Published on
ABSTRACT
Background: The HEART Score is an effective method of risk-stratifying emergency department patients with chest pain. The rate of major adverse cardiovascular events (MACE) in patients with moderate HEART score referred from an urgent care center (UC) for an expedited outpatient cardiology evaluation is unknown.
Purpose: The primary outcome of this study was to examine the rate of MACE when patients with moderate HEART score were referred for expedited outpatient cardiology follow-up after evaluation in urgent care. The secondary outcome was to determine if there is a decrease in rate of ED transfer after this protocol was introduced.
Methods: A cross-sectional study including 133 patients who presented to one of five UCs with chest pain or an anginal equivalent and a HEART score of 4 to 6 (ie, moderate risk) was conducted by a multispecialty group in Las Vegas. A streamlined evaluation protocol to assess each HEART score component was adopted by all UC providers to facilitate an expedited outpatient cardiology follow-up as an alternative to referral to the ED. Data were collected from February 14, 2019 through January 14, 2020. The population was followed for 6 weeks with a primary endpoint of MACE determined by electronic medical record review and direct phone contact with patients. Outcomes were confirmed in 91% of patients. Chest pain transfer data were compared between the final 6 months of 2018 and the final 6 months of 2019.
Results: Over the course of 11 months, 133 patients with a moderate risk HEART score were referred to outpatient cardiology in an expedited manner. The average age was 66 years, with 58% female and 42% male patients; 101 patients (76%) were seen within 3 days; 72 (54%) underwent stress testing; four (3%) had coronary CT angiogram; and four (3%) received an invasive coronary angiogram. Four patients were found to have MACE, including one with non─ST-elevation myocardial infarction (nSTEMI) and subsequent coronary stent, two who were found to have obstructive disease after coronary angiography with subsequent coronary artery bypass graft (CABG), and one who had an abnormal stress test and subsequent CABG. No deaths were identified. The rate of referral to the ED declined by 34%.
Conclusions: Patients with a moderate risk HEART score referred from UC for an expedited outpatient cardiology evaluation had a low rate of MACE/coronary intervention, with no deaths. There was also a significant decrease in the rate of ED referrals.
INTRODUCTION
The advent and validation of the HEART score have improved the disposition of low-risk patients (HEART score 0-3 [HEART being an acronym for history, ECG, age, risk factors, and troponin]) due to a low risk of a major adverse cardiac event (MACE), as defined by revascularization, MI, or death within 4-6 weeks.1,2 In a study of over 2,000 patients in the Netherlands, Backus et al showed a 1.7% risk of MACE in those deemed low-risk,2 though a recent analysis of North American patients has shown a lower rate of 0.8%.3
MACE outcomes for patients in the moderate-risk HEART category (score of 4-6) in the Netherlands were shown to be 17%,2 with a recommendation of admission for further evaluation; however, less is known about the safety of an expedited outpatient evaluation. In 2018, the American College of Emergency Physicians (ACEP) for the first time published a practice guideline for patients seen in the ED with a negative evaluation for chest pain, recommending follow-up within 1-2 weeks, and an acceptable miss rate of a MACE of 1%-2%.4
The rate of MACE in patients with chest pain and a moderate risk HEART score presenting to an Urgent Care (UC) center is unknown. The primary outcome of this study is to examine the rate of MACE after a negative UC evaluation, when this group is referred for an expedited outpatient follow-up within 3 days. The secondary outcome is to determine the change in ED referral rate after the protocol for expedited outpatient follow up was introduced.
