Urgent message: Because bite and stings can be sustained in a variety of settings from many different animals and can transmit a wide variety of infectious agents, urgent care providers should have specific knowledge about treating wounds from mammals, nonmammals, and marine animals.
ALEXANDER NATHANSON, MD
Practitioners at urgent care centers often see patients who have sustained animal bites or stings. In addition to causing structural damage to tissues, bites and stings expose patients to potentially dangerous bacteria from animal oral flora or bacteria from the surface of the skin. In rare cases, bites can result in exposure to the rabies virus, and infection with the virus carries an extremely poor prognosis. Therefore, the need for rabies prophylaxis must be addressed in almost all cases of mammalian bites. Urgent care providers should also have some familiarity with certain bites and stings from nonmammals that can cause harm through envenomation, including snakes, scorpions, and marine wildlife such as stingrays, jellyfish, and siphonophores.
Mammals
Dogs
Overview
Dogs are responsible for about 80% of all animal bites in the United States. The breeds commonly implicated are German shepherds and pit bull terriers. Most dog bites come from dogs known to the individual, and the incidence of biting is higher in dogs that have not been neutered. Dog bites can result in scratches, abrasions, deep lacerations, puncture wounds, tissue avulsions, and crush injuries (Figure 1). Children are at a higher risk than adults are for being bitten by dogs.1 Because children are of similar height to many dogs, bites in children are commonly seen on the face, neck, and trunk. In adults, dog bites are most commonly seen on the hands.

Organisms
Infections from bite wounds are often polymicrobial because of a mix of bacteria can be introduced into the wound from the animal’s oral flora as well as from the patient’s skin. Most bite wound cultures from bites yield a mix of aerobic and anaerobic organisms. Pasteurella multocida is cultured in 50% of dog-bite infections.2 Staphylococcus and Streptococcus species are very common, including methicillin-resistant S. aureus (MRSA), the source of which can be either the animal or the patient’s skin.
Additionally, Capnocytophaga canimorsus, a gram-negative rod that can occasionally be isolated in a dog’s oral flora, can cause fulminant sepsis in some immunocompromised patients, including those with asplenia or cirrhosis.
Management
If a dog-bite wound is actively bleeding, direct pressure should be applied and full a neurovascular assessment should be performed of the areas distal to the wound. The wound should be thoroughly irrigated with normal saline. Anesthesia should be administered if necessary, and devitalized tissues should be debrided. If the bite occurs over the metacarpophalangeal joints on the hand, the wound should be explored in both the anatomic
position and the clenched-fist position.3 If a wound appears to be infected, a Gram stain and aerobic and anaerobic cultures can be obtained prior to initiation of antibiotics. Cultures of uninfected bite wounds are not useful in guiding antimicrobial treatment.4
Imaging can be useful in deep wounds or if the bite is located near a joint to evaluate for disruption of the bone or for the presence of foreign bodies such as teeth. Dog-bite wounds can be repaired if conditions are safe to do so. The wound should be clinically uninfected and less than 12 hours old if not on the face, or less than 24 hours if on the face. Avoid repairing crush injuries, puncture wounds, and wounds in immunocompromised hosts. Deep and complex wounds may require surgical consultation. After thorough irrigation, the wound should be repaired with primary closure. Avoid deep sutures, and avoid glue. Dog-bite wounds will generally need antibiotics if repaired.5 Uninfected wounds presenting less than 9 hours after injury do not need antimicrobial therapy if the wound is uncomplicated and properly irrigated. However, in patients presenting with full- thickness wounds more than 9 hours after the injury, prophylactic antibiotics have been shown to help prevent infection.6 Tetanus immunization status should be addressed in dog-bite wounds.
Cats
Overview
Cats are responsible for 10% to 20% of all animal bites in the United States, and cat bites tend to occur more frequently in women than in men or children. These bites are usually associated with handling the animal. Bite location is most commonly the face or upper extremities. Injuries often consists of deep puncture wounds with a small opening (Figure 2). When this type of wound occurs on the hand, bacteria can be inoculated into the periosteum or the joint space, which can result in tenosynovitis, osteomyelitis, or septic arthritis.
Organisms
Pasteurella multocida is isolated in 75% of cat-related wound infections, including both cat bites and catscratches.2 Staphylococcus, Streptococcus, and Moraxella species can also be found in infections from exposure to cats.
