Published on
Urgent message: Chief complaints may lead the provider “off the trail” of a more urgent diagnosis. Anchoring bias occurs when relying too heavily on this first piece of information. Providers must remain vigilant for the subtle and nonspecific warning signs of pulmonary embolism.
Ryan Hagan, PA-C and Christina Gardner, DHSc, MBA, PA-C
INTRODUCTION
Chief complaints are used to guide decision-making and may suggest an organ system, but a life-threatening condition may be found in a different organ system. Addressing the patient’s concern might satisfy her, but a careful history and exam can reveal a must-not-miss diagnosis. Pulmonary embolism is a potentially life-threatening condition that may present subtly with nonspecific signs or symptoms. Risk factors such as a recent orthopedic surgery should raise the index of suspicion of a must-not-miss diagnosis.
CASE PRESENTATION
Mrs. Q is a 75-year-old female whose chief complaint in the urgent care is “black stools” associated with fatigue and lightheadedness for 4 days.
- Medications: Aspirin, meloxicam, and a multivitamin with iron daily
- Personal medical history: Significant for diverticulitis, colitis, and hemorrhoids
- Past surgical history: Total knee arthroplasty performed 5 weeks ago
- Social history: Former smoker, drinks three glasses of wine per week
- Review of systems: Denies frank bleeding, hematemesis, N/V/D or abdominal pain
- Physical exam/vital signs:
| BP | 180/90 |
| Resp | 18 |
| Pulse | 90 |
| SpO2 | 99% on RA |
| Temp | 99⁰F |
Heart and lung sounds are normal, abdomen is soft and nontender, and she is well-appearing. Stool guaiac is negative for blood.
- MDM/UC course: During the exam she becomes acutely tachypneic at a rate of 24 breaths per minute. Further examination reveals her right knee is swollen, red, tender, and warm. Mrs. Q did not mention her knee symptoms because she attributed these to normal postoperative healing.
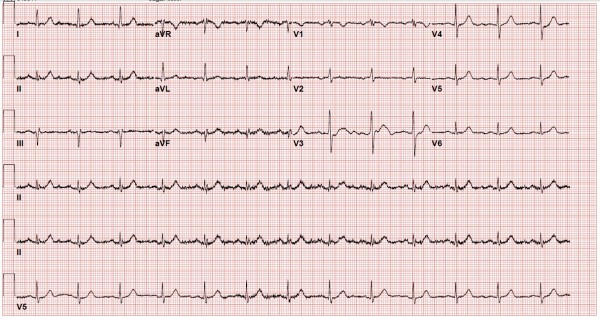
- Testing: A STAT EKG showed normal sinus with no ST or T wave abnormalities (Figure 1).
- MDM: Mrs. Q has a Well’s score for PE of 6 (moderate). With clinical gestalt, her risk for PE is moderate-to-high, and she requires transfer to the emergency department.
Differential Diagnosis
EMS transported the patient to the ED where ultrasound showed a right lower extremity DVT. Her chest x-ray was normal, and a CTA chest revealed bilateral pulmonary emboli. The patient was admitted for bilateral pulmonary emboli and treated with heparin. She transitioned to apixaban (Eliquis) prior to discharge 2 days later. Gastroenterology was consulted for the chief complaint, but endoscopy was not indicated as her hemoglobin was stable and the guaiac test was negative. At her PCP follow-up, she was doing well and denied any signs of GI bleeding.
| Differential Diagnosis for Pulmonary Embolism |
| Acute coronary syndrome Anemia Angina pectoris Hypersensitivity pneumonitis Mitral stenosis Myocardial infarction Pericarditis Pneumonia Pneumothorax Pulmonary hypertension |
DISCUSSION
Overview
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are two manifestations of the same disease known as venous thromboembolism (VTE); 47% of patients with PE have signs of DVT.1 Virchow’s triad describes three pathways to thrombus formation: endothelial damage, stasis, and hypercoagulation. Major orthopedic surgery involves endothelial injury, and stasis occurs with immobilization on the operating table and during bed rest. Thus, at least two elements of the triad are present with total knee arthroplasty (TKA).
At baseline, major orthopedic surgeries like TKA place individuals at high risk for VTE.2 The risk is further increased when there is older age, prior VTE, malignancy, cardiac disease, thrombophilia, longer duration of anesthesia, or prolonged immobilization.3
Providers mitigate risk by utilizing pharmacological and mechanical prophylaxis. These include heparin, direct oral anticoagulants (DOACs), pneumatic compression devices, graduated compression stockings, venous foot pumps, and ambulation.
