Urgent message: The urinalysis is a ubiquitous test in urgent care settings, though there is nuance and complexity in its interpretation. An evidence-based approach is essential to assuring correct interpretation and decision-making.
Douglas W. Wallace, MD, Blakeley Hudson, MD, and Matthew Delaney, MD
Introduction
The urinalysis (UA) is one of the most commonly ordered tests across a variety of practice settings. Despite its ubiquity, interpreting a UA can be complicated and nuanced. Given the variable treatment and disposition decisions that we make based on its results, it is crucial to employ an evidence-based approach to UA interpretation.
What Are the Components of a Urinalysis?
A urine sample can be evaluated both qualitatively (gross appearance and dipstick urinalysis) and quantitatively (microscopic urinalysis). Additional studies on the urine include urine culture, urine PCR, and various urinary antigen studies. Our focus here will be on interpretation of the urine dipstick, urine microscopy, urine culture, and subsequent decision making.
Where to Begin?
The first step is to obtain an adequate sample, with minimal contamination. This is ideally achieved with a clean catch, midstream sample from the first urine of the day. The reality of sample collection is never this ideal, but here are some tips to improve the quality of a urine sample.
- Locally disinfect the urethral meatus with a sterile swab
- Retract the labia in women or the foreskin in men
- Collect a sample midstream
Of these listed measures, obtaining a midstream sample has been shown to be the most helpful in reducing contamination. Cleaning of the meatus and retraction of adjacent structures are important but less helpful overall.1
How Do I Approach Interpretation of a Dipstick Urinalysis?
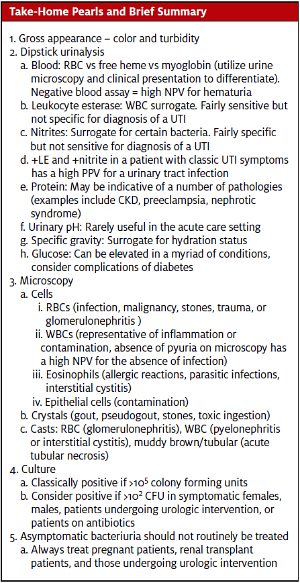
Blood
The urine dipstick test represents information obtained from a qualitative chemical reaction performed on the urine sample. Blood is the first dipstick assay. It nonspecifically detects red blood cells, free heme, and myoglobin molecules. Positive blood on a dipstick can thus represent hematuria, hemolysis, or myoglobinuria. These etiologies can be differentiated by noting the actual number of RBCs per high power field on microscopic urinalysis.
In the setting of rhabdomyolysis, you might see a positive dipstick test for RBCs (3 + blood), but a subsequent microscopic analysis of the sample will reveal few or no RBCs as myoglobin in the urine causes a false positive for the Blood assay. If your facility lacks the capability for quantitative urine microscopy, the clinical presentation of a patient with 3+ blood becomes vital in your decision making. A patient who complains of aching muscles and dark urine after vigorous exercise may have rhabdomyolysis, whereas a patient with a past medical history of nephrolithiasis presenting with a familiar onset of unilateral flank pain and emesis may have acute ureterolithiasis. The discernment will fall to your history and physical and clinical gestalt. Once hematuria is confirmed, the next step is to consider its origin. Blood in the urine can be caused by many pathologies, including a urinary tract infection (UTI), malignancy, urolithiasis, traumatic injury, or an underlying inflammatory process such as glomerulonephritis. Despite it being nonspecific, the blood assay does have a high negative predictive value, and if negative, essentially rules out significant hematuria.2
Infection
Leukocyte esterase (LE) measures white blood cell byproducts and is a surrogate marker for the presence of white blood cells (WBCs). Leukocyte esterase is fairly sensitive for the presence of a UTI but not highly specific. WBCs in the urine can be reflective of any inflammatory process in the urinary tract or even represent contamination from the adjacent genitalia in a female patient.
