Published on
Urgent message: Anaphylaxis is a true medical emergency that requires rapid and aggressive treatment. When a patient with a Type 1 hyper – sensitivity reaction is brought to your urgent care, here is how to proceed.
DAVID WEIN, MD, MBA, FACEP, and DENNIS DIXON, MD
Introduction
Anaphylaxis is a severe, whole-body, allergic reaction to a chemical that has become an allergen. Anaphylaxis is a true medical emergency, often with a rapid and unpredictable onset. It is commonly seen in young, otherwise healthy patients; without prompt medical intervention, it is potentially lethal. Fortunately, treatments for anaphylaxis are very effective and widely available. Overall, the risk of death from anaphylaxis has been estimated at around 1%, with 500-1000 deaths annually.1 Due to an unclear definition of the criteria for anaphylaxis, as well as poor reporting, the number of annual deaths may be significantly higher.1
Pathophysiology
Hypersensitivity reactions occur when a normal immune system responds in an excessive or undesirable way. Effects of these reactions vary from mild discomfort to death, depending on the type and severity of the reaction. According to the traditional Gell and Coombs classification, there are four types of hypersensitivity reactions2:
Type I (immediate) hypersensitivity reactions
Type 1 hypersensitivity reactions are immunoglobulin E (IgE)-mediated.2Often they are referred to as “immediate” hypersensitivity reactions because symptoms occur within minutes of exposure. Type I hypersensitivity reactions require a prior sensitization to an antigen, at which time IgE is formed and binds to mast cells and basophils. During subsequent exposures, cell-bound IgE is crosslinked by the antigen, leading to degranulation. Multiple mediators (histamines, cytokines, and leukotrienes) are then released, causing clinical symptoms.
Type II (cytotoxic) hypersensitivity reactions
Type II hypersensitivity reactions are caused by immunoglobulin M (IgM)- or immunoglobulin G (IgG)- binding cell-bound antigens, leading to complement activation and destruction of the cell.2 Examples include autoimmune hemolytic anemia, idiopathic thrombocytopenia purpura, and Goodpasture’s nephritis.
Type III (immune complex) hypersensitivity reactions
Type III hypersensitivity reactions are also mediated by IgM and IgG.2 In contrast to Type II reactions, circulating antigen-antibody complexes are deposited in capillaries, again leading to complement activation and cell destruction. Examples include serum sickness and systemic lupus erythematosus.
Type IV (delayed) hypersensitivity reactions
Type IV hypersensitivity reactions are mediated by T-lymphocytes,2 as opposed to antibodies. The most common example is contact dermatitis.
