Urgent message: Urgent care is often the first stop for patients experiencing acute eye complaints, including conjunctivitis. The capability to accurately distinguish between infectious conjunctivitis of a viral nature vs that of a bacterial nature is essential to administering appropriate treatment and avoiding inappropriate use of antibiotics.
Isabelle Dortonne, MD, Patrizia Colmenares, OD, Trevor Lyford, BA, OSC, and John Sheppard, MD, MMSc
INTRODUCTION
The vast majority of acute conjunctivitis is viral in nature, with 65% to 90% due to adenoviruses.1 Despite this, a study by University of Michigan’s Kellogg Eye Center found that 58% of patients with a pink eye diagnosis filled a prescription for antibiotics.2 Further, a surprisingly large number of prescriptions for conjunctivitis are antibiotic–corticosteroid combinations. Primary care and urgent care providers are at the front lines of conjunctivitis diagnosis, evaluating up to 83% of patients initially presenting to a non-eyecare provider.2 Eye complaints make up approximately 3% of all urgent care visits.3 It is important to differentiate between conjunctivitis of bacterial versus viral vs other etiology in order to manage these conditions correctly and reduce the overuse of antibiotics.
HISTORY AND PHYSICAL EXAM
Differentiating between bacterial and viral conjunctivitis can be difficult because most of the signs and symptoms tend to be largely non-specific and may overlap.
Key questions to consider:
- When did symptoms begin?
- In most cases, acute forms of viral and bacterial conjunctivitis tend to be self-limiting and will resolve on their own in 7-14 days. Cases lasting longer should seek evaluation by an ophthalmologist.
- Has the patient had an upper respiratory infection (URI) recently?
- A recent URI and palpable preauricular or sub-mandibular lymph nodes are suggestive of viral etiology.
- Contact with any other at-risk groups or infected friends/co-workers/family members?
- Viral conjunctivitis is extremely contagious with a transmission rate between 10-50%.4 It can be transmitted via fomites contaminated with ocular secretions or via respiratory secretions.
- One study found that adenovirus spread to 50% of family members or those in close contact with the infected individual.4
- Bacterial conjunctivitis can be spread through direct contact with ocular secretions or contaminated fomites.
- Recent infection in the other eye?
- Infected individuals can shed the virus for up to 14 days after the onset of symptoms, with the virus able to survive on innate surfaces for days.
- Co-infection of the other eye during the 14-day shedding period is common.
- Type of discharge?
- Watery discharge tends to be associated with viral or allergic conjunctivitis, and purulent discharge with bacterial conjunctivitis.
- Does the eye itch?
- Itching is a common symptom in allergic conjunctivitis, although pruritis can be present to a lesser degree in viral conjunctivitis.
- Does the patient wear contact lenses?
- Does the patient sleep in contact lenses or wear contacts for greater than 8 hours a day?
- When was the patient’s most recent contact lens fitting?
- Contact lens abuse and overuse can lead to secondary causes of red eyes not associated with infection, or to sight-threatening infectious keratitis.
Red Flag Symptoms
If the patient presents with severe pain, light sensitivity, or reduced vision consider referral to ophthalmology. These symptoms could be signs of uveitis, high intraocular pressure, corneal ulcer or herpetic corneal disease. Patients with uveitis require management by an eye care provider with topical steroids and diligent diagnostic testing.
Those with a corneal ulcer (keratitis) will need topical/oral antibiotics, oral antivirals, or topical/oral antifungals, depending on etiology. When in doubt, or vision is significantly reduced, an ophthalmology referral should immediately be considered.
Narrowing the list of red eye differentials solely on presentation without the use of diagnostics is a daunting task. The above descriptions are examples of classic presentations, but we all know that real-world presentations are not always as clear cut.
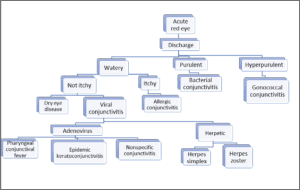
Differential Diagnosis of Conjunctivitis Presenting with Discharge
Bacterial Conjunctivitis
Bacterial conjunctivitis classically presents as a red, irritated eye with a purulent white-yellow or green discharge, foreign body sensation, conjunctival papillae and chemosis. One week of topical antibiotics is generally indicated. Hyperacute conjunctivitis with excessive purulent yellow- green discharge accompanied by marginal keratitis, conjunctival papillae and preauricular adenopathy is suggestive of gonococcal conjunctivitis.1 Treatment entails aggressive topical antibiotics (eg, bacitracin or gentamicin), irrigation to prevent accumulation of purulent material potentially damaging to the cornea, as well as appropriate systemic treatment (ceftriaxone and coverage for chlamydia with azithromycin or doxycycline).
