Urgent message: Urgent care centers are encouraged to meet best practices for communication during transitions of care. Partnering with pharmacists may optimize medication therapy for patients, helping fulfill these best practices.
JENNIFER A. FLAVIN, PharmD, CHRISTOPHER G. GREEN, PharmD, STEPHANIE C. COOK, DO, and STUART J. BEATTY, PharmD, BCACP
Objective: This study aimed to (1) evaluate the impact of a pharmacist-provided comprehensive medication review (CMR) service on medication therapy appropriateness, safety, efficacy, and adherence for urgent care patients and (2) identify the workflow considerations required for incorporation of the service in an urgent care practice. Methods: In this prospective study of a nonrandomized convenience sample, pharmacists reviewed the electronic medical records of scheduled urgent care patients to identify those with at least 4 chronic medications and 1 chronic disease state. On completion of the patients’ urgent care visit, clinic staff members recruited eligible patients for a pharmacist-provided CMR within the following 28 days. CMR interventions were communicated to the patient’s primary-care provider. A follow-up phone call to the patient 1 week after the CMR visit and a chart review 1 month after the visit were completed to determine the acceptance of interventions by the patient and provider, respectively. Descriptive statistics were used to report primary and secondary outcomes. Results: In the 28-week study, 76 patients accepted the offer for a CMR. Of those, 29 patients (38%) completed their CMR and consented for inclusion in the study. Pharmacists identified a total of 166 interventions. These interventions addressed issues of appropriateness (44%), adherence (23%), efficacy (20%), and safety (13%). Conclusion: Results demonstrate optimization of medication therapy for urgent care patients through a pharmacist-provided CMR service. These findings may help support future partnerships between pharmacists and urgent care practices.
Introduction
It is predicted that almost 52,000 additional primary care providers (PCPs) will be required to serve the health-care needs of the U.S. population in the next 10 years.1 This shortage, combined with increased demand for emergency department (ED) services, has led to an increase in the use of urgent care centers and retail clinics as cost-effective and time-saving options for care. A 2010 comparison of visits between urgent care, retail clinics, and EDs determined that a significant portion of ED visits were for nonemergency conditions. Researchers estimated that treating these conditions at urgent care centers or retail clinics instead of in an ED could save up to $4.4 billion in health costs annually.2 In response to this opportunity, 50 to 100 new walk-in, stand-alone urgent care centers are opening every year, according to the American Academy of Urgent Care Medicine.1
With the increase in use of urgent care centers comes a need for quality standards for communication from the urgent care center to the primary-care office during transitions of care. In 2008, a national survey found that one-third of urgent care providers did not send information to their patients’ PCPs and that those who communicated did not do so consistently. In the same year, the Centers for Medicare & Medicaid Services (CMS) called for the design of best practices for urgent care communication during patient-care transitions to EDs or back to primary care. This set of standards, the CMS Best Practices for Urgent Care Transitions, was published in July 2014 and requires that at the end of each urgent care visit, as a patient transitions back into primary care, clinical information must be sent to the patient’s PCP, medication reconciliation must be completed, and the patient must be provided with effective education about their therapy. To comply with these standards, medication reconciliation should include identification of potential medication errors; explanation of which medications should be stopped, started, or adjusted; and preparation of an accurate list of medications to be given to the patient and provider. Additionally, patients must be educated about the importance of longitudinal care and referred to a PCP if they do not already have one.3
University Health Services is an interprofessional team-based clinic composed of physicians, nursepractitioners, pharmacists, and nurses who provide urgent care services to employees of the Ohio State University (OSU). The urgent care service is a benefit of the OSU health plan used by approximately 80 employees weekly. In addition to diagnosis and triage of acute needs, these urgent care visits serve as a touchpoint for patients with chronic medical conditions and medications who may not have adequate medication management or who may experience fragmented care. Clinical pharmacists at University Health Services offer a comprehensive medication review (CMR) as standard of care to patients prescribed multiple chronic medications, to patients with multiple diagnosed chronic disease states, or on referral from the urgent care physician.
Pharmacist-provided medication reviews have demonstrated positive effects on clinical outcomes, adherence to medication therapy, hospital readmission rates, mortality, patient satisfaction, and cost savings.4,5 By definition, a CMR is a component of a medication therapy management service that includes an assessment of all medication therapies with identification of any medication-related problems, preparation of a personal medication record for the patient, a medicationrelated action plan for patient self-management, and documentation of service provided and recommended interventions to the PCP and other providers, as appropriate. 6 Figure 1 illustrates the overlap in elements of a medication therapy management service and these best practices for care transitions. Although a CMR can lead to improved patient outcomes, there is little information in the literature regarding the impact of CMR in the urgent care setting.