Clinical Syndromes
This article discusses Type I hyper- sensitivity reaction only, as this type of reaction is responsible for urticaria, angioedema, and anaphylaxis. While these manifestations may occur in isolation, it appears as though these findings are part of a continuum of the same spectrum of allergic disease.2 Urticaria is defined as raised, circumscribed areas involving the dermis and epidermis, which cause pruritis. Angioedema involves edema of subcutaneous and submucosal tissue secondary to increased vascular permeability. Typically for Type I hypersensitivity reactions, cutaneous symptoms are exceedingly common, seen in 90% of reactions.3 Respiratory symptoms are seen in 40%-60% of cases. GI and cardiovascular symptoms are less common, each only occurring in about 30% of cases.3
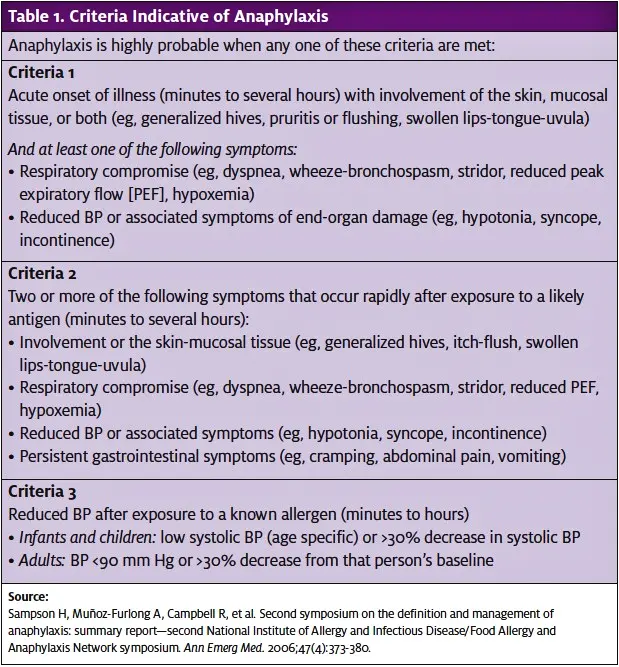
While we understand the common symptoms seen in anaphylaxis, no clear definition for anaphylaxis exists. In 2006, there was a consensus attempt to define anaphylaxis and its management; while no unified definition was agreed upon, it is thought that anaphylaxis is highly likely when any one of three criteria are met (Table 1).4
Anaphylaxis vs Anaphylactoid Reactions Anaphylactoid reactions are complement-mediated reactions that do not involve antibodies or prior antigen sensitization, as are seen in anaphylactic reactions.5 Clinically, it is virtually impossible to differentiate an anaphylactoid reaction from an anaphylactic reaction, but luckily treatment is the same for both.
Anaphylactoid reactions have a tendency to be dose dependent; patients who have an anaphylactoid reaction may not have a subsequent reaction if re-exposed to the offending agent. One of the most commonly seen anaphylactoid reactions is to radiocontrast media. At one time, it was thought that these were Type I hyper- sensitivity reactions to iodine, but they were later found to be anaphylactoid reactions caused by the hyperosmolar concentration of the radiocontrast media.5 These reactions are becoming less frequent with the development low-osmolality contrast solutions.
A number of protocols exist to prevent contrast- related anaphylactoid reactions in susceptible patients, and while they vary by institution, they generally include steroids plus antihistamines administered 1-13 hours prior to administration of the contrast media.5
Of note, while asthma and allergy history increase the risk for adverse reactions to contrast material, a history of shellfish or iodine allergy is not directly associated with reaction to contrast.5
Management of Anaphylaxis
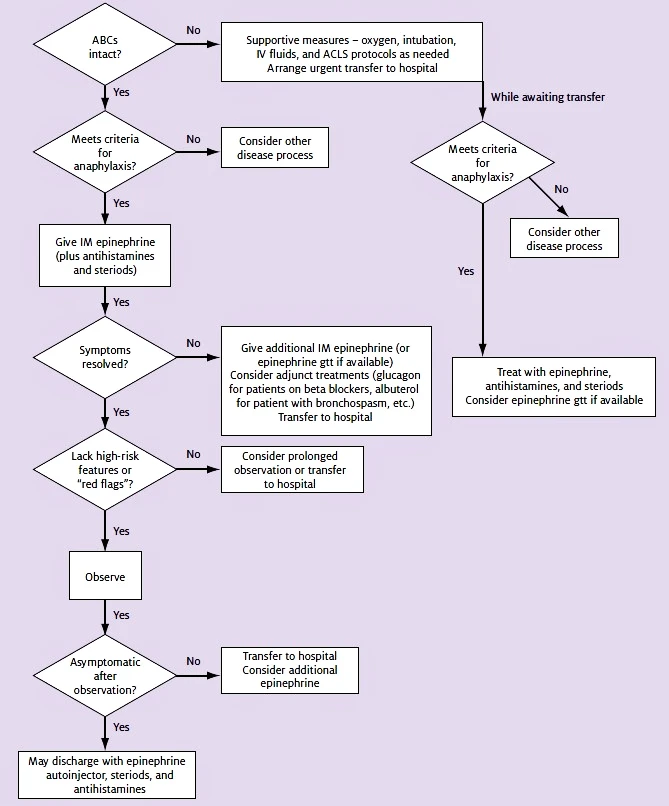
Management of anaphylaxis centers around the use of epinephrine, with antihistamines and steroids as adjunctive treatments (Figure 1).