Nitrite is an indicator of nitrite reductase, an enzyme present in organisms of the genus Enterobacteriaceae (E coli, Proteus, Salmonella, Shigella, and Yersinia); many of which are frequent uropathogens. Positive nitrites are in turn fairly specific for bacteriuria but not very sensitive, as there are also a number of bacteria that do not produce nitrites (notably enterococcal and staphylococcal species).
The LE and nitrite assays are perhaps best used in conjunction. A meta-analysis by Devillé, et al found that the combination of positive LE and nitrites on dipstick urinalysis improved diagnostic accuracy compared with symptoms alone, having a high positive predictive value for urinary tract infection in females older than 14 years with classic symptoms.3 Three symptoms (dysuria, urgency, and nocturia) were also shown to have a positive likelihood ratio (LR) for UTI significantly greater than 1.0 (1.1, 1.2, and 1.3, respectively).4 If a dipstick analysis in clinical practice is positive for both nitrites and LE in the setting of a patient with classic symptoms (dysuria, nocturia, urgency), it is reasonable to assume the patient has a UTI while sending a urine culture as indicated. The most common bacteria causing uncomplicated cystitis and pyelonephritis are E coli (75%-95%), P mirabilis, K pneumoniae, and S saprophyticus.5 Urgent care providers should familiarize themselves with relevant treatment guidelines, as well as local antibiotic resistance data.
Protein is present in a variety of pathologies, including CKD, nephrotic syndrome, preeclampsia, and ESRD in diabetic patients.6 Patients with persistent proteinuria should be further evaluated with a 24-hour urine protein and continued outpatient follow-up. If ongoing proteinuria is present, nephrology referral should be strongly considered.
Other relevant aspects of the dipstick urinalysis include pH, specific gravity, and glucose. Urinary pH can be abnormal in a variety of clinical presentations, notably metabolic acidosis and toxic ingestions. Any patient with severe acid base derangements on a basic metabolic panel and a substantially abnormal urinary pH should be referred for further evaluation. Otherwise, urinary pH is rarely useful in the acute care setting. Specific gravity measures osmolality of urine and can be used as a surrogate marker of a patient’s hydration status. A low or normal specific gravity is reassuring that significant dehydration is less likely in an otherwise well appearing patient. Glucose in the urine can be a marker of new-onset or uncontrolled diabetes along with a host of other illnesses, suspected by symptoms of polyuria, polydipsia, polyphagia, and weight loss. Persistent glycosuria should prompt further testing and consideration of referral for evaluation for diabetes and subsequent management as indicated.
What About Microscopic Urinalysis?
Though not widely available or in common use in many urgent care settings, urine quantitative microscopy provides additional data about a urine sample, much of which can be clinically useful. The first value mentioned on a microscopic urinalysis report is the gross assessment of the urine with the consistency and color being noted. A consistency of “turbid,” for example, might be indicative of crystals or inflammation in the urine. Changes in color may indicate the presence of blood (red or dark), drugs (orange for azo or rifampin, green for methylene blue), or ingested foods (beets or rhubarb). Urine sediment analysis is also routinely reported on microscopy and is an assessment that cannot be obtained from dipstick testing. There are three primary components of the sediment: cells, casts, and crystals. There are four cell lines that are important: RBCs, WBCs, eosinophils, and epithelial cells (most often squamous cells).
As mentioned previously, dipstick urinalysis can nonspecifically detect the presence of RBCs, free heme, or myoglobin in the urine. Microscopy can then be utilized to confirm the presence of true hematuria, again seen in five principal pathologies: infection, malignancy, stones, trauma, or glomerulonephritis. Gross hematuria should be evaluated further to discern an etiology; patients with persistent hematuria need referral for urological consultation. This can frequently be done as an outpatient if the patient is clinically stable and well appearing.
Pyuria, defined by WBCs >10 per high power field, can be indicative of infection or inflammation. Similar to leukocyte esterase, lack of pyuria has a high negative predictive value for the presence of infection.7
Eosinophils in the urine should prompt consideration for interstitial cystitis but can also be present in parasitic infections and allergic reactions.
