Urgent message: Abdominopelvic pain is one of the most complex issues encountered in the urgent care settings. Clinicians must make evaluations and decisions rapidly, and it is imperative that they make the appropriate diagnosis to prevent negative outcomes. How this article helps you: assists you in detecting potentially life-threatening problems.
Introduction
Abdominopelvic pain is something that every urgent care provider can relate to. Although urgent care statistics are not readily available, the Centers for Disease Control and Prevention reports that 5.1% of emergency department (ED) visits are because of abdominal pain, whereas 10.9% of all ED diagnoses made are related to the digestive or genitourinary system. More adults visit the ED annually for stomach-related pain or cramps than for any other concern.1 It is reasonable to assume that a similar number of patients, if not more, present to an urgent care center only, or prior to going to an ED. Pain anywhere in the abdomen or pelvis can represent a myriad of potential problems, some of which can be life-threatening.
The task of evaluating this issue can make even the most savvy provider sweat.
Of course there is a great divide between the male and female presentations of abdominopelvic pain and the subsequent evaluations. Given the breadth of the topic, this discussion is broken into two parts. Part 1 focuses on men, with examination of relevant anatomy, medical history, physical examination, testing, and, finally, diagnosis and treatment. Part 2, in this journal’s next issue, will focus on women and will include discussion of pitfalls to avoid in practice.
Consider the case of a 78-year-old man who presents to an urgent care center with a 3-day history of worsening generalized abdominal pain. He had a sudden worsening of the pain the preceding night and now reports associated back pain as well. He denies any nausea, vomiting, diarrhea, or constipation. He says his abdomen feels full, and his legs feel weak. He has never had pain like this before, but he admits that he has not seen his primary-care provider in 5 years. The task for the health-care provider is to tease out the relevant information, to avoid being overwhelmed by the potential seriousness and large differential, and to competently arrive at a decision that will best serve the patient. The relevant anatomy should always be taken into consideration before moving on to pathology and decision-making, and thus male anatomy is discussed next.
Anatomy
Much of what is generally considered the digestive tract passes through or is in some way connected to the abdomen and pelvis. As food and liquid enter the stomach from the esophagus, they cross the diaphragm and enter the abdominal cavity. From the stomach, substances cross into the small intestine, which is broken into three parts—the duodenum, the jejunum, and the ileum. The ileum connects to the large intestines at the ileocecal valve. From there, digestive contents move into the ascending colon, across transverse colon, down the descending colon, into the sigmoid colon, and out through the rectum and anus.
Other organs connect to the intestines along the way to provide various enzymes and to aide in the absorption of important nutrients. The liver secretes bile, which is stored in the gallbladder. The pancreas secretes insulin and other enzymes. The appendix, although having no clinical function, is a site of infection. It attaches to the large intestine near the proximal ileum. The urogenital tract also sits within the abdominopelvic cavity. The bladder and prostate sit above the musculature of the pelvic floor in what is commonly referred to as the true pelvis, the area of the pelvis below the pelvic brim. The inguinal canal opens through the ligamentous and muscular structures of the anterior abdominal wall to connect the testicles to the peritoneal space. The blood supply and ductus deferens pass through the canal. The major vessels that carry blood to and from the abdomen and the lower half of the body also pass through the abdominopelvic cavity—the descending aorta and the inferior vena cava.
The abdominal cavity is wrapped in a serous membrane known as the peritoneum. The peritoneum is better described as a sac in which abdominal organs protrude. The aspect that lines the abdominal wall is the parietal peritoneum, and the aspect into which organs push is the visceral peritoneum. Any organ with only an anterior surface touching the peritoneum is considered retroperitoneal in nature, including the ascending and descending colon, kidneys, ureters, adrenal glands, aorta, inferior vena cava, rectum, esophagus, duodenum, and the pancreas, except for its tail. This leaves the stomach, the first part of the duodenum, the jejunum, ileum, cecum, appendix, transverse colon, sigmoid colon, liver, spleen, and the remainder of the pancreas as intraperitoneal.
Although the heart is separated from the abdomen by the diaphragm, irritation of the heart musculature can cause pain in the upper abdomen, and is thus something the clinician should be aware of.2
Medical History and Physical Examination
Clinical Gestalt
Astute clinicians know that one of their greatest tools is their clinical gestalt. The impression that a clinician gets on meeting an ill patient is difficult to describe, but it can be one of the greatest determining factors when making important decisions. Does the patient look sick or in pain? Is the patient motionless, or thrashing about? Is the patient’s skin flushed or gray? For example, the 78-year-old patient discussed here may look pale or be diaphoretic. Either one of these findings should alert the clinician to a potentially serious problem.