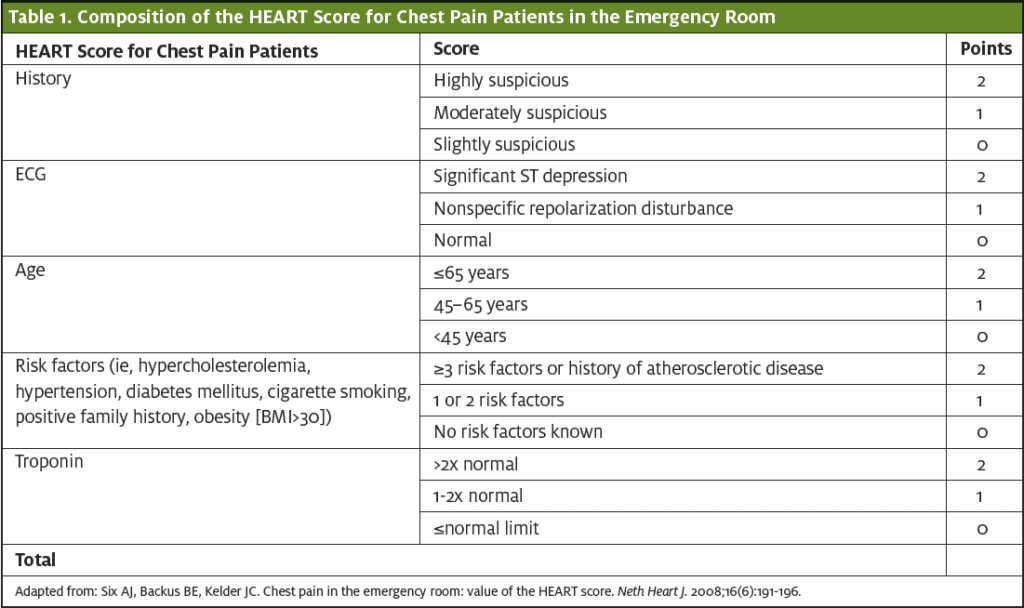
The HEART Score
The HEART score is a risk-stratification tool for assessing the likelihood that a patient with chest pain will experience a clinically important, irreversible cardiac event (ie, myocardial infarction, revascularization, or cardiac death). Each component of the HEART score is assigned a point value between 0 and 2, depending on the extent of the abnormality. A total HEART score between 0 and 3 represents a 2.5% risk for an event, while a score ≥7 carries a 72.7% risk.
METHODS
A cross-sectional study including 133 consecutive patients who presented to one of five Las Vegas urgent care locations with chest pain or an anginal equivalent (eg, jaw or throat pain with exertion) and a HEART score between 4 and 6 between February 14, 2019 and January 14, 2020 was conducted. Patients under the age of 18 or those with positive troponin, paced rhythm, left bundle branch block, significant ST-segment deviation on electrocardiogram, escalating angina, or unstable vital signs were excluded.
Patients were seen by UC providers including physicians, most of whom were board-certified in Family Medicine, and advanced-practice providers (APPs), both physician assistants (PA) and nurse practitioners (NP). In cardiology follow-up, patients were seen by cardiologists (if new patients to the practice) or APPs (if established patients).
UC clinicians followed a predefined protocol with disposition recommendations for patients with an intermediate HEART risk score (4-6) to be scheduled for an expedited cardiology consultation within 3 days of discharge.
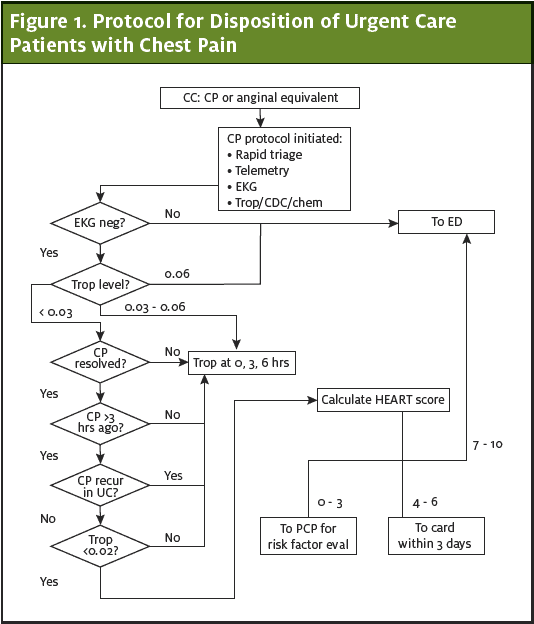
The cardiology department conducted appointments for these patients, scheduled directly by the UC staff. During the cardiology consultation, additional disposition decisions were made, including medical treatment, outpatient stress testing, echocardiography, coronary CT angiography or a conventional coronary angiography.