Although thromboprophylaxis reduces risk of VTE in the immediate postoperative period, the risk following total knee or hip arthroplasty extends past the 7 or 10 days of hospital admission.4 The risk is highest during the first 5 weeks post-op.5 The cumulative incidence of DVT and PE for 3 months following TKA is 2.1%.2
Presentation
A postoperative patient with acute and unexplained dyspnea is classic for PE. However, symptoms may vary markedly, ranging in severity from no symptoms to shock or sudden death. Dyspnea is the most common symptom followed by pleuritic chest pain. Table 1 shows the most common signs and symptoms among patients with no prior cardiopulmonary disease according to the PIOPED II study.1
| Table 1. Signs and Symptoms for PE Without Prior Cardiopulmonary Disease | |
| Symptom | Frequency |
| Dyspnea | 73% |
| Pleuritic pain | 44% |
| Calf or thigh swelling | 41% |
| Cough | 34% |
| Wheezing | 21% |
| Sign | |
| Tachypnea | 54% |
| DVT signs in calf or thigh | 47% |
| Tachycardia | 24% |
| Rales | 18% |
| Increased P2 heart sound | 15% |
Diagnostics
The most validated decision rules are the Geneva score and Well’s score.6 For low-risk patients, the PERC rule can be used to rule out PE.7 In these cases, providers may avoid using a D-dimer test.
Low D-dimer levels may be useful to rule out PE when used together with clinical decision rules, but this test is not specific.8 While D-dimer levels are elevated with VTE, they can also be elevated in surgery, cancer, trauma, renal disease, or age. In patients with recent TKA, D-dimer has limited usefulness. It has shown to always be elevated in the first week following hip and knee replacement.9 When there is high probability of VTE, D-dimer may only waste time and resources leading up to CTA scanning.
A normal chest x-ray in the setting of hypoxia should raise suspicion for PE. The chest x-ray may show atelectasis or pleural effusion.6 In rare cases, the specific signs of Hampton’s hump (a lateral, dome-shaped opacity) or Westermark sign (oligemia distal to a large vessel occluded by a PE) can be observed. Chest x-ray is more useful for detecting alternative diagnoses than signs of PE.
EKG can be useful in diagnosing PE. The most common EKG abnormalities are sinus tachycardia and nonspecific ST or T wave abnormalities. One study found tachycardia is present in 45% of cases.6 A normal heart rate is common. Right bundle branch block and S1Q3T3 are suggestive but not common. In less than 10% of cases, the S1Q3T3 pattern may be observed showing deep S waves in lead I, and deep Q waves and inverted T waves in lead III.10 Neither chest x-ray nor EKG can reliably rule out PE.11,12 Definitive diagnosis of PE is made with CT pulmonary angiography or ventilation-perfusion scanning.
Disposition
All patients with suspected PE should be transported to an emergency department. Following diagnosis, anticoagulation is initiated and patients are observed for complications.
References
- Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879.
- White RH, Romano PS, Zhou H, et al. Incidence and time course of thromboembolic outcomes following total hip or knee arthroplasty. Arch Intern Med. 1998;158(14):1525-1531.
- Jaffer AK, Barsoum WK, Krebs V, et al. Duration of anesthesia and venous thromboembolism after hip and knee arthroplasty. Mayo Clin Proc. 2005;80(6):732-738.
- Leclerc JR, Gent M, Hirsh J, et al. The incidence of symptomatic venous thromboembolism during and after prophylaxis with enoxaparin: a multi-institutional cohort study of patients who underwent hip or knee arthroplasty. Canadian Collaborative Group. Arch Intern Med. 1998;158(8):873-878.
- Caron A, Depas N, Chazard E, et al. Risk of pulmonary embolism more than 6 weeks after surgery among cancer-free middle-aged patients. JAMA Surg. 2019;154(12):1126-1132.
- Righini M, Robert-Ebadi H, Le Gal G. Diagnosis of pulmonary embolism. Presse Med. 2015;44(12 Pt 2):e385-e391.
- Singh B, Mommer SK, Erwin PJ, et al. Pulmonary embolism rule-out criteria (PERC) in pulmonary embolism—revisited: a systematic review and meta-analysis. Emerg Med J. 2013;30(9):701-706.
- Lucassen W, Geersing GJ, Erkens PM, et al. Clinical decision rules for excluding pulmonary embolism: a meta-analysis. Ann Intern Med. 2011;155(7):448‐460.
- Rafee A, Herlikar D, Gilbert R, et al. D-dimer in the diagnosis of deep vein thrombosis following total hip and knee replacement: a prospective study. Ann R Coll Surg Engl. 2008;90(2):123-126.
- Panos RJ, Barish RA, Whye DW Jr, Groleau G. The electrocardiographic manifestations of pulmonary embolism. J Emerg Med. 1988;6(4):301-307.
- Elliott CG, Goldhaber SZ, Visani L, DeRosa M. Chest radiographs in acute pulmonary embolism. Results from the International Cooperative Pulmonary Embolism Registry. Chest. 2000;118(1):33-38.
- Rodger M, Makropoulos D, Turek M, et al. Diagnostic value of the electrocardiogram in suspected pulmonary embolism. Am J Cardiol. 2000;86(7):807-A10.
Author affiliations: Ryan Hagan, PA-C, Carilion Clinic in Daleville, VA. Christina Gardner, DHSc, MBA, PA-C, Advanced ACP Fellowship in Urgent Care and Rural Health at Carilion Clinic; Radford University PA program. The authors have no relevant financial relationships with any commercial interests.