Another well-known organism that can be traced to a cat exposure is Bartonella henselae, which is responsible for cat-scratch disease. It can be transmitted through either a bite or a scratch from a cat, and also through fleas. A papule or pustule is often found at the inoculation site, and tender lymphadenopathy can develop 7 to 60 days after the initial exposure. The majority of the time, there is a solitary enlarged lymph node near the inoculation site; however, enlargement of multiple lymph nodes in the same region or different anatomic regions is a possibility. In some cases there can be visceral organ involvement of the liver and/or spleen, as well as visual disturbances from optic nerve involvement.
Management
Cat bites usually result in puncture wounds. In such cases, avoid high pressure irrigation of the wound. Instead, wounds can be soaked in antiseptic solution for 15 minutes. Inspect for evidence of deep tissue puncture. Punctures generally require antimicrobial therapy. They should not be repaired, because of the risk of trapping a deep-seated infection.
As with other animal bites, injury sites should be assessed for neurovascular compromise, and devitalized tissue should be debrided. Bacterial culture can be obtained if there is evidence of infection. Although cat-scratch wounds have the potential to be contaminated with the same organisms as bites, they likely do not require the same aggressive approach as bite wounds do. If the wound is thoroughly irrigated and the patient presents less than 9 hours after sustaining it, then it likely will not require antibiotics unless there is clear evidence of infection. Tetanus immunization status should be addressed in cat-bite wounds.
Cat-scratch disease is commonly associated with prolonged fever, and it should be considered when evaluating for fever of unknown origin, especially in children. This diagnosis can be usually be confirmed with serology. Cat-scratch disease usually responds to azithro mycin, but systemic infections may require additional antimicrobial therapy.

Humans
Presentation
Human bites can occur in a variety of situations. Minor bites can occur during sexual activity, and they can occur secondary to psychiatric illness. In children, bites can be seen from play-fighting. However, if the bite has an intercanine distance of more than 3 cm, the bite likely came from an adult, and this should raise concerns about child abuse.7 Some of the most dangerous human bites happen when there is an injury to a closed fist, such as in a fistfight when a fist comes into contact with another individual’s teeth. These are usually small lacerations over the third and fourth metacarpophalangeal or proximal interphalangeal joints on the dominant hand. These wounds are highly prone to infection, given the proximity of the skin to the joint spaces.
Organisms
Bites from humans tend to have a higher complication rate than bites from dogs or cats, largely because of the greater variety of pathogenic organisms isolated from infected wounds. Pasteurella is occasionally seen, as are Staphylococcus and Streptococcus species. Eikenella corrodens is a gram-negative organism found in the human oral flora that is unique to human-bite infections.8
Management
In human bites, risks for transmission of blood-borne pathogens should be considered. Individuals who have not been vaccinated for hepatitis B and those for whom the vaccine is ineffective (i.e., they are HBsAb negative) are at risk and should receive the hepatitis B vaccine series. If the source of the bite is positive for the hepatitis B surface antigen, those who are not immune should receive hepatitis B immunoglobulin in addition to the full vaccine series. Human immunodeficiency virus and hepatitis C are very rarely transmitted through saliva alone, unless there is visible blood in the saliva.9,10
As with other animal bites, human bite injuries should be assessed for neurovascular compromise. Wounds should be thoroughly irrigated. Wounds over the metacarpophalangeal or proximal interphalangeal joints should be explored in both the anatomic position and the clenchedfist position. Because of the higher complication rate associated with human bites in comparison with other animal bites, extra caution should be taken when deciding whether to repair the wound. Avoid repairing bite wounds to the hand and puncture wounds. Head and neck wounds may be considered for repair if clinically uninfected. In general, all full-thickness human-bite wounds should be treated with prophylactic antibiotics. Tetanus immunization status should also be addressed.
Rodents
Organisms and Presentation
Bites from rodents are often seen in individuals who care for these animals or house them as pets. Rodent bites are often too small to be clearly seen. These bites can become infected 10% of the time, commonly by Streptobacillus moniliformis and Spirillum minus.11 These organisms can cause a rare condition known as rat-bite fever. The incubation period for this illness is usually less than 7 days. Generalized flu-like symptoms, such as fever, headache, and pharyngitis, are first to appear. Afterward, patients may develop a maculopapular rash on the extremities and polyarthritis. Rare complications include meningitis, as well as endocarditis in those with a history of heart valve disease.
Management
The organisms in these bites are difficult to isolate in cultures and should be suspected and treated empirically in patients with a history of rodent exposure. Rat-bite fever usually responds well to penicillin and ceftriaxone. It can remit and relapse in untreated patients.