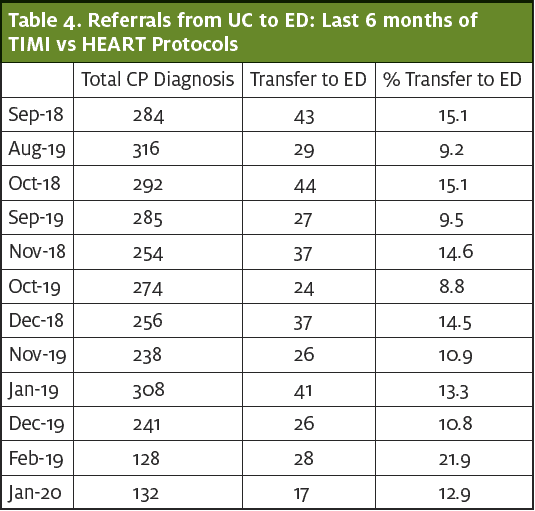
The Thrombolysis in Myocardial Infarction (TIMI) score5 protocol was used for risk stratification of patients presenting to UC with chest pain or angina equivalent, prior to institution of new HEART model in February 2019. Thus, the percentage of ED referral was compared between the times when each protocol was used.
RESULTS
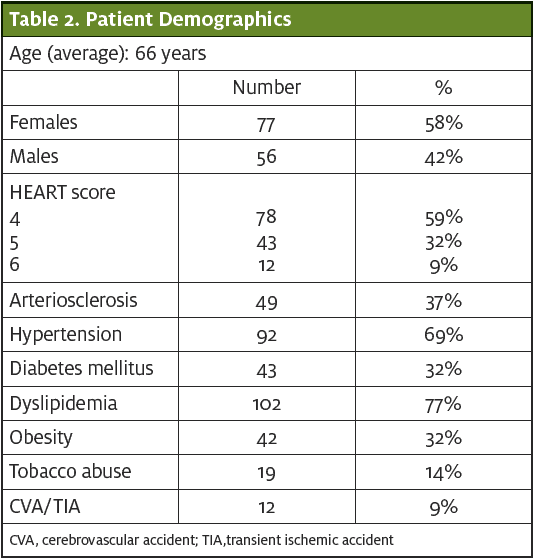
Data were collected from February 14, 2019 through January 14, 2020. The average age was 66; 77 subjects were female (58%) and 56 were male (42%). (See Table 2.) The population was followed with a primary endpoint of MACE at 6 weeks, determined by electronic medical record review and direct phone contact with patients.
OUTCOMES
Over the course of 11 months, 133 patients with a negative UC evaluation and a moderate-risk HEART score were referred for an expedited cardiology follow-up. Of the 133 patients referred for outpatient evaluation, 114 showed up for the appointment; of these 101 (76%) were seen within 3 days. Of these patients, 72 (54%) underwent stress testing, four (3%) had coronary CT angiogram, and four (3%) received an invasive coronary angiogram.
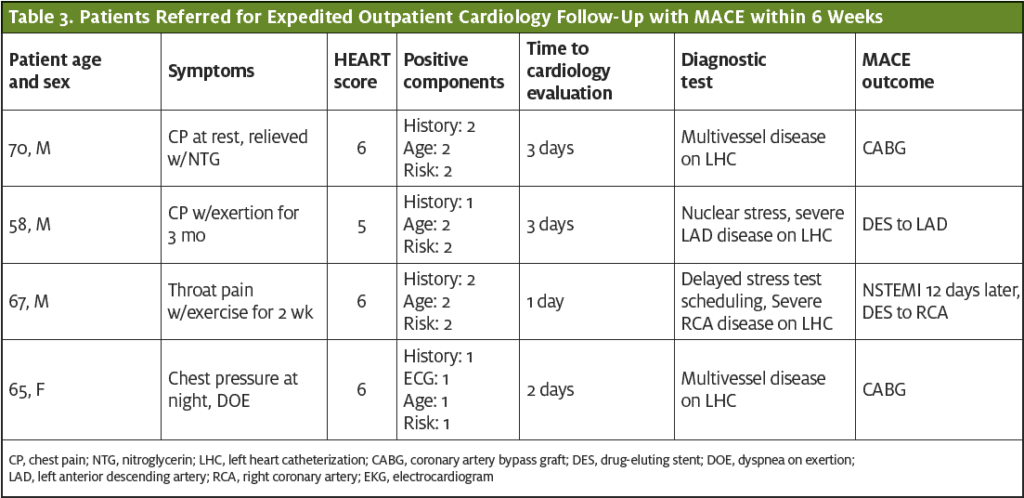
Four patients were found to have a MACE. One patient had a non-ST elevation myocardial infarction (nSTEMI) and subsequent coronary stent, two patients were found obstructive disease after coronary angiography with subsequent coronary artery bypass graft (CABG), and one patient had an abnormal stress test and subsequent CABG. No deaths were identified.