Pain
When eliciting a medical history from the patient, the description of pain can provide key details to the differential diagnosis. Although pain level may show no relationship to the severity of the disease process, the timing of pain onset can be a clue to the diagnosis. Abrupt pain is suspicious for rupture of a hollow organ or potentially a vascular accident. Gradual-onset pain should prompt consideration of infection or inflammatory conditions. The location of pain is also important. Pain can also be referred to and from the abdomen. Irritation of the diaphragm from above because of ischemia of the inferior cardiac wall may cause upper abdominal or epigastric pain. An inflamed gallbladder may irritate the diaphragm from below, causing referred pain to the right shoulder blade.
Associated Symptoms
A thorough review of any associated symptoms is also important:
- Nausea and vomiting preceded by abdominal pain should alert the health-care provider to obstruction, especially if the patient has had prior abdominal surgeries. The presence of vomiting without diarrhea is less likely to be viral gastroenteritis than if both are present.
- Fever can indicate an infectious process and is also important when ruling out sepsis.3,4
- Symptoms of volume depletion such as light-headedness, dry mouth, and headache are especially important in conjunction with vomiting.
- Urinary symptoms such as burning with urination, urgency, frequency, and discharge should obviously alert the clinician to the possibility of a genitourinary infection. In men, special attention should be paid to the prostate and the testicles, and suspicion of a sexually transmitted infection should increase simply because urinary tract infections are not common in men.
- Associated unilateral back or flank pain should cause concern about the possibility of a renal stone.
- Abdominal pain described as tearing through to the back should cause the clinician to evaluate the patient for aortic dissection.
- Reluctance to eat or drink anything occurs in most cases of abdominal pain, but a decrease in pain with oral intake may indicate a peptic ulcer if the pain is in the epigastric region.
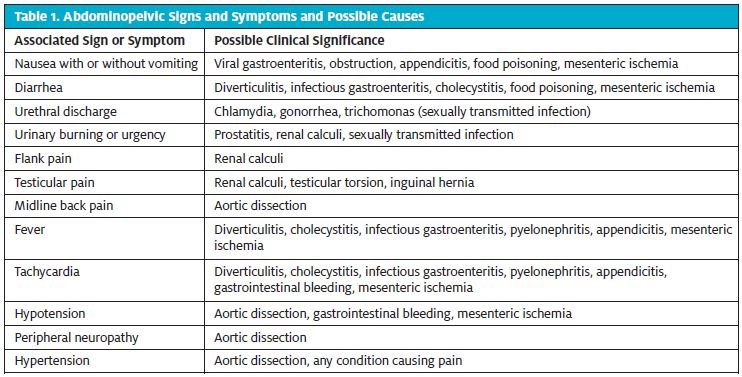
Table 1 lists some associated findings and their possible clinical significance.
 Past Medical History
Past Medical History
A detailed medical history is always necessary. For example, a history of abdominal surgeries increases the risk of obstruction-related adhesions. Medications like opioids can slow gut motility. A history of weight loss and previous cancer is ominous for recurrence or metastasis.
General Physical Examination
Any patient who appears ill should be treated swiftly. Well-trained front-desk and ancillary staff members can help identify and triage acutely ill patients. The physical examination should include the following:
- Assessment of vital signs: Vital signs can play an important role in determining patient prognosis, but sometimes they can be misleading and thus should be taken into context of the complete examination. We all remember the saying “Treat the patient, not the numbers.” Although fever and tachycardia are certainly ominous, 15.6% of adults with acute appendicitis do not have a fever.5 Paradoxical bradycardia can easily delay the diagnosis of abdominal bleeding when free blood irritates the peritoneum, lowering the pulse rate rather than increasing it as expected.6
- Cardiopulmonary examination: A good cardiopulmonary examination can reveal complicating diagnoses like heart failure or provide information about diagnoses that present as abdominal pain, like pneumonia or myocardial infarction.
- Abdominal examination:
- The abdomen should be fully exposed and assessed for any distention, surgical scars, hernias, rashes, and so on.
- Bowel sounds must be identified in all four quadrants, but they cannot be deemed absent until approximately 5 minutes pass without sound. Hyperactivity suggests gastroenteritis or early obstruction, whereas the absence of sound indicates late obstruction or ileus.
- Percussion must be performed, and a normal abdomen should have varying degrees of dullness and tympany. Excess tympany represents free air or increased intraluminal gas. Dullness suggests bleeding or obstruction.