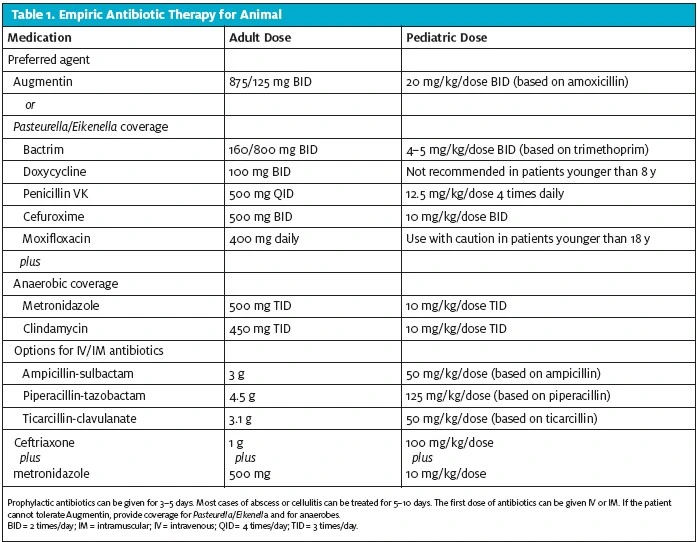
Antibiotics in the Treatment of Mammalian Bites
Antibiotics should be chosen to cover the specific organisms commonly found in animal bites, such as Pasteurella and Eikenella, as well as anaerobes. Coverage for MRSA should be considered. Among oral agents, Augmentin (amoxicillin clavulanate) is the first choice. If MRSA coverage is required, doxycycline or Bactrim (trimethoprim-sulfamethoxazole) can be added. Clindamycin covers anaerobes, but it is not recommended as a solo agent, owing to poor Pasteurella coverage.
In cases of more severe infections, the first dose of antibiotics can be given intramuscularly or intravenously. Options include Unasyn (ampicillin-sulbactam), Zosyn (piperacillin-tazobactam), and a third-generation cephalosporin plus Flagyl (metronidazole).
Prophylactic antibiotics can be given for 3 to 5 days. Most abscesses or cellulitis can be treated for 5 to 10 days.12 Deeper infections such as tenosynovitis or osteomyelitis may require a combination of parenteral and oral antibiotics for a significantly longer duration.
Table 1 gives details on empiric antibiotic therapy for animal bites.
Rabies
Overview
Rabies is a viral illness that can be contracted from the bites of mammals that carry it. It is characterized by motor weakness, paresthesias, and encephalitis, eventually leading to coma and death. In patients with established rabies, the illness is almost always fatal. Rabies is transmitted through an animal’s saliva. It has an incubation period of 1 to 3 months. Around the world, 50,000 people die of rabies every year, whereas in the United States, 2 or 3 people die every year because of it.13 Dogs are responsible for 95% of rabies transmissions to humans around the world. However, in the United States, vaccination programs have effectively eliminated domestic dogs as a reservoir, except for certain cases in the Southwest along the border between the United States and Mexico. There are actually more rabid domestic cats than rabid dogs in the United States because there are fewer vaccination laws for the former than for the latter.
In the United States, bats are the most common source of transmission. Raccoons, foxes, coyotes, and skunks are the most commonly infected terrestrial animals. Although there have been reports of rabies in larger rodents such as beavers and woodchucks, rabies is almost never found in smaller rodents such as squirrels, chipmunks, mice, rats, hamster, gerbils, or guinea pigs. There has never been a documented transmission of rabies to humans from one of these animals.
The decision on whether to administer post exposure prophylaxis for rabies depends on a number of factors. Consultation with local public health officials can provide information about the epidemiology of rabies in the immediate geographic area.
Exposure to bats appears to carry the highest risk. Rabies has been found in bats in almost all states in the United States. Bat bites are small and often unseen. If an individual is awake and aware of the bat at all times, then prophylaxis is not necessary. However, if an individual awakes to find a bat in the bedroom, or if a young child, mentally disabled person, or intoxicated person is found to be exposed to a bat, then prophylaxis should be administered unless the bat can be captured and tested. Bites from wild terrestrial animals such as raccoons, coyotes, or skunks should be considered high risk, and prophylaxis should begin immediately, especially if the bite is in a high-risk anatomic area close to the central nervous system, such as the head or neck. If the animal is captured, tested, and found to be free of rabies, then the vaccine series can stop. If the exposure is lower risk, such in the case of a superficial bite or scratch far from the central nervous system, and the animal is captured, then prophylaxis can wait for until the animal is tested.