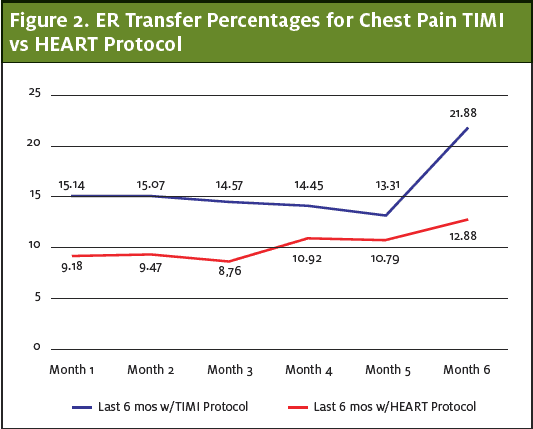
The secondary outcome was to determine if this protocol decreased referrals to the ED. Institution of the outpatient protocol during the 12 months after initiation decreased the rate of ED referral rate by 34%.
The number of UC presentations for chest pain between September 14, 2018 and February 13, 2019 was 1,522 with 230 transfers to the ED (15.1%). After introduction of the protocol (on February 14, 2019), UC visits for chest pain and referrals were reassessed: from August 14, 2019 to January 13, 2020 there were 1,486 presentations for chest pain with 149 transfers (10%), representing a 34 reduction in referrals to the ED ( Z statistic is 4.2169, p<0.00001, 95% confidence interval that the difference between the two means is between 2.73% and 7.47%.) (See Table 4.)
DISCUSSION
Though clinicians still have considerable concern for MACE when discharging patients from the ED with chest pain,6 the practice of referring patients with a low-risk HEART score for outpatient evaluation has become more widely accepted. Less is known about the risk of patients with a moderate-risk HEART score and the safety of referring them from UC for an expedited outpatient cardiology evaluation.
After introduction of a protocol to evaluate UC patients with chest pain as outpatients over a span of 12 months, only four of 133 Patients had a MACE. One had a positive stress test and received a stent to the LAD, and two were referred for a cardiac catheterization resulting in coronary artery bypass grafts (CABGs). One patient returned and was found to have an nSTEMI, but this patient had an outpatient referral which deviated from the instituted protocol (the patient did not have a stress test scheduled as ordered by a cardiologist within 3 days due to scheduling problems).
Institution of the protocol resulted in a decrease of 34% in patients referred from the UC to the ED, with subsequent potential implications including reduced cost, decreased resource utilization, less patient inconvenience, and less potential for over-testing and false positive results.
The risk of MACE in patients after a negative evaluation is low, with one of the primary considerations being missed MI. Hess, et al demonstrated a low rate of adverse outcomes in patients with nSTEMI with a rate of sudden cardiac death of 0.79% in the 6 months following diagnosis.7,8 Even in the ED setting, there is an exceedingly low risk of clinically relevant cardiac events, including STEMI, life-threatening arrhythmia, cardiac arrest and death.9
After a negative evaluation for chest pain, patients are better able to understand their individual risk and to make decisions using a shared decision-making model.7,8
Of the 133 patients referred for expedited outpatient evaluation, 19 (14%) cancelled or did not show up for their cardiology appointments and 101 (76%) were seen within a 3-day window. We attempted to contact all 133 patients by phone. Twelve patients (9%) could not be reached by phone, but lack of MACE was confirmed by chart review.
To our knowledge, this is the first study to evaluate MACE outcomes and decreased ED referrals in UC patients after the institution of a protocol for expedited outpatient referral to cardiology. These are the initial results in 133 patients over an 11-month period of time. Future work will focus on validating these results by applying and studying the protocol in a larger group of UC patients with chest pain.
LIMITATIONS
Limitations include missed MACE outcomes with the 9% of patients who were not able to be contacted. We did not evaluate for adverse cardiac events after the cardiology visit, such as complications from a cardiac catheterization or a procedure. Past studies have shown that there is some clinician variation in calculation of the HEART score10,11; this study did not standardize the calcuation and we did not examine for physician variation. Some patients who did not follow up may have had an unrecognized MACE such as a silent MI. Finally, the UCs in this study did have the ability to get troponin testing, and this may limit the generalizability to most UCs where troponin testing is not generally available while the patient is still present.
