Physical Examination
On physical examination, the patient’s vital signs are as follows:
• Temperature: 99.2°F (37.3°C)
• Pulse: 114 beats/min
• Respiration: 28 breaths/min
• Blood pressure: 162/94 mm Hg
• Oxygen saturation: 99% on room air
The patient is alert and oriented, is not in acute distress, and is breathing comfortably. Her pelvis is stable on palpation, but she has pain on palpation over her left hip, which has a visible deformity. The overlying skin is intact. Her left leg is shortened and externally rotated. She has no pain at the knee. Her dorsal pedal pulse is 2+, and sensation is grossly intact.
Both lungs are clear to auscultation. She has a regular heart rate and rhythm, without murmur, rub, or gallop. Her abdomen has a normal appearance, with no surgical scars, and it is soft and nontender without rigidity, rebound, or guarding. Her medical history reveals hypertension, for which she takes hydrochlorothiazide. She does not smoke.
Differential Diagnosis
• Hip fracture
• Osteosarcoma
• Pelvic metastases
• Jones fracture
• Maisonneuve fracture
Urgent Care Work-Up
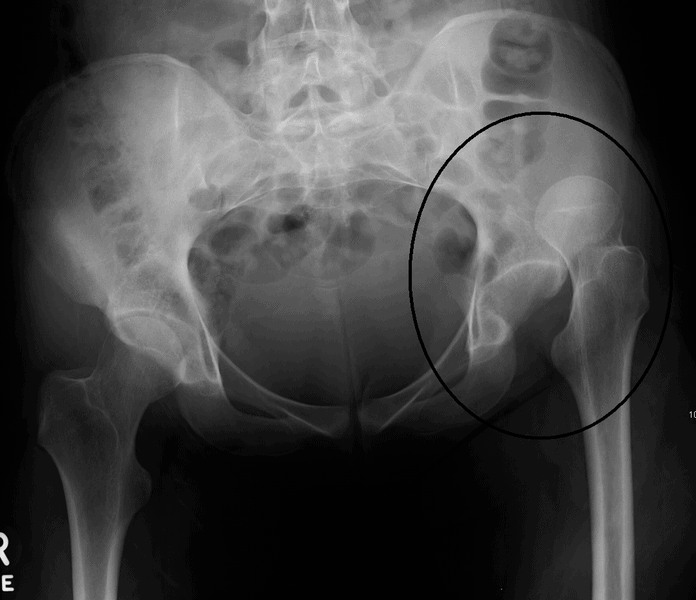
An x-ray (Figure 2) is obtained that shows a dislocated hip.
Diagnosis
The patient’s left hip is dislocated.
Learnings
Hip dislocations may occur primarily, usually as a result of trauma such as a motor vehicle accident, or secondarily in patients who have had a hip replacement. The rate of occurrence in the first year after surgery is 1.9%, with a 7% dislocation rate at 25 years, but the rate is 5% to 8% in patients with Parkinson disease and 6% in patients with stroke. A general classification of a primary hip dislocation is complex (with associated fracture) versus simple (no associated fracture).
A differential diagnosis of hip pain includes many items, but with a hip dislocation, the patient is in significant pain and the dislocation is evident on the x-ray:
• Transient synovitis
• Fracture
• Septic arthritis
• Legg-Calvé-Perthes disease
• Apophyseal avulsion fracture
• Overuse or strain
Ninety percent of hip dislocations are posterior. The mechanism for these is forced adduction and internal rotation, with flexion of the hip. Only 10% of hip dislocations are anterior. The mechanism for these is abduction, external rotation, and either flexion or extension of the hip.
The pelvis is composed of three rings, including the large ring of the pelvis and the two smaller rings of the inferior pubic rami. The femoral neck extends proximally to the femoral head, which inserts deep into the acetabulum of the pelvis, like a ball in a socket. The femoral head is held in the acetabulum by the strong fibrous labrum as well as by the musculature. In hip dislocation, the femoral head slips out of the acetabulum, typically posteriorly.
What to Look For
When obtaining the medical history, ask about the mechanism of injury. In primary hip dislocation, the symptoms typically begin suddenly and are often the result of significant trauma. In secondary dislocation, the mechanism may seem benign, such as crossing the legs or reaching down to tie shoes. Pain in dislocations generally localizes to the hip. There will be extreme pain with attempted movement through the range of motion, both passively and actively, as well as an inability to ambulate. Inquire about paresthesia, pain, and any sensation of warmth or coolness of the extremity.
In performing the physical examination, look for the following issues:
• General condition: Document the patient’s general appearance and position and ability to ambulate.
• Skin changes: Inspect and palpate for erythema, ecchymosis, abrasions, lacerations, fluctuance, necrosis, crepitus, and ecchymosis.
• Location of pain
• Exacerbators of pain: Determine what makes pain worse, such as movement through the full range of motion.
• Shortening of the affected leg
• Swelling over the hip
• Involuntary external rotation of the hip: Watch for this when you flex the patient’s hip.
• Internal rotation of the hip: Patients typically have a limited internal rotation of the hip.
For these patients, obtain x-rays (plain film). A healthy hip has a rounded femoral head extending from the femoral neck that is firmly in the acetabulum. A pelvis x-ray will typically be adequate to demonstrate dislocation. When there is a posterior dislocation, the femoral head appears small and is located superior to the acetabulum, though with a posterior dislocation without superior displacement, the femoral head may appear to rest within the acetabulum; a lateral film will confirm the dislocation. Computed tomography and magnetic resonance imaging are not routinely necessary, but they may be helpful in equivocal cases.
Treatment
Additional trauma should be excluded. With experienced health-care providers and a cooperative patient, reduction (particularly with secondary dislocations of prosthetic hips) may be attempted in the urgent care center. Note, however, that this is a rare situation, and almost all patients will be transferred to an emergency department. Indications for transfer are as follows:
• Concern that there is a hip fracture
• Intractable pain
• Inability to exclude septic arthritis