In the United States, the risk of rabies exposure from a domestic dog or cat bite is very low, and the decision over whether post exposure prophylaxis is required depends on factors such as the vaccination status of the animal and whether the attack was provoked or unprovoked.
Risk Factors
A bite to an individual trying to handle or feed an animal should be considered a provoked attack. This type of behavior is not suspicious for rabies infection. However, an unprovoked attack, such as if an animal runs up and bites an individual without any provocation, is more concerning. If possible, this animal should be examined for any bites or wounds that would give clues about rabies exposure. A healthy dog or cat that bites a person should be observed for 10 days, because this is the time period during which an animal will show clear signs of rabies if it is present. However, if the bite occurs on the head or neck, then prophylaxis should begin, because the incubation period for rabies can be significantly shorter than those 10 days. Dog bites that occur outside of the United States, especially in the developing world, should be considered high risk, because in most cases of rabies in the United States, the disease is transmitted by dogs from developing countries rather than by domestic dogs.13
Management
When administering rabies prophylaxis, begin with thorough cleansing of the wound with soap and water. Consider soaking the wound in a virucidal agent such as iodine. Proper wound cleansing can prevent the likelihood of rabies transmission in up to 90% of cases.14 Postexposure prophylaxis usually requires a combination of both passive and active immunization. Rabies immunoglobulin provides immediate virus-neutralizing antibodies. The full volume of the immunoglobulin dose should be injected in and around the wound. If there is no clear wound, then this should be administered into the gluteal muscles. Additionally, a rabies vaccine should be administered at the same time and again on days 3, 7, and 14.15 The vaccine induces the formation of antibodies that take effect about 1 week after exposure. The vaccine should be administered at a different site from where the immunoglobulin is injected.
Certain high-risk groups such as veterinarians and laboratory workers may have received pre-exposure prophylaxis with the vaccine. In such cases, no rabies immunoglobulin is necessary. Vaccines should be administered on days 0 and 3.15
Snakes
Overview
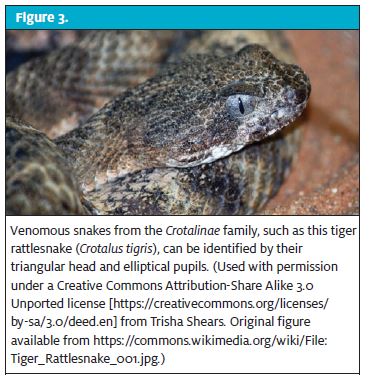
Venomous snakes can be encountered in wilderness areas throughout the United States. Most snake bites in the United States are caused by members of the Crotalinae family, specifically rattlesnakes (Figure 3), copperheads, and water moccasins, which are collectively known as pit vipers. Although venomous snakes can live in almost all parts of the United States, most bites occur in the Southwest. Rattlesnakes are the most dangerous of venomous snakes and account for the majority of fatalities attributed to snake bites. Venomous snakes usually have some distinctive characteristics, such a triangular head, elliptical pupils, and hollow fangs,16 that allow them to be identified from a distance so as to avoid encountering them up close or capturing them.
Bites can present as one or two deep puncture wounds. A bitten individual should be kept calm, and the affected area should be elevated and immobilized before the person is transferred to an emergency department. Physicians should not attempt any aggressive techniques such a tourniquets, suctioning, or pressure immobilization.17
Crotalinae secrete a hemotoxic venom that can cause affects ranging from local reaction and swelling to compartment syndrome, rhabdomyolysis, and disseminated intravascular coagulation–like (DIC-like) syndrome. Severity depends on the amount of venom injected and the species of snake responsible for the attack. Antivenin is available for moderate to severe envenomations, and it has been responsible for significantly decreasing the mortality rate for snake bites, which is currently less than 1%.
Unlike Crotalinae, coral snakes secrete a neurotoxic venom. They are found in the U.S. South and Southeast and can be identified by their brightly colored pattern of adjacent yellow and red bands (Figure 4). Coral snakes are nonaggressive and will bite only if provoked. However, their bites are small and can be easy to miss. Symptoms include local numbness, cranial nerve palsies, and, in severe cases, respiratory depression and airway compromise. Patients with bites should be monitored for any signs of respiratory depression over a period of time. Antivenin can be used when it is available

Scorpions
Overview
Encounters with scorpions occur in the U.S. Southwest, and such encounters are a significant problem over the border in Mexico, where deaths from scorpion stings outnumber deaths from snake bites 10 to 1. In the United States, there has not been a confirmed death from a scorpion sting since 1968. Although several species of scorpion can produce clinically significant symptoms, most stings in the United States are attributed to Centruroides exilicauda, commonly known as the bark scorpion, which likes to reside under trees and rocks and has the highest potential of all scorpion species for inducing systemic symptoms. Scorpions are not typically aggressive and will usually sting only if stepped on or cornered.