CONCLUSIONS
Patients with a moderate-risk HEART score referred from UC for an expedited outpatient cardiology evaluation had a very low rate of MACE outcomes and no deaths. The referral rate to the ED decreased by 34% during the study period. Expedited outpatient cardiology referral for UC patients with chest pain and moderate risk HEART score appears to be a reasonable approach for this patient population.
Citation: Barbarash S, Lebron-Gallegher, D, Julson, Weinstock, M. A multicenter study of the rate of MACE in chest pain patients with a moderate HEART risk score referred from urgent care for an expedited outpatient cardiology evaluation. J Urgent Care Med. September 2020. Available at:
REFERENCES
- Backus BE, Six AJ, Kelder JC, et al. Chest pain in the emergency room: a multicenter validation of the HEART score. Crit Pathways in Cardiol. 2010;9:164–169)
- Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients in the emergency department. Int J Cardiol. 2013;168(3):2153-2158.
- Laureano-Phillips J, Robinson RD, Aryal S, et al. HEART score risk stratification of low-risk chest pain patients in the emergency department: a systematic review and meta-analysis. Ann Emerg Med. 2019;74(2):187-203.
- Tomaszewski CA, et al. Clinical policy: critical issues in the evaluation and management of emergency department patients with suspected non-ST-elevation acute coronary syndromes. American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Suspected Non–ST-Elevation Acute Coronary Syndromes. Ann Emerg Med. 2018;72(5):e65-e106.
- Antman EM, Cohen M, Bernink PJ, et al. The IMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000; 284(7):835-8
- Than M, Herbert M, Flaws D, et al. What is an acceptable risk of major adverse cardiac event in chest pain patients soon after discharge from the emergency department? A clinical survey. Int J Cardiol. 2013;166(3):752-754.
- Hess EP, Knoedler MA, Shah ND, et al. The chest pain choice decision aid: a randomized trial. Circ Cardiovasc Qual Outcomes. 2012;5(3):251–259.
- Hess EP, Hollander JE, Schaffer JT, et al. Shared decision making in patients with low-risk chest pain: prospective randomized pragmatic trial. BMJ. 2016;355:i6165.
- Weinstock MB, Weingart S, Orth F, et al. Risk for clinically relevant adverse cardiac events in patients with chest pain at hospital admission. JAMA Intern Med. 2015;175(7):1207-1212.
- Dubin J, Kiechle E, Wilson M, et al. Mean HEART scores for hospitalized chest pain patients are higher in more experienced providers. Am J Emerg Med. 2017;35(1):122–125
- Wu WK, Yiadom MY, Collins SP, et al. Documentation of HEART score discordance between emergency physician and cardiologist evaluations of ED patients with chest pain. Am J Emerg Med. 2017;35(1):132–135.
This study was conducted as a retrospective chart review. Patient identifiers were used only for the purposes of tracking outcomes and measures were taken to ensure no breaches of PHI occurred. The data were initially planned and collected as part of an internal safety and quality monitoring project and care was not changed based on this study. IRB approval was not sought out prospectively for these reasons and the work did conform to usual ethical standards around protecting patient privacy. No funding was obtained for this study.
The authors would like to thank:
Allen Frye, NP – Research coordinator, Adena Health Systems
Robert Korkow, MBA – Senior Data Engineer, Healthcare Economics department, Southwest Medical, part of OptumCare
John Foreman, PE – Business Operations Director, Specialties, Southwest Medical, part of OptumCare
Julia Somerville-Reeser, RN, BSN, RN-BC – Cardiology Manager, Southwest Medical, part of OptumCare
Author affiliations: Svetlana Barbarash, MD, FACC, Department of Cardiology, Southwest Medical, part of OptumCare, Las Vegas, NV. Dolores Lebron-Gallagher, MS PA-C, Department of Cardiology, Southwest Medical, part of OptumCare, Las Vegas, NV. Hollis Julson, MD, Department of On Demand Medicine, Southwest Medical, part of OptumCare, Las Vegas, NV.
Michael B. Weinstock, MD, Department of Emergency Medicine, Adena Health Systems, Chillicothe, OH. The authors have no relevant financial relationships with any commercial interests.
This study received Internal Review Board (IRB) approval from the UnitedHealth Group Office of Human Research Affairs.