Airway management and aggressive fluid resuscitation are also key to proper management. Special considerations should be made when treating patients with angioedema or those taking beta blockers. Important red flags are discussed on page 14.
Airway management
As in the management of any critical patient, ABCs (airway, breathing, and circulation) are the priority. Edema often leads to airway compromise, requiring intubation. Patients who do not show signs of impending airway compromise should be re-examined frequently, as they have the potential to decompensate rapidly. In an outpatient setting without airway capabilities, the patient should be transferred to a hospital if there is any sign of respiratory distress, as the potential for the patient to decompensate is high. Transfer of such a patient should occur with a transport team that has airway management capabilities.
Epinephrine is the drug of choice for the treatment of anaphylaxis.3,4,6 Patients meeting criteria for anaphylaxis should receive epinephrine. While there have not been any controlled trials on the use of epinephrine in anaphylaxis, recommendations are based on pathophysiology, animal models, and expert consensus guidelines.
In terms of safety, epinephrine has been used for many years and overall has been shown to be a very safe drug. Most complications have been related to the IV route and are primarily related to incorrect dosing. Perhaps some caution should be used in elderly or cardiac patients, especially when using the IV route.
There are no absolute contraindications to the use of epinephrine, although several theoretical con- traindications exist. In patients on beta blockers, the use of epinephrine can potentially lead to unopposed alpha stimulation, but most experts recommend using epinephrine in these patients, if needed. In fact, these patients sometimes require higher doses. (Patients on beta blockers are discussed in greater detail in Anaphylaxis on beta blockers on page 14.)
Most commercially available epinephrine contains sodium metabisulfite as a preservative, which could pose a problem to sulfite-allergic patients.7 Currently there is no consensus on treatment in this group of patients, but experts still recommend giving epinephrine in the setting of anaphylaxis.
Epinephrine should initially be given 0.01 mg/kg up to a maximal dose of 0.5 mg IM of 1:1000 dilution every 5-15 minutes as needed. Commercially available epi- nephrine autoinjectors are available in two doses: 0.3 mg (for patients over 30 kg) and 0.15 mg (for patients 15-30 kg). While epinephrine is often given subcuta- neously, the intramuscular route offers a more rapid and predictable absorption of the drug,4,8 as decreased peripheral blood flow during anaphylaxis is likely to decrease the efficacy of the subcutaneous route.
In addition, a prospective, randomized, blinded, placebo-controlled, six-way crossover study of intra- muscular vs subcutaneous injection of epinephrine in young men found that intramuscular injections in the thigh from an autoinjector had the best and most rapid absorption when compared to other methods of delivery.8 It is important to note that this study only measured serum epinephrine levels in healthy subjects following administration and was not outcome-based.
In general, the intramuscular route is the safest method of administration of epinephrine. However, if the patient continues to decompensate in spite of treat- ment, intravenous administration may be required.
Protocols regarding IV epinephrine have not been well established, and a debate remains over the best dilution to use. In the absence of a readily available, premade epinephrine infusion, it is easy to mix your own IV epinephrine using crash cart epinephrine, which is a 1:10,000 (100 mcg/mL) dilution; 1 mL of crash cart epinephrine contains 100 mcg of epinephrine. Dilute 1 mL of crash cart epinephrine into 9 cc of normal saline, making 10 mL of 1:100,000 (10 mcg/mL) epinephrine. This can be administered 0.5 mL-1 mL every 2-5 minutes as needed.
Antihistamines
Antihistamines are given routinely in anaphylaxis, but their effectiveness may be only minimal in the acute phase. They work mainly by preventing mast cell degran-lation, which with anaphylaxis has already occurred.4,6 The role of H1 blockers (diphenhydramine, hydrox- yzine) in allergic reactions has been well established. Of the commonly used H1 blockers, diphenhydramine is the only one that comes in an IV formulation. For an adult, the dose is 25 mg-50 mg IV; for a child, the dose is 1 mg/kg up to a maximal dose of 50 mg IV. Promethazine is another H1 blocker. In some countries it is used to treat allergic reactions, but in the United States it is reserved for use as an antiemetic.
