Urgent message: Proper empiric antibiotic treatment in women with acute uncomplicated cystitis and pyelonephritis can prevent unnecessary morbidity and provide urgent relief from these common genitourinary infections.
MOZELLA WILLIAMS, MD
Genitourinary infections in women are encountered frequently in the urgent care setting. Timely diagnosis and proper empiric antibiotic treatment will usually forestall serious complications and provide speedy relief. Over a lifetime, 50% of women will experience an acute uncomplicated cystitis, also known as a lower urinary tract infection (UTI), making acute uncomplicated cystitis the most common bacterial infection among this population. Acute uncomplicated pyelonephritis usually occurs as a consequence of ascending acute uncomplicated cystitis. Although often self-limited, acute uncomplicated cystitis takes a significant toll on women and warrants careful consideration. Pyelonephritis carries more potential for serious complications of morbidity, which makes proper empiric treatment very important.
In 2010, the Infectious Diseases Society of America (IDSA), in collaboration with the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), updated their practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis. They took into account in vitro resistance prevalence and the ecological adverse effects of antibiotic therapy.1 These guidelines are limited to premenopausal, non-pregnant women with no known underlying urogenital anatomical problems, nor other serious comorbidity.
Acute uncomplicated cystitis
Acute uncomplicated cystitis is an infection of the lower urinary tract. The classic symptoms are dysuria, urinary urgency, frequent voiding of small volumes of urine and, less commonly, suprapubic pain and gross hematuria. Risk factors for acute uncomplicated cystitis include recent sexual intercourse, diaphragm use with spermicide, and recurrent UTI.2 Physical examination is often unremarkable, making history-taking crucial. Factors that reflect complicated acute cystitis, and therefore are outside the scope of these treatment guidelines, include male gender, history of childhood UTIs, immunocompromised condition, preadolescence, postmenopausal status, pregnancy, underlying metabolic disorders (including diabetes mellitus), and known renal/urological conditions (including renal stones, renal stents, indwelling urinary bladder catheters, neurogenic bladders, and polycystic kidney disease).
However, acute uncomplicated cystitis remains very common, and a healthy, premenopausal, non-pregnant woman presenting with even one of the classic symptoms raises the probability of the diagnosis to 50%.3 Vaginal discharge or irritation makes acute uncomplicated cystitis less likely. One study reported that a new onset of urinary frequency and dysuria in the absence of vaginal discharge or irritation has a positive predictive value of 90% for acute uncomplicated cystitis.3
Urine dipstick testing is convenient and frequently available in the urgent care setting and remains an acceptable alternative to urinalysis and urine microscopy. Discovery of urine nitrite and/or leukocyte esterase on the strip will help confirm a suspicion of acute uncomplicated cystitis. Urine culture is not necessary for this diagnosis.
Escherichia coli is the most common pathogen found in women with acute uncomplicated cystitis, therefore, it is helpful to know the local resistance patterns to E. coli. Unfortunately for urgent care providers, most microbial resistance data are from inpatient labs, capturing a different (i.e., sicker, older) patient population than found in an urgent care center.
First-line empiric treatment of acute uncomplicated cystitis has shifted from fluoroquinolones due to an increase in E. coli resistance in the United States from 3% in 2000 to an alarming 17.3% in 2010.4 Three comparable first-line options—trimethoprim/sulfamethoxazole (TMP/SMX), nitrofurantoin, and fosfomycin (Table 1)—are recommended. As always, antibiotic selection should be tailored to each individual patient.

Fluoroquinolones can be used when drug allergy/intolerance eliminates first-line options (Table 2) or local E. coli resistance to TMP/SMX exceeds 20%. Betalactams such as ampicillin/clavulanate, cefdinir, cefpodoxime) are less likely to be effective and not recommended as empiric first-line treatment for acute uncomplicated cystitis.
Compete resolution of symptoms should occur within 2 weeks and often begins within 36 hours of treatment. Other supportive measures have included increasing water intake and ingestion of cranberry juices and extracts, although there is no evidence that supports the latter.5 Analgesia with ibuprofen or acetaminophen, as well as phenazopyridine (i.e., pyridium 100-200 mg PO every 8 hours) may be helpful.