Presentation
A low-grade reaction to scorpion venom may present as only local pain and paresthesia. The tap test has been recommended for differentiating the sting of a bark scorpion from other ailments, including stings from other scorpion species. To perform the test, have the patient look away while you gently tap the wound. A sting from a bark scorpion will produce significantly exacerbated pain. Moderate to severe envenomations can cause cranial nerve palsies and/or neuromuscular dysfunction. Cranial nerve palsies can present as blurred vision, abnormal eye movements, tongue fasciculations, and hypersalivation. Airway maintenance can be a concern in patients with scorpion sings. Neuromuscular symptoms can include restlessness, fasciculations, and shaking and jerking of the extremities, which can mimic a seizure, except that the patient will likely be awake and alert. Scorpion sting envenomation can be more severe in children than in adults because of their smaller size.18
Management
Supportive care is the mainstay of managing scorpion bites. Local or generalized analgesia should be given as needed. Benzodiazepines can be given for motor neuron hyperactivity, and atropine can be given to combat excessive cholinergic activity. For severe envenomations, scorpion antivenin can be obtained.
Marine Animals
Populations including fishers, swimmers, snorkelers, and aquarium workers may be at risk for stings from certain types of venomous marine wildlife. Catfish spines can cause injury to fishers who are removing them from a fishing line. Scorpionfish and lionfish are often found in commercial and home aquariums and can cause injury during their routine care and feeding. Other marine animals, including sea urchins, coral, and stonefish, cause injury during accidental contact, such as when they are stepped on. In the case of sea urchins, multiple spines can break off and become embedded deep in tissues.
Stingrays
Overview
Stingrays can be somewhat more dangerous. They often attack in the late summer to early fall when they burrow in the shallow surf, where they can be accidentally stepped on. Stingrays possess whiplike tails with venom containing spines at the end. When the animal is stimulated or frightened, it flings its tail upward, embedding the spines in the victim. Advise patients that when they are walking in the surf, they can prevent stingray attacks by shuffling their feet. This prevents their stepping down hard onto a stinger, and the movement alerts stingrays to their presence.
Management
Stingray envenomations cause immediate localized pain. Any systemic symptoms are usually from severe pain rather than from the envenomation. For pain control, wounds should be immersed in hot water at 40° to 45°C for up to 90 minutes.19 Additional analgesia with nonsteroidal anti-inflammatory drugs or opiates may be needed. The wound should be copiously irrigated, and any foreign bodies should be removed. Retained spines from sea urchin encounters are usually visible on radiographs. Stingray attacks may require more extensive imaging to rule out penetrating trauma. [Editor’s note: See also “Stingray Envenomation and Subsequent Skin and Soft-Tissue Infection Due to Vibrio parahaemolyticus and Aeromonas hydrophila” in this issue.]
Jellyfish and Similar Marine Animals
Overview
Another common cause of marine envenomation comes from jellyfish. Jellyfish live in coastal waters all over the world, and swimmers can be stung if they make contact with their tentacles. As with other marine envenomations, patients will experience immediate pain. Several minutes later they may develop a linear red or urticarial rash. However, this rash is not always immediate and can present several hours later. Jellyfish venom can have local and systemic effects. Outside the United States, the Australian box jellyfish has been associated with no fewer than 70 deaths. In the United States, jellyfish stings are usually mild. The severity of the sting depends on the type of jellyfish and the amount of skin contact with the tentacles.
On the East Coast of the United States, there have been encounters with the Portuguese man-of-war (Physalia physalis), which is often mistaken for a jellyfish but is instead a siphonophore, a colony of organisms that work together as one animal (Figure 5). It produces a very painful sting. Rare deaths have been reported because of these animals, either through cardiac arrest, respiratory arrest, or drowning due to limb paralysis.