In contrast to the use of H1 blockers, the use of H2 blockers is more controversial. It is thought that they may add a possible benefit when used in combination with an H1 blocker.4,6,9 H2 blockers are safe and fairly inexpensive, so there is little downside to giving them. Famotidine 20 mg IV, ranitidine 50 mg IV, and cimetidine 300 mg IV are commonly used adult doses.
In cases of anaphylaxis, the decision to give antihistamines should not delay administration of epinephrine. While antihistamines alone may be used to treat minor allergic reactions, they are not sufficient in cases meeting the criteria for anaphylaxis and should be used only as an adjunct to epinephrine therapy. Antihistamines may also play a role in treating biphasic reactions.
Corticosteroids
There is no role for steroids in the acute management of anaphylactic reactions because onset is delayed 4-6 hours. However, steroids may prevent protracted or biphasic reactions. If given, methylprednisolone should be administered 1 mg/kg-2 mg/kg IV.4
Adjunctive treatments
Oxygen should be administered to any patient with signs of respiratory compromise. Inhaled beta agonists (eg, albuterol) may have a role in continued bronchospasm refractory to epinephrine. In addition, aggres- sive IV fluid resuscitation is recommended early in the disease process. This is typically accomplished with isotonic crystalloid fluids (normal saline or Lactated Ringer’s Irrigation), administered in 20 mg/kg boluses under pressure.
Anaphylaxis on beta blockers There have been many reports of patients on beta blockers experiencing anaphylactic reactions that are refractory to the usual doses of epinephrine and who require higher doses. In these patients, glucagon may help as an adjunct to epinephrine.4,6 The initial dose is 1 mg-5 mg IV given over 5 minutes, followed by an infusion of 5 mcg/min-15 mcg/min.4 This dose of glucagon frequently can cause nausea and vomiting.
Angioedema
Angioedema due to ACE inhibitors is thought to be linked to increased bradykinin levels as a result of blocked breakdown mechanisms. Typically it is seen in the first week after starting treatment, but in some patients, angioedema has occurred months to years after starting treatment. In contrast to other type I hypersensitivity reactions, ACE inhibitor-induced angioedema lacks simultaneous urticaria. Management is generally accomplished with standard anaphylactic treatments, although no controlled trials have demonstrated efficacy of these treatments. The use of fresh frozen plasma (FFP) has been proposed, especially in cases refractory to other treatments.2
Another relatively common cause of angioedema is C1 esterase deficiency. It is hereditary and linked to increased bradykinin levels as a result of uninhibited production. Treatment generally involves FFP, although this is controversial. Standard anaphylactic treatments are ineffective.2
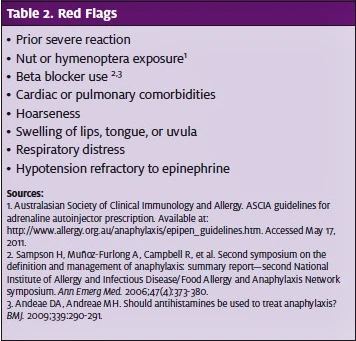
Red flags
There are several red flags to watch out for when evaluating a patient with anaphylaxis (Table 2). Previous history of a severe reaction, especially one requiring intubation or vasoactive substances, should be taken very seriously. Allergies to nuts and hymenoptera have a tendency to cause more severe reactions compared to other common allergens. As noted previously, patients taking beta blockers may experience symptoms refractory to epinephrine. Additionally, patients with cardiac or pulmonary comorbidities lack the reserve seen in healthier patients and have the potential to decompensate quickly. When examining the patient, hoarseness is caused by edema around the vocal cords and signifies impending airway compromise if not dealt with promptly. Any swelling of the lips, tongue, uvula, or oral mucosa may progress to airway obstruction. Lastly, a patient exhibiting hypotension at any time, especially if not responsive to the first dose of IM epinephrine, should be admitted to the hospital for observation, as these patients have the potential to do very poorly.