Factors that should prompt further investigation in acute uncomplicated cystitis are the development of fever (temperature greater than 100.4° F or 38° C), flank pain, hematuria and/or worsening dysuria, urinary urgency, and urinary retention. Consideration must be given to the sequelae of pyelonephritis or other serious intra-abdominal process. Any hemodynamic instability should raise suspicions of urosepsis. Stabilization efforts should be initiated in the urgent care setting with expeditious transfer to an emergency department (ED). Empiric intravenous (IV) antibiotics, when available, can be started once blood and urine cultures are obtained. For urosepsis, the choice of antibiotics should be done in consultation with either the ED or admitting physician and is beyond the scope of this discussion. Fluid resuscitation is frequently needed and should be started immediately. IV fluid management will be discussed later.
Acute Uncomplicated Pyelonephritis
Acute uncomplicated pyelonephritis is a common serious bacterial infection in women and has the highest incidence in women ages 15 to 29. Although acute pyelonephritis can occur in men, children, and pregnant women, it is rare and outside the scope of IDSA antibiotic treatment guidelines.
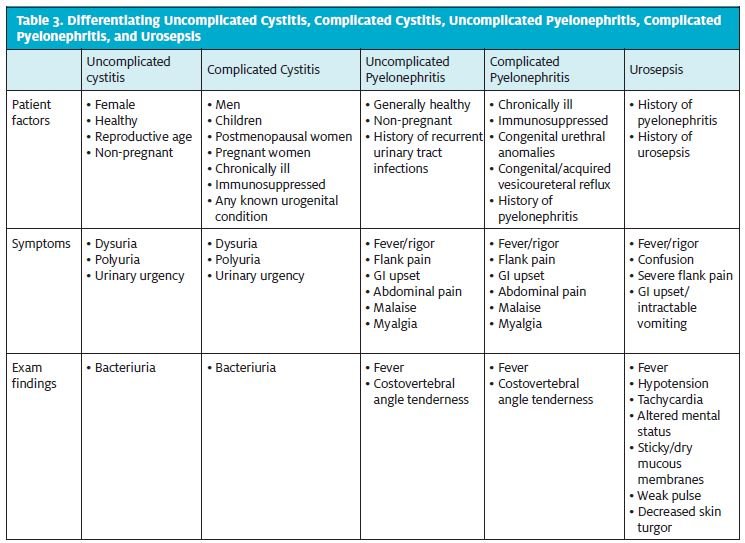
As with acute cystitis, the clinical determination of uncomplicated versus complicated pyelonephritis is based upon a patient’s predisposing factors. Complicated acute pyelonephritis is diagnosed in patients who have a known genitourinary tract abnormality (i.e., vesicourethral reflux, ectopic ureter, congenital ureteropelvic junction obstruction) or other serious predisposing/ chronic medical conditions (Table 3). Complicated cases require careful consideration because of the increased likelihood of non-classic presenting symptoms, broader array of causative pathogens, and progression toward intrarenal/perinephric abscess or emphysematous pyelonephritis.6 Urosepsis, an ascending genitourinary infection that causes hemodynamic instability, is diagnosed based on vital signs (fever, tachycardia, hypotension),physical exam findings (altered mental status, cool or clammy skin, weak pulse) and any other findings suggestive of shock.
Classic symptoms of acute pyelonephritis are sudden onset of dysuria, urinary urgency, urinary frequency, flank pain, fever, nausea, and vomiting. Flank pain is nearly always present. Gross hematuria is rare. On exam, documented fever may be noted but is often absent early in the course. Tenderness on costovertebral angle palpation is very common.
