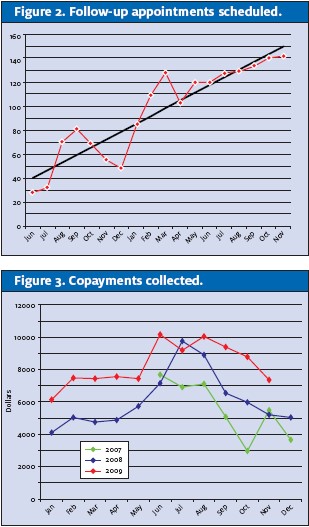
It also produced the desired results in two key outcome measures: follow-up appointment scheduled (Figure 2) and copays collected (Figure 3).
Finally, changing the culture to include clerical staff in the delivery of care has changed our relationship with the patient. In addition to the positive financial outcomes, patients are more compliant with instructions.
| Table 1. | ||||
| Reference point | Date to be collected | Method/source/who collects | Tracking/trending results | |
| Program growth & opportunity Expand primary care across network |
Market share development: identify patients within the ED requiring a follow-up appointment who do not have an established primary care provider | Number of appointment made for patients without a primary care provider | At each patient encounter, rep indicates follow-up information in access database Information reported to network manager monthly |
Data reviewed and additional work plans generated; e.g., request for direct access to primary care at main campus |
Service delivery
|
Access, access, access
|
Number of appointments made for patients at the time of discharge |
|
Develop e-messaging between locations as it relates to “clerical communication” |
| Finance Attain long-term financial strength |
|
|
|
|