Management
In patients stung by a jellyfish or siphonophore, remove any tentacle contents from the skin promptly but not aggressively. Studies of encounters with the Portuguese man-of-war and the Hawaiian box jellyfish have demonstrated the benefit of immersion in hot water of the affected area. This appears to be provide better pain control than other previously suggested remedies such as acetic acid or meat tenderizer.20
Conclusion
To successfully manage animal bites and stings, providers should have knowledge of the risks associated with the specific types of bites and stings that can occur. All bite and sting wounds should be carefully cleaned, and the structural integrity of the affected body part should be evaluated. Tetanus status should always be addressed. Providers should be vigilant about the risks of performing primary closure of bite wounds and should be aware of the contraindications to such repairs. When providing antimicrobial therapy, clinicians should be careful to choose antibiotic agents that provide coverage for Pasteurella, Eikenella, and anaerobes. Providers should also be able to assess the risk for rabies and know when to provide rabies prophylaxis. Additionally, although most of the bite wounds that patients present with are from mammals, providers should have some familiarity with nonmammalian bites and stings, specifically from snakes, scorpions, and marine animals.
References
- Avner JR, Baker MD. Dog bites in urban children. Pediatrics. 1991;88:55–57.
- Francis DP, Holmes MA, Brandon G. Pasteurella multocida: infections after domestic animal bites and scratches. JAMA. 1975;33:42–45.
- McDonald LS, Bavaro MF, Hofmeister EP, Kroonen LT. Hand infections. J Hand Surg Am. 2011;36:1403–1412.
- Talan DA, Citron DM, Abrahamian FM; Emergency Medicine Animal Bite Infection Study Group. Bacteriologic analysis of infected dog and cat bites. N Engl J Med. 1999;340:85–92.
- Fleisher GR. The management of bite wounds. N Engl J Med. 1999;340:138–140.
- Brakenbury PH, Muwanga C. A comparative double blind study of amoxycillin/clavulanate vs placebo in the prevention of infection after animal bites. Arch Emerg Med. 1989;6:251–256.
- Kellogg ND; American Academy of Pediatrics Committee on Child Abuse and Neglect. Evaluation of suspected child physical abuse. Pediatrics. 2007;119:1232–1241.
- Rayan GM, Putnam JL, Cahill SL, Flournoy DJ. Eikenella corrodens in human mouth flora. J Hand Surg Am. 1988;13:953–956.
- Richman KM, Rickman LS. The potential for transmission of human immunodeficiency virus through human bites. J Acquir Immune Defic Syndr. 1993;6:402–406.
- Lohiya GS, Tan-Figueroa L, Lohiya S, Lohiya S. Human bites: bloodborne pathogen risk and postexposure follow-up algorithm. J Natl Med Assoc. 2013;105:92–95.
- Elliott SP. Rat bite fever and Streptobacillus moniliformis. Clin Microbiol Rev. 2007; 20:13–22.
- Stevens DL, Bisno AL, Chambers HF, et al. Executive summary: practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e10–e52. [See also Stevens DL et al, Clin Infect Dis 2014;59:147–159 for corrections regarding cell counts and dosages. Available from: http://cid.oxfordjournals.org/content/60/9/1448.2.long]
- Human rabies. Atlanta, GA: Centers for Disease Control and Prevention [updated 2012 May 3; cited 2015 August 6]. Available from http://www.cdc.gov/rabies/location/usa/surveillance/human_rabies.html
- Dean DJ, Baer GM, Thompson WR. Studies on the local treatment of rabies-infected wounds. Bull World Health Organ. 1963;28:477–486.Rupprecht CE, Briggs D, Brown CM; Centers for Disease Control and Prevention (CDC).
- Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep. 2010;59(RR-2):1–9. Gold BS, Dart RC, Barish RA. Bites of venomous snakes. N Engl J Med. 2002;347: 347–356.
- American College of Medical Toxicology; American Academy of Clinical Toxicology;
- American Association of Poison Control Centers; European Association of Poison Control Centres and Clinical Toxicologists; International Society on Toxinology; Asia Pacific Association of Medical Toxicology. Pressure immobilization after North American Crotalinae snake envenomation. Clin Toxicol (Phila). 2011;49881–882.
- Curry SC, Vance MV, Ryan PJ, et al. Envenomation by the scorpion Centruroides sculpturatus. J Toxicol Clin Toxicol. 1983;21:417–449.
- Clark RF, Girard RH, Rao D, et al. Stingray envenomation: a retrospective review of clinical presentation and treatment in 119 cases. J Emerg Med. 2007;33:33–37.
- Nomura JT, Sato RL, Ahern RM, et al. A randomized paired comparison trial of cutaneous treatments for acute jellyfish (Carybdea alata) stings. Am J Emerg Med. 2002;20:624–626.