Unlike with acute uncomplicated cystitis, urine culture with microbial susceptibility is necessary in all cases. With the pathogen(s) identified, proper antibiotic adjustment can be made, if needed. Urine dipstick with microscopy is also frequently available and useful at the time of diagnosis in the urgent care setting. In addition to the presence of urine nitrate and leukocyte esterase, white blood cell casts, although infrequently seen, also support the diagnosis. A midstream urine collection is ideal and specific instructions should be offered to the patient before a sample is obtained. Interestingly, several studies have found no significant difference in the amount of contamination in cultures from urine of patients who used preparatory wipes to cleanse the urethral opening and those who did not.7-9 Urinary bladder catheterization is not necessary as long as a midstream sample is collected.8-9
More than 95% of women with acute pyelonephritis will have urine culture that has a single gram-negative organism of greater than 105 colony-forming units. E. coli is the most common pathogen, and less often, other Enterobacteriaceae, Pseudo monas aeruginosa, group B streptococci and enterococci are seen. A baseline serum basic metabolic profile should be obtained to ascertain renal function. Qualitative urine beta human chorionic gonado tropin testing is imperative in any woman of reproductive age. Blood cultures are not needed for uncomplicated acute pyelone phritis in the urgent care setting, and a suspicion of bacteremia warrants emergent evaluation in the ED and likely hospital admission.
Urosepsis and Rapid IV Resuscitation
Urosepsis, one of the most worrisome sequelae of acute pyelonephritis, requires rapid resuscitation to prevent hemodynamic collapse (hypovolemic shock). To prevent permanent ischemic endorgan damage, aggressive crystalloid IV fluids (isotonic 0.9% “normal” saline, lactated Ringer’s solution) should be administered at a rate appropriate for the size of the patient and with some awareness of significant comorbidities (e.g., congestive heart failure). In adolescents and adults, resuscitation with a 1 to 2 liter bolus of IV fluids is reasonable until transfer to a facility with more invasive monitoring is possible. In children, IV normal saline at a rate of 20 mL/kg should be initiated. Electrolyte repletion is typically not indicated until considerable fluids are given and should be done in conjunction with laboratory data (i.e., basic metabolic panel, arterial blood gas).
Although rarely needed, pelvic computed tomography with contrast media is the ideal renal imaging modality for finding a genitourinary structural problem, obstruction, or abscess. Renal ultrasonography and magnetic resonance imaging are also available. Contrast-induced nephropathy remains a concern, particularly for patients with underlying renal disease and/or who are taking potentially nephrotoxic agents, such as metformin.
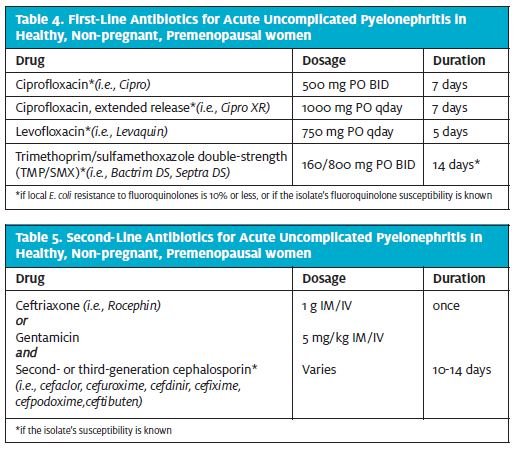
According to IDSA, fluoroquinolones remain the firstline agents for acute pyelonephritis (Table 4). A 14-day course of TMP/SMX also is acceptable in patients who are allergic to or intolerant of fluoroquinolone, and/or if local E. coli resistance to fluoroquinolones is greater than 10%.1 A second-line regimen is a one-time parenteral dose of a third-generation cephalo sporin, followed by a 10- to 14-day course of a second- or third-generation cephalosporin, provided the pathogen susceptibility is known (Table 5).
Clinical improvement should be expected within the first 48 to 72 hours after treatment is initiated. If not, referral to an ED for consideration of hospitalization with IV antibiotics is of paramount importance.
Initial Management of Acute Pyelonephritis During Pregnancy
Although the rates of asymptomatic bacteriuria are roughly the same among pregnant and non-pregnant women, various anatomical and hormonal changes greatly increase the rates of pyelonephritis in pregnant women. During pregnancy the kidneys enlarge and are more engorged with blood, the ureters dilate, the bladder enlarges and is unable to contract as strongly, and loose vesicourethral junctions and a growing gravid uterus conspire to prevent efficient emptying of the bladder.