| Pathogens | Presentation | |
| Bacterial Conjunctivitis | Staphylococcus aureus, (most common), Staphylococcus epidermidis, Streptococcus pneumoniae and Haemophilus influenzae | Red eye, purulent or mucopurulent discharge with mattering and adherence of lids, chemosis5,10 |
| Gonococcal Conjunctivitis | Neisseria gonorrhoeae | Hyperacute conjunctivitis with excessive yellow-green purulent discharge, conjunctival injection, chemosis, lid swelling, tender preauricular lymphadenopathy accompanied by genitourinary disease6,10 |
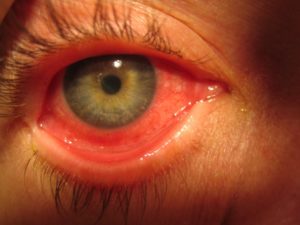
Adenoviral conjunctivitis with diffuse bulbar and inferior tarsal conjunctival injection, serious discharge, irregular corneal reflex and corneal epitheliopathy, ipsilateral pre-auricular lymphadenopathy, and pharyngitis. (Photo courtesy of Robert Sambursky, MD.)
VIRAL CONJUNCTIVITIS
- Herpetic Infection
Viral conjunctivitis due to a herpetic infection can present very similarly to adenoviral conjunctivitis. Herpes simplex infection presents with a red, irritated eye, follicular conjunctivitis and possibly corneal dendrites. Herpes zoster ophthalmicus will usually present with a vesicular rash that respects trigeminal dermatome. Patients with a rash that extends to the tip of their nose in the nasociliary branch distribution of the ophthalmic portion (V1) of the trigeminal nerve, known as Hutchinson’s sign, are more likely to have ocular involvement. The treatment for herpetic infections involves topical and/or oral antiviral medication. It is important to note that in cases of herpetic conjunctivitis/keratitis, steroid use will prolong the infection and will cause an increase in viral load leading to greater complication risks.
| Viral Conjunctivitis: Herpetic | Presentation |
| Herpes Zoster | Acute vesicular dermatomal skin rash along the first division of the 5th cranial nerve, injection, with or without corneal involvement1,10 |
| Herpes Simplex | Conjunctival injection with acute unilateral follicular conjunctivitis, with or without corneal dendrites or geographic ulceration1,10 |
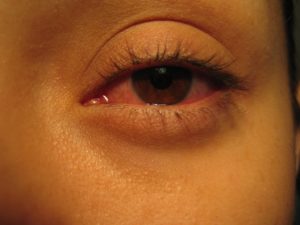
Blepharitis with pseudoptosis, intense bulbar conjunctival injection, serous discharge, pruritic caruncular inflammation, and epiphora due to canalicular edema resulting from adenoviral infection. (Photo courtesy of Robert Sambursky, MD.)
2. Adenovirus
Viral conjunctivitis due to adenovirus can be broken down into three main categories: pharyngeal conjunctival fever, epidemic keratoconjunctivitis (EKC) and nonspecific conjunctivitis. Adenoviral conjunctivitis classically presents as an acute red eye with watery discharge and lymphadenopathy. Pharyngeal conjunctival fever presents with similar findings as well as pharyngitis and fever. EKC can present as the most severe of the three forms, with classic signs as well as pseudomembranes, subepithelial infiltrates from keratogenic serotypes, and conjunctival hemorrhage.
Epidemic keratoconjunctivitis (EKC), caused most commonly by adenoviral serotypes 8, 19, and 37, is the only adenoviral syndrome associated with corneal inflammation. Keratitis in EKC characteristically presents with multiple corneal infiltrates in the subepithelial stroma beginning 1 to 2 weeks after onset of the conjunctivitis. The corneal infiltrates of EKC cause significant ocular morbidity; reduced vision, photophobia, and foreign body sensation may persist for months to years after infection. 5
There is no gold standard of treatment for adenoviral conjunctivitis due to its self-limiting nature. Treatment is supportive with artificial tears, cool compresses, and as needed antihistamine drops. Antibiotics are not effective in treating adenovirus and should only be used when a bacterial co-infection is suspected. Systemic antivirals are not effective for adenoviral conjunctivitis. There are current ongoing clinical trials regarding the use of povidine iodine and topical ganciclovir in treatment.7 In severe cases of EKC, pseudomembranes should be removed with forceps or a cotton swab and careful topical corticosteroids should be applied to prevent scarring.1 Referral to an ophthalmologist to manage the corticosteroids is warranted. Patients are considered contagious while the eye is still injected and tearing. During this time period, strict hand hygiene precautions should be employed, and the patient should stay home from work and school while contagious.