Epithelial cells in the urine, particularly squamous cells, are an important sign of contamination and the need for a novel specimen. The authors’ opinion is that if the pretest probability for urinary tract infection is very high (classic symptoms of UTI in a young healthy female patient), the presence of epithelial cells should not dissuade a provider from pursuing appropriate UTI treatment if a novel specimen is not readily able to be obtained.
Casts and crystals
Casts are cylindrical structures that are formed in the renal tubules and assume the shape of the lumen in which they are formed. They are described based on their appearance. Some examples are RBC casts indicating glomerulonephritis, WBC casts indicating renal inflammation as in pyelonephritis, and muddy brown or tubular casts indicating acute tubular necrosis and renal cell death. Crystals can be present in several disease processes. Uric acid crystals may indicate gout or tumor lysis syndrome, calcium pyrophosphate crystals may indicate pseudogout, and calcium oxalate crystals may indicate stones or ethylene glycol ingestion as notable examples.
Not all clinics have the ability to do urine microscopy testing. Fortunately, although urine microscopy can provide a lot of clinically useful information, the available evidence suggests microscopy adds little relevant data compared to the dipstick results when assessing specifically for UTI. In a systematic review Beyer et al found that adding urine microscopy to urine dipstick only slightly improved the sensitivity for detecting an underlying UTI.8 The authors noted that the sensitivity of dipstick and microscopy combined fell below the gold standard of a urine culture.9 Prior studies noted that microscopic detection of moderate bacteria and WBCs in urine microscopy had sensitivities less than 75% and 80%, respectively.10 The positive predictive value (PPV) of microscopic examinations of pyuria, bacteriuria, or both have been shown to be as low as 33%.11 A positive dipstick urinalysis without additional urine microscopy in the setting of classic symptoms of a urinary tract infection is likely sufficient to diagnose a UTI with an additional urine culture as indicated.
When Should I Send a Urine Culture?
Urine culture is considered the gold standard for diagnosis of a urinary tract infection, yet there is significant practice variation in terms of providers’ ordering patterns. National and international guidelines recommend urine culture in all patients clinically suspected of having a UTI with the exception of patients with uncomplicated cystitis. Uncomplicated cystitis is classically defined as a healthy, young, non-pregnant female with typical symptoms of a urinary tract infection and no risk factors for drug resistance. In turn, urine cultures should be performed in all of the following clinical scenarios.12
- Suspected acute pyelonephritis
- Symptoms that do not resolve or recur within four weeks after the completion of treatment
- Women who present with atypical symptoms
- Elderly patients in whom you have suspicion for UTI without classic symptoms
- Complicated urinary tract infection (male patients, pregnant patients, vesicoureteral reflux patients, patients with recent instrumentation, diabetic patients, immunocompromised patients, patients with a history of resistant or nosocomial infections, patients with urinary obstruction)
A urine culture is classically considered positive when the culture is greater than 100,000 colony-forming units per mL if an adequate sample that limited contamination was obtained. There are a number of notable exceptions to this rule including: male patients, women with classic symptoms of a urinary tract infection, patients already on antibiotics, and patients undergoing urologic intervention. In these patients, greater than 100 colony-forming units per mL are sufficient to diagnose a urinary tract infection.13
There are limitations to the sensitivity of urine culture in specific patient populations despite it being the current gold standard. Though not available in any routine clinical practice, approximately 90% of symptomatic women will be found to have a true urinary tract infection if multiplex PCR is utilized to detect urinary pathogens despite a negative urine culture, suggesting that most women with classic symptoms can reasonably be treated empirically for urinary tract infection.14
Asymptomatic Bacteriuria: to Treat or not to Treat?
