Published on
Differential Diagnosis
- Atrial flutter with intermittently paced beats
- Inferior STEMI
- Wolff Parkinson White
- Third-degree AVB
- Sinus bradycardia
Diagnosis
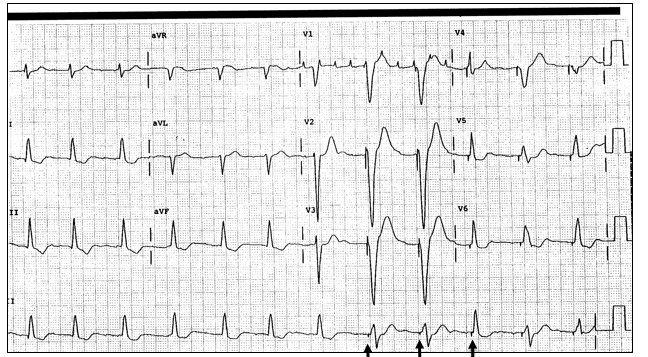
This woman was diagnosed with atrial flutter with intermittently paced beats.
The ECG reveals a regular rate of approximately 70 beats per minute.
Sinus bradycardia is a rate <60 beats per minute.
There is no evidence of ST elevation in the inferior leads (II, III, aVF).
The ECG of Wolff Parkinson White reveals a gradual upsloping of the initial reflection of the QRS complex, called delta wave, and additional ECG finds may include a shortened PR interval (<120ms), a widened QRS complex, and ST/T wave changes; these changes are not present on this ECG.
In third-degree AV block, there is dissociation between atrial and ventricular depolarizations; again, not present here.
This ECG shows pacer spikes consistent with an intermittently paced ECG with an underlying rhythm likely atrial flutter, as evidenced by flutter waves in leads V1 and V2.
Learnings/What to Look for:
- Pacer spikes may occur with every beat or be “demand” (ie, present only when the pacemaker senses a need to fire, as present in this ECG; see the lead II “rhythm strip” at the bottom of the ECG)
- Atrial flutter is a regular rhythm and often present in patients with a history of atrial fibrillation
- The “saw tooth” pattern is best seen in leads II and V1. These are the atrial depolarizations and are usually blocked 2:1, leaving a rate which is often 150
- As with atrial fibrillation, atrial flutter confers a risk of CVA, so the need for anticoagulation should be considered
Pearls for Urgent Care Management and Considerations for Transfer
- Establish the presence of a pacemaker with the patient and compare with an old ECG
- If the patient has an automatic implantable cardiac defibrillator (AICD) and there are intermittent shocks occurring, it will need to be emergently interrogated in the ED or with their cardiologist
- In patients with palpitations, chest discomfort, shortness of breath, diaphoresis, weakness, or dizziness and if present, consider emergent ED referral to evaluate for ischemia/infarction or electrolyte abnormalities
- Asses vitals for signs of hemodynamic instability such as tachycardia, hypotension, dizziness, or confusion
- If there is concern for ischemia, transfer to the ED for emergent evaluation