| Viral Conjunctivitis: Adenovirus | Serotype | Presentation |
Pharyngeal Conjunctival Fever
| 3, 7 Less commonly: 2, 4, 14 | Bilateral conjunctivitis, high fever, pharyngitis, preauricular lymph node enlargement5,10 |
Epidemic Keratoconjunctivitis
| 8,19,37 | Unilateral watery discharge, hyperemia, chemosis, ipsilateral lymphadenopathy with subepithelial infiltrates appearing on the cornea 4-7 days after initial symptoms5,10 |
| Nonspecific Conjunctivitis | 1-11, 13, 15, 17, 19, 20-30, 32, 33, 36-39, 42-49 | Unilateral, watery discharge, follicles on palpebral conjunctiva, preauricular lymph node enlargement6,10 |
DIAGNOSTICS
When assessing a patient with acute conjunctivitis, it is important to keep in mind that adenovirus makes up the majority of cases of viral conjunctivitis. Currently, most diagnoses of adenoviral conjunctivitis are made clinically. It is estimated that clinical diagnoses have only 40%–72% accuracy when compared to traditional laboratory diagnostics. Viral cell culture with immunofluorescence assay and PCR are cumbersome, expensive, and time consuming.7
Rapid diagnostic tests and culture are among the most common procedures in urgent care centers, done at 49.2% of patient visits with a total of 87.1 million performed in 2018.3 As such, advancement in rapid testing for conjunctivitis, especially concerning adenovirus, could be expected to have ready application in the urgent care setting. The most recent such test, QuickVue Adenoviral Conjunctivitis Test (Quidel), formerly RPS AdenoPlus, is a second generation test built upon the RPOS Adeno Detector, with enhanced sensitivity and specificity. Administration is simple, and can be performed easily by ancillary staff with results within 10 minutes. It utilizes an immunoassay test strip, which comes into direct contact with the sample antigen. It recognizes viral hexon antigen from all 55 subtypes of adenovirus. A recent prospective study of 128 patients with clinical diagnosis of acute viral conjunctivitis has demonstrated high sensitivity (85%-90%) and specificity (96%-98%) when compared to current standard diagnostic methods of cell culture and PCR.7
Implications of Novel Diagnostic Testing
Morbidity from adenoviral conjunctivitis can span from weeks to years, with discomfort and decreased vision from varying levels of inflammation. In severe conditions, especially in which diagnosis and thus initiation of corticosteroids are delayed, a patient can develop permanent dry eyes and scarring of the conjunctiva and cornea. Nearly 20% of scripts filled for conjunctivitis are an antibiotic-corticosteroid combination. However, unless warranted due to signs of inflammatory infiltrates or membranes such as in EKC, corticosteroids are contraindicated in viral conjunctivitis because they can lengthen the course of the disease and may reactivate latent herpes simplex virus.2
Routine use of effective rapid tests may have the potential to inform sound prescribing decisions and ultimately curb growth of antibiotic resistance in the community and decrease ocular surface toxicity from antibiotic use. Moreover, the U.S. healthcare system could potentially save $430 million annually with accurate diagnosis of adenoviral conjunctivitis.8 When accounting for indirect costs from lost wages and disability, diagnosed cases of bacterial conjunctivitis cost the US health system up to an estimated $857 million a year.9
PREVENTION
Contaminated surfaces, fomites and hands are the main modes of adenovirus transmission. Frequent careful hand washing and disinfection of contaminated objects thus become paramount preventive efforts. Adenovirus is resistant to many types of disinfectants so it is crucial that specific “virucidal” agents are used. 70% isopropyl alcohol is ineffective against adenovirus.11 Ethanol-based formulations have better effectivity showing 99.99% viral inactivation after 30 seconds.12
Surfaces should be cleaned with EPA-registered disinfectants.13 Ideally, outpatients should not be put in the waiting room and should preferably be seen immediately, albeit impractical. Waiting room and exam room seats should be disinfected with a virucidal product. Providers and clinical staff should refrain from shaking hands with potentially infected patients, should always wear gloves when touching these patients, and should wash their hands before seeing another patient.14 If hospitalized patients become infected with extremely contagious strains like EKC, they should be put in isolated rooms.