Study Purpose
We conducted a study to evaluate the impact of a pharmacist-provided CMR service on medication therapy appropriateness, safety, efficacy, and adherence for urgent care patients and to identify the workflow considerations required for incorporation of the service in an urgent care practice.
Methods
Ours was a prospective interventional 6-month pilot study of a nonrandomized convenience sample. The project was approved by the OSU institutional review board.
Study investigators screened the electronic health records (EHRs) of all patients scheduled for same-day urgent care appointments in an employee based clinic to identify those who were eligible for the CMR service. To be eligible for participation, patients were required to take 4 or more chronic medications, have 1 or more chronic disease states, be at least 18 years of age, speak English as their primary language, have OSU health insurance, and have no documentation of a CMR in their EHR in the preceding year. Eligible patients were flagged on the clinic schedule for recruitment. Clinic staff members offered eligible patients the opportunity to review their medications with a pharmacist on completion of their urgent care visit. Patients who accepted the offer for a CMR were scheduled for the encounter by front desk staff members. CMR encounters were encouraged to be completed immediately after the urgent care visit. Patients unable to complete the CMR immediately after the urgent care visit were asked to schedule an appointment for a CMR within the 28 days that followed.
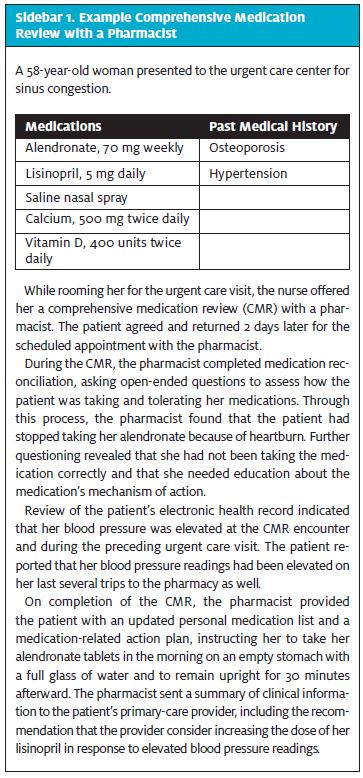
At the time of their CMR encounter, the patient met with a pharmacist to review all of their medications, including any changes made during the urgent care encounter. All medications were screened for a documented indication, effectiveness in treating the indication, potential for safety issues, and patient adherence. At the end of the CMR visit, the patient was provided with a medication-related action plan that included any interventions made directly with the patient and an updated personal medication record. When applicable, documented interventions were routed to the patient’s prescriber in addition to the summary of the CMR visit. Sidebar 1 summarizes an example CMR encounter with a pharmacist. Patients received a follow-up phone call 1 week after their CMR encounter to assess whether interventions made with the patient were accepted.
One month after the CMR encounter, researchers reviewed the patient’s EHR to determine if interventions made with the provider were accepted. Interventions were grouped by type of drug-related problem addressed and were categorized into those addressing medication therapy indication, safety, efficacy, and adherence. Interventions categorized as addressing indication for medication included untreated medical condition, unnecessary therapy, suboptimal drug, duplicate therapy, preventative therapy needed, immunization needed, and over-the-counter therapy recommendation. Interventions categorized as addressing safety of medication therapy included adverse drug reaction, drug interaction, contraindication, dose too high, needs monitoring for safety, and duration of therapy too long. Interventions categorized as addressing efficacy of medication therapy included dose too low, needs monitoring for efficacy, and cost-efficacy. Interventions categorized as addressing patient adherence to medication therapy included overuse, underuse, and inappropriate administration. A single researcher categorized interventions for consistency across CMR encounters that were completed by 3 different pharmacists.
The determination of whether a provider was the most appropriate recipient of an intervention was based on the need for a prescription or other order, whether consultation with the prescriber was necessary, and whether it was more suitable for the intervention to be addressed at a future primary-care visit for continuity of care. For example, if an indication for an immunization was identified, patients were given the opportunity to have the vaccine administered during their CMR encounter under a standing protocol with the medical director. Interventions regarding indication for an immunization were made with the PCP if the patient was unable to receive the immunization at the time of the CMR encounter. When this occurred, the outcome from the prescriber was recorded rather than the outcome from the patient.
Results
Sample Characteristics and Recruitment
During the 24-week study period, 1546 urgent care visits were completed. Of the 274 urgent care patients who met the eligibility criteria for a CMR, 138 patients were offered a CMR. A total of 76 patients agreed to a CMR, and 29 of those completed the CMR within 28 days of their urgent care visit and consented for inclusion in the study.