Disposition
Patients with severe anaphylactic reactions generally require hospital admission. Factors to consider include severity of symptoms, history of protracted or recurrent anaphylaxis, comorbidities (asthma, COPD, CHF, etc.), beta blocker use, extremes of age, and home/social sit- uation. Generally, in the outpatient setting, all but the most mild reactions should be transferred to the hospi- tal ED for further evaluation and observation. This can vary widely, depending on the ease of transport and out- patient facility capabilities.
Unfortunately, there are no good guidelines for dis- position of patients with mild or rapidly resolving symp- toms. If a patient is to be discharged, he or she should be observed for a minimum of several hours, and maybe longer for individuals with more severe disease or high- risk features. Recurrence of allergic symptoms following resolution has been reported in up to 20% of cases, some as long as 72 hours following initial symptoms.10
If a patient is to be discharged following an anaphylactic reaction, it is mandatory that he or she has a reliable caretaker and 911 telephone access, as well as receive a prescription for epinephrine autoinjectors, including instructions on their use. A good rule of thumb is to prescribe two or three autoinjectors on dis- charge and instruct the patient to always carry one on his person. A short course of H1 blockers, H2 blockers, and steroids is also recommended. While there has not been a fully proven treatment duration, three days is usually sufficient.2
In addition, epinephrine autoinjectors may be indicated in select patients suffering from allergic reactions even if they do not meet criteria for anaphylaxis.4 Certain allergies—such as to peanuts, tree nuts, shellfish, and insect stings—have high potential for causing anaphylactic reactions during future exposures.11 Asth- matic patients who have suffered a generalized allergic reaction and individuals living in remote locations with limited access to emergency medical care should also be prescribed an epinephrine autoinjector.11
Conclusion
Anaphylaxis is a medical emergency that requires rapid and aggressive treatment. It is important to remember that although skin findings are common, they are not necessary for the diagnosis of anaphylaxis. Epinephrine is safe and effective and should be considered the main- stay of treatment. Intramuscular injections are preferred over the subcutaneous route. Antihistamines (both H1 and H2 blockers) and steroids probably do not play a major role in the treatment of acute anaphylactic reactions, but there is little reason not to give them and they will likely help to prevent the recurrence of symptoms. Have a low threshold to admit patients suffering from anaphylaxis for hospital observation, and remember that even with treatment, symptoms may recur. n
REFERENCES
- Neugut AI, Ghatak AT, Miller Anaphylaxis in the United States: an investigation into its epidemiology. Arch Intern Med. 2001;161(1):15–21.
- Davis, Allergy and anaphylaxis: analyzing the spectrum of clinical manifestations. Emerg Med Pract. 2005;7(10):1-24.
- Lieberman P, Kemp S, Oppenheimer S, et The diagnosis and management of ana- phylaxis: an updated practice parameter. J Allergy Clin Immunol. 2005;115(3):S483-S523.
- Sampson H, Muñoz-Furlong A, Campbell R, et Second symposium on the definition and management of anaphylaxis: summary report—second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Ann Emerg Med. 2006;47(4):373-380.
- Maddox TG. Adverse reactions to contrast material: recognition, prevention, and Am Fam Physician. 2002;66(7):1229-1234.
- Andeae DA, Andreae Should antihistamines be used to treat anaphylaxis? BMJ. 2009;339:290-291.
- Roth JV, Shields A dilemma: how does one treat anaphylaxis in the sulfite allergic patient since epinephrine contains sodium metabisulfite? Anesth Analg. 2004;98(5):1499-1500.
- Simons FE, Gu X, Simons Epinephrine absorption in adults: intramuscular vs sub- cutaneous injection. J Allergy Clin Immunol. 2001;108(5):871-873.
- Tang A practical guide to anaphylaxis. Am Fam Physician. 2003;68(7):1325-1332.
- Ellis AK, Day Incidence and characteristics of biphasic anaphylaxis: a prospective evaluation of 103 patients. Ann Allergy Asthma Immunol. 2007;98(1):64-69.
- Australasian Society of Clinical Immunology and ASCIA guidelines for adren- aline autoinjector prescription. Available at: http://www.allergy.org.au/anaphylaxis/ epipen_guidelines.htm. Accessed May 19, 2011.