In general, asymptomatic bacteriuria should not be routinely treated, even in patients with a history of immunosuppression, diabetes, spinal cord injuries, indwelling catheter placement, advanced age, or those undergoing orthopedic procedures.12,13 A number of trials have demonstrated that treatment of asymptomatic bacteriuria has no statistically significant effect on the incidence of symptomatic UTI, complications of UTI, or death compared with no treatment or placebo in all of these patient populations.7 The available evidence and national and international guidelines do support treating asymptomatic bacteriuria in pregnant patients, patients undergoing urologic intervention, and renal transplant recipients.12,13 Despite these recommendations, frequent over treatment of asymptomatic bacteriuria is occurring in a variety of settings and can be harmful. Overtreatment can lead to a number of complications including unnecessary adverse drug effects, allergic reactions, and antibiotic resistance.
Citation: Wallace DW, Hudson B, Delaney M. Urinalysis: A simple test with complicated interpretation. J Urgent Care Med. July 2020. Available at: https://www.jucm.com/urinalysis-a-simple-test-with-complicated-interpretation/
References
- Rabinovitch A, Arzoumanian L, Curcio KM, et al. Urinalysis-Approved Guideline. 3rd ed. Wayne, PA: Clinical and Laboratory Standard Institute. 2009;29(4). http://www.clsi.org/source/orders/free/gp16-a3.pdf (Accessed on March 31, 2020).
- Daum GS, Krolikowski FJ, Reuter KL, et al. Dipstick evaluation of hematuria in abdominal trauma. Am J Clin Pathol. 1988 Apr;89(4):538-42.
- Devillé WL, Yzermans JC, van Duijn NP, et al. The urine dipstick test useful to rule out infections. A meta-analysis of the accuracy. BMC Urol. 2004 Jun 2;4:4.
- Simati B, Kriegsman B, Safranek S. FPIN’s clinical inquiries. Dipstick urinalysis for the diagnosis of acute UTI. Am Fam Physician. 2013;15;87(10).
- Carroll MF, Temte JL. Proteinuria in adults: a diagnostic approach. Am Fam Physician. 2000;62(6):1333-1340.
- Cortes-Penfield NW, Trautner BW, Jump RLP. Urinary Tract Infection and Asymptomatic Bacteriuria in Older Adults. Infect Dis Clin North Am. 2017;31(4):673-688.
- Beyer AK, Currea GCC, Holm A. Validity of microscopy for diagnosing urinary tract infection in general practice – a systematic review. Scand J Prim Health Care. 2019;37(3):373-379.
- Córdoba G, Holm A, Sørensen TM, et al. Use of diagnostic tests and the appropriateness of the treatment decision in patients with suspected urinary tract infection in primary care in Denmark – observational study. BMC Fam Pract. 2018;19(1):65.
- Bailey BL. Urinalysis predictive of urine culture results. J Fam Pract. 1995;40:45-50.
- Lohr JA, Portilla MG, Geuder TG, et al. Making a presumptive diagnosis of urinary tract infection by using a urinalysis performed in an on-site laboratory. J Pediatr. 1993;122:22-25.
- Bonkat G, Bartoletti RR, Bruyère F, et al. European Association of Urology Practice Guidelines: Urologic Infections. Available at: https://uroweb.org/guideline/urological-infections/. Accessed March 1, 2020.
- Nicolle LE, Gupta K, Bradley SF, et al. Clinical Practice Guideline for the Management of Asymptomatic Bacteriuria: 2019 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2019;68(10):e83‐e110.
- Heytens S, De Sutter A, Coorevits L, et al. Women with symptoms of a urinary tract infection but a negative urine culture: PCR-based quantification of Escherichia coli suggests infection in most cases. Clin Microbiol Infect. 2017;23(9):647–652.
- Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103‐e120.
Douglas W. Wallace, MD is Assistant Professor, Department of Emergency Medicine, University of Alabama at Birmingham. Blakeley K. Hudson, MD is Resident Physician, Department of Emergency Medicine, University of Alabama at Birmingham. Matthew Delaney, MD is Associate Professor and Assistant Residency Director, Department of Emergency Medicine, University of Alabama at Birmingham. The authors have no relevant financial relationships with any commercial interests.