Acute pyelonephritis in pregnancy, in addition to maternal morbidity, carries higher rates of preterm birth, subsequent low birth weight infants, and higher infant morbidity and mortality, which compel clinicians to keep a low threshold of suspicion about pregnant women who present with urinary concerns.
Acute pyelonephritis in pregnant women warrants parenteral antibiotics initially, usually delivered IV in the inpatient setting. “Mild to moderate” pyelonephritis, in the absence of urosepsis, can be treated with 1 or 2 days of IV antibiotics and a transition to an oral 10- to 14-day regimen (based on culture sensitivity results), provided a patient is afebrile and has shown clinical improvement (Table 6). Ceftriaxone, cefepime, nitrofurantoin and amoxicillin/clavulanate have Class B pregnancy risk classification. The Class B status means they are reasonably safe to use, especially in the second and third trimester, because fetal harm is possible but unlikely.
For patients in whom these ideal regimens are contraindicated, others can be considered. Parenterally, ampicillin 1 to 2 g IV every 6 hours plus gentamicin 1.5 mg/kg IV every 8 hours can be used. Ampicillin and gentamycin are pregnancy Class B and D, respectively. If the causative organism is resistant to nitrofurantoin and amoxicillin/clavulanate, trimethoprim/sulfame thoxazole double-strength (TMP/SMX), 1 tablet PO every 12 hours can be used. TMP/SMX has a Class D pregnancy, classification, which denotes known evidence of fetal risk; however, the risk may (as is the case in acute pyelonephritis) outweigh the fetal risk in serious maternal conditions.
Conclusion
Healthy, non-pregnant, premenopausal woman frequently present to urgent care centers with acute uncomplicated cystitis and pyelonephritis. The evidence-based empiric treatment guidelines set forth by the IDSA make these conditions easily managed using basic urgent care center resources. Acute uncomplicated cystitis should be treated, unless otherwise indicated, with 3 days of double-strength TMP/SMX, 5 days of nitrofurantoin, or a one-time dose of fosfomycin. Acute uncomplicated pyelonephritis should be treated, unless otherwise indicated, with 7 days of ciprofloxacin, 5 days of levofloxacin, or 14 days of double-strength TMP/SMX. Acute pyelonephritis in pregnant women should be treated initially with parental antibiotics, followed by a 10- to 14-day course of oral treatment. Finally, if there is any hemodynamic instability in the setting of a urogenital infection, urosepsis must be considered and the patient treated with appropriate resuscitation with IV fluids and parenteral antibiotics, and transfer to an ED.
References:
- Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011; 52(5):e103-e120.
- Hooton TM, Scholes D, Hughes JP, et al. A prospective study of risk factors for symptomatic urinary tract infection in young woman. N Engl J Med. 1996;335(7):468-474.
- Bent S, Nallamothu BK, Simel DL, Fihn SD, Saint S. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002; 287(20):2701-2710.
- Sanchez GV; Master RN, Karlowsky JA, Bordon JM. In vitro antimicrobial resistance of urinary Escherichia coli isolates among U.S. outpatients from 2000-2010. Antimicrob Agents Chemother. 2012:45(4):2181-2183.
- Jepson RG, Mihaljevic L, Craig J. Cranberries for treating urinary tract infections. Cochrane Database Syst Rev. 2000;(2):CD001322.
- Nicholle LE. Complicated pyelonephritis: unresolved issues. Curr Infect Dis Rep. 2007;9(6):501-507.
- Bradbury SM. Collection of urine specimens in general practice: to clean or not to clean? J R Coll Gen Pract. 1988;38(313):363-365.
- Immergut MA, Gilbert EC, Frensilli FJ, Goble M. The myth of the clean catch urine specimen. Urology. 1981;17(4):339-340.
- Bray PA, Corry MF. Mid-stream urine collection: Is preparatory cleansing essential? N Z Nurs J. 1979;72(3):13-14.