EKC patients should not return to school or work while they are actively infected. Patients should be considered infectious if they still have injected conjunctiva and increased tearing. Viral shedding may persist for 10 to 14 days after the start of signs and symptoms. Information regarding the natural history of this disease should preclude frequent unannounced return visits, further breaking the chain of office transmission.15
CONCLUSION
Infectious conjunctivitis is one of the most common eye complaints, with the majority of cases initially presenting in a primary care or urgent care setting. A focused history taking and physical examination can help distinguish between viral and bacterial etiologies, or can shed light on red flag symptoms that oblige ophthalmology referral. Advancements in rapid diagnostic testing further assist with making early diagnosis of adenoviral conjunctivitis, saving patients from ocular surface toxicity and the financial burden of unwarranted antibiotic treatment. Cutting down on the over-diagnoses of bacterial conjunctivitis and increasing rates of accurate adenoviral conjunctivitis could potentially yield great economic savings and decrease long term morbidity for both patients and the healthcare system.
Citation: Dortonne I, Colmenares P, Lyford T, Sheppard J. Evaluation of infectious conjunctivitis by clinical evaluation and novel diagnostics. J Urgent Care Med. October 2019. Available at: https://www.jucm.com/evaluation-of-infectious-conjunctivitis-by-clinical-evaluation-and-novel-diagnostics/.
REFERENCES
- Abelson M, Shapiro A, Lapsa I. Meeting the Challenge Of Conjunctivitis. Rev Ophthalmol. com. https://www.reviewofophthalmology.com/article/meeting-the-challenge-of-conjunctivitis. Published June 13, 2006. Accessed 17 July 17, 2019.
- Shekhawat NS, Shtein RM, Blachley TS, Stein JD. Antibiotic prescription fills for acute conjunctivitis among enrollees in a large United States managed care network. Ophthalmol. 2017;124(8):1099-1107.
- Urgent Care Chart Survey. J Urgent Care Med.
- Azari A, Barney N. Conjunctivitis: A systematic review of diagnosis and treatment. 2013; 310:1721-1729.
- Garcia-Zalisnak D, Rapuano C, Sheppard J, Davis A. Adenovirus ocular infections: prevalence, pathology, pitfalls and practical pointers. Eye & Contact Lens. 2018;44:S1-S7.
- Keen M, Thompson M. Treatment of acute conjunctivitis in the United States and evidence of antibiotic overuse: isolated issue or a systematic problem? Ophthalmol. 2017;124:1096-1098.
- Sambursky R, Trattler W, Tauber S, et al. Sensitivity and specificity of the AdenoPlus test for diagnosing adenoviral conjunctivitis. JAMA Ophthalmol. 2013;131:17-22.
- Udeh B, Schneider J, Ohsfeldt R. Cost effectiveness of a point-of-care test for adenoviral conjunctivitis. Am J Med Sci. 2008;336:254-264.
- Smith AF, Waycaster C. Estimate of the direct and indirect annual cost of bacterial conjunctivitis in the United States. BMC Ophthalmology. 2009; 9(13):1-13.
- Bagheri N, Wajda BN. The Wills Eye Manual. 7th ed. Philadelphia, PA: Wolters Kluwer; 2017: 104-111.
- Koo D, Bouvier B, Wesley M, et al. Epidemic keratoconjunctivitis in a university medical center ophthalmology clinic; need for re-evaluation of the design and disinfection of instruments. Infect Control Hosp Epidemiol. 1989;10:547–552.
- Steinmann J, Becker B, Bischoff B, et al. Virucidal activity of 2 alcohol based formulations proposed as hand rubs by the World Health Organization. Am J Infect Control. 2010;38:66–68.
- AAO Cornea/External Disease PPP Panel. San Francisco, CA, Hoskins Center for Quality Eye Care; 2013.
- Meyer-Rusenberg B, Loderstadt U, Richard G, et al. Epidemic keratoconjunctivitis: The current situation and recommendations for prevention and treatment. Dtsch Arztebl Int. 2011;108:475–480.
- Ghebremedhin B. Human adenovirus: Viral pathogen with increasing importance. Eur J Microbiol Immunol. 2014;4:26–33.
Isabelle Dortonne, MD is a Resident at Eastern Virginia Medical School, Department of Ophthalmology. Patrizia Colmenares, OD is a Resident in Ocular Disease Optometry. Trevor Lyford, BA, OSC is an ophthalmic scribe and technician with Virginia Eye Consultants. John Sheppard, MD, MMSc is President of Virginia Eye Consultants and Professor of Ophthalmology at Eastern Virginia Medical School. Dr. Dortonne, Dr. Colmenares, and Mr. Lyford have no relevant financial relationships with any commercial interests. Dr. Sheppard has financial interests in TearLab, Johnson & Johnson Vision, Quidel, Allergan, Bausch + Lomb, Topcon, and Novartis.

John Sheppard, MD, MMSc

Isabelle Dortonne, MD

Patrizia Colmenares, MD