Table 1 provides an overview of demographic information collected. The majority of participants were female and white and had a mean age of 48.8 years (SD, 12.0 years). Patients who completed a CMR took an average of 8.4 (SD, 3.2) chronic medications and had an average of 3.8 (SD, 1.7) chronic medical conditions. The average time elapsed since the last primary-care visit was 7.6 (SD, 7.1) months. The average time elapsed from urgent care visit to CMR visit was 10.3 (SD, 8.8) days, with only 14% of patients choosing to complete their CMR immediately after their urgent care visit. The average time spent in the CMR visit was 42.4 (SD, 21.6) minutes.
Comprehensive Medication Review Interventions
Identified
In the 29 CMR encounters, pharmacists identified a total of 166 interventions, with a mean of 5.7 (SD, 3.4) interventions per patient. These interventions were classified according to type (Figure 2) as addressing indication (44%), adherence (23%), efficacy (20%), and safety (13%). The most common interventions made overall were indication for immunization (indication), underuse (adherence), and need for monitoring for efficacy (efficacy).
Outcomes of Comprehensive Medication Review
Interventions with Patients
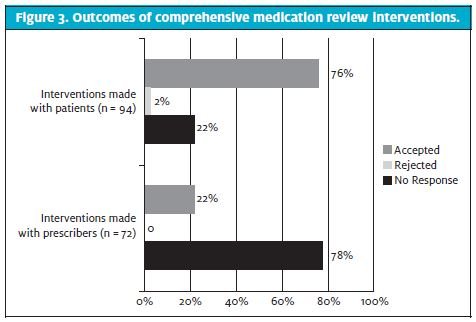
Ninety-four of the 166 total interventions (57%) were made directly with patients (Figure 2), with the most common being underuse (adherence), inappropriate administration (adherence), and over-the-counter therapy recommendation (indication). One week after the CMR encounter, patients reported accepting 76% of interventions and rejecting 2% of interventions; 22% of interventions had no response or no response could not be determined by a follow-up phone call (Figure 3).
Outcomes of Comprehensive
Medication Review Interventions with Providers
Seventy-two of the 166 total interventions (43%) were made with prescribers (Figure 2), with the most common being need for immunization (indication), need for monitoring for efficacy (efficacy), and untreated medical condition (indication). One month after the CMR encounter, EHR review indicated that prescribers accepted 22% of interventions (Figure 3). For the remaining 78% of interventions, there was no response or no response could be determined by a follow-up chart review.
Discussion
Urgent care centers are used by patients with fragmented care who may benefit from medication management with a pharmacist. With an aging population and increasing burden of chronic conditions, prescription medication use has grown since the beginning of the 21st century.7 Whether patients have a PCP with limited accessibility or they do not have a PCP at all, some urgent care centers are providing preventative services as well as care for ongoing chronic conditions.8 All patients included in this study had a self- identified PCP, with most having consulted their PCP in the preceding 6 to 12 months. Despite this, and despite average of 8.4 chronic medications and 3.8 chronic medical conditions for each patient, pharmacists were able to identify an average of 6 interventions to optimize medication therapy for each patient included in the study. These interventions indicate an opportunity for optimization of medication therapy in the urgent care population.
More than half of the interventions made during the CMRs were resolved between the patient and pharmacist and communicated to the PCP. The majority of these interventions related to adherence and safety, allowing issues of nonadherence from medication underuse or inappropriate administration and adverse drug reactions to be corrected directly with the patient at the time of the visit. Interventions related to indication for drug therapy were split evenly between providers and patients, with over-the-counter medication therapy recommendations representing the most common intervention made with patients in this category. High acceptance rates for patient-addressed medication-related problems suggest that patients are receptive to pharmacist interventions in the urgent care setting.
The majority of interventions related to efficacy of medication therapy were made with prescribers, because they frequently involved a recommendation for an order to be placed. Documented acceptance rates of interventions made with prescribers were lower than for those made with patients, which may represent a limitation of the chosen follow-up methods. The large percentage of interventions made with providers that had no response suggests that review of the EHR 1 month after the CMR encounter did not often reveal the outcome of the intervention. Prescribers might or might not have been receptive to the recommendations or might have intended to address them at follow up, but they did not document their response in the chart within a month of the communication. Although an extension of the follow-up period would impact the extent to which the outcome could be directly related to the intervention made during the CMR encounter, direct communication with prescribers through a phone call, instead of passive communication through the EHR, might have resulted in more documented responses.
The CMS Best Practices for Urgent Care Transitions3 were designed to improve partnerships between urgent care centers and PCPs, but they may also represent an opportunity for partnerships between urgent care practices and pharmacists. The pharmacist-provided CMR service included elements that met the best practice standards, including medication reconciliation and review, patient education and discharge instructions in the form of a medication-related action plan, and a summary of clinical information sent to the patient’s PCP.
Although recommendations were sent to prescribers directly along with the summary of the encounter, patients were also informed that their prescribers were being contacted and were encouraged to discuss the issues identified in their medication-related action plan with their prescribers to achieve a resolution. Although the response rates from prescribers were low, some replied with a message of gratitude, indicating appreciation for the service and/or communication. A future direction for study would be to measure provider and patient satisfaction with the service.
Pharmacists complete CMRs in a variety of practice environments, including clinic settings, community pharmacies, long-term-care facilities, and health systems. In the urgent care setting, patients are often seen on a walk-in basis, with little opportunity for workup. The fast paced nature of an urgent care practice can make incorporation of the CMS best practices for care transitions challenging. Pharmacists are uniquely trained to identify opportunities to optimize medication therapy and can complete a CMR with minimal preparation when necessary. Despite the option to be seen immediately after completion of their urgent care visit, only 4 of 29 patients in our study chose to complete their CMR the same day. Patients might have opted to schedule their CMR visit for another time so that they could return home or to work. Only 18% of the urgent care patients seen during the study period met the criteria of ≥4 chronic medications and ≥1 chronic disease state, which might be a factor of the age and general health status of the employee population. The single-payer, employee-based model of the clinic was a limitation of the study. Implementation of the CMR service in a more public urgent care setting may result in improved use of the service.
The small sample size was another limitation of the study. Only half of the patients who met eligibility criteria were offered a CMR with the pharmacist. This represents a barrier to incorporation of the service into the normal operations of an urgent care clinic. The pharmacists performing the study have many responsibilities outside of the CMR service. As a result, there was a heavy reliance on the nursing staff to recruit eligible patients for the service.
Additionally, flagging of the clinic schedule might not have been the most effective way to signal clinic staff to recruit eligible patients. A contributing factor to the poor recruitment rate was a change in nursing and urgent care provider staff during the study. With consistent staffing and a designated pharmacist managing the service, patients could have been recruited more effectively.
Few urgent care centers have pharmacists on staff, because of the expense associated with employment of an additional health-care provider. Some avenues to help pay for a pharmacist include CMR reimbursement and value-based payment models. Completion of a CMR by a credentialed pharmacist is a reimbursable service under some health plans. Association of the interventions made during the CMRs with cost savings to the health plan is another future consideration for this study. Incorporation of pharmacists into the health-care team is further supported by the move toward a value-based payment structure, with pharmacist- provided medication therapy management associated with improved health-care quality and cost savings. Colleges of pharmacy seeking unique practice sites for training of student pharmacists and pharmacy residents may represent opportunities for collaboration. Additionally, urgent care centers and retail clinics are often located in close proximity to community pharmacies to allow for convenient medication dispensing for patients. These pharmacies are potential partners for shared services with the common goal to optimize medication therapy and communication during care transitions.
Conclusion
Urgent care center use by patients with chronic medical conditions and medications provides a unique opportunity for pharmacists to optimize medication therapy. The results of our study demonstrated the impact of a pharmacist-provided CMR service on medication therapy appropriateness, safety, efficacy, and adherence for urgent care patients. The provision of a CMR can help meet CMS standards through inclusion of elements of care coordination through transitions that may help support future partnerships between pharmacists and urgent care practices.
References
- American Academy of Urgent Care Medicine. Future of urgent care. Orlando, FL: American Academy of Urgent Care Medicine [© 2014; accessed 2014 July 27]. Available from: http://aaucm.org/about/future/default.aspx
- Weinick RM, Burns, RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Millwood). 2010;29:1630–1636.
- Shamji H, Baier RR, Gravenstein S, Gardner RL. Improving the quality of care and communication during patient transitions: best practices for urgent care centers. Jt Comm J Qual Patient Saf. 2014; 40: 319–324.
- Hatah E, Braund R, Tordoff J, Duffull SB. A systematic review and meta-analysis of pharmacist-led fee-for-services medication review. Br J Clin Pharmacol. 2014; 77:102–115.
- Ramalho de Oliveira D, Brummel AR, Miller DB. Medication therapy management: 10 years of experience in a large integrated health care system. J Manag Care Pharm. 2010;16:185–195.
- American Pharmacists Association; National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model (version 2.0). .J Am Pharm Assoc (2003). 2008;48:341–353.
- Gu Q, Dillon CF, Burt VL. Prescription drug use continues to increase: U.S. prescription drug data for 2007–2008. NCHS Data Brief. 2010;42:1–8.
- Urgent Care Association. Industry FAQs. Naperville, IL: Urgent Care Association [accessed 2014 July 15]. Available from http://www.ucaoa.org/general/ custom.asp?page=IndustryFAQs