- Palpation should be done from light to deep, with the clinician watching the patient’s face while applying pressure to evaluate for tenderness. Guarding suggests significant pathology, such as bacterial infection. Rigidity is a strong indicator of peritonitis. There may be costovertebral angle tenderness if there are retroperitoneal processes such as renal calculi or pyelonephritis.
Diagnostic Signs
The special tests should be performed next. Because of space limitations, techniques are not described here, but there are plenty of reference works to consult.
- Rebound tenderness indicates peritoneal irritation and is most commonly used in the diagnostic evaluation of appendicitis. When the clinician releases pressure from palpation on the abdomen and the patient experiences this as more painful than the pressure itself, that is a positive finding.
- Rovsing sign indicates peritoneal irritation, and although it is nonspecific, it should be viewed as one of many tools in your toolbox. Its findings are positive when deep palpation on the left side of the abdomen leads to pain on the right side.
- Psoas sign indicates appendicitis that is irritating the psoas muscle posteriorly. It is performed most commonly by asking the patient to lift the right leg against resistance while the patient is prone.
- McBurney point is not an examination but is worth noting as the area midline between the umbilicus and the anterior superior iliac spine. Tenderness here suggests appendicitis.
- Murphy sign suggests inflammation of the gallbladder. Findings are positive when the patient’s breathing arrests during deep palpation of the right upper quadrant. The diaphragm pushes the liver and gallbladder down against the fingertips, producing pain that causes the patient to stop breathing.
- The Markle sign is performed by firmly tapping on the heels of the supine patient, jarring the abdominal cavity enough to elicit pain if there is peritoneal inflammation.
- A prostate examination should at least be considered in all men with abdominal pain, as should testicular and hernia examinations. Although the performance of a prostate examination when there is abdominal pain is supported repeatedly in literature, it is often not completed in the clinical setting. Genital and prostate examinations are uncomfortable and can be embarrassing for some patients. A judicious approach is to perform these examinations anytime an alternative diagnosis is not abundantly clear or if there is concern about the presence of pathology in the reproductive tract, as with urinary hesitancy, deep rectal pain, urethral discharge, testicular pain, or testicular swelling.
- A hernia check should also be considered if there is any concern about possible intestinal obstruction because of bowel incarceration.
Laboratory Testing
The complete blood cell (CBC) count is a commonly ordered but seldom useful test in the urgent care setting. For example, a study7 reported in 2006 showed that of 744 adults with appendicitis, only 64.8% had an elevated white blood cell (WBC) count. The study also showed that a WBC count greater than 12 × 109/L had a positive predictive value for appendicitis of only 84.3%. A normal CBC count should never be used to rule out significant pathology.
The complete metabolic panel has a similar lack of usability in the urgent care. For instance, elevation of serum alanine aminotransferase and aspartate aminotransferase levels has only a 38% sensitivity for determining the presence of acute cholecystitis.8 A serum lipase test should be considered when pancreatitis is suspected. Although classically ordered in tandem with amylase, lipase testing has been shown to be more sensitive and specific to amylase in the setting of acute pancreatitis.9 The lipase test generally ordered in conjunction with computed tomography (CT) imaging if the patient’s condition is otherwise stable. In the absence of urinary tract symptoms (burning with urination, hesitancy, etc.), positive findings on urinalysis (i.e., the presence of WBCs or blood in the urine) should never be used to make clinical decisions about a patient’s condition and readiness for discharge, because both of these findings can result from lower abdominal infection outside of the urinary tract, specifically peritonitis.
Diagnostic Imaging
Plain film radiography has largely been replaced by CT and ultrasonography for investigating abdominal pain. Bowel obstruction remains one of the few diagnoses that can be made on plain film, but studies show that it has limited sensitivity and specificity compared with CT: 77% versus 93% and 50% versus 100%, respectively.10
Ultrasonography has limited use as well, although it can be used to evaluate for splenic enlargement, testicular torsion, epididymitis, and cholecystitis. Focused assessment with sonography in trauma is being used in EDs to evaluate for abdominal free fluid but is not applicable to urgent care. Most importantly, ultrasonography is the imaging modality of choice in evaluation of testicular or inguinal pathology.
CT is the most widely used imaging modality in the investigation of acute abdominal pain, but it also has an increased cost and more radiation exposure for the patient. CT is 97% sensitive for diverticulitis and is the recommended study of choice for pancreatitis, mesenteric ischemia, dissecting aorta, and most other causes of abdominal pain, given its ability to look for severity and complications.11
Diagnosis-Specific Treatment
The following possible causes of abdominal pain in men should always be considered. Listed for each one are treatment plans to think over once the medical history has been obtained, the physical examination has been performed, and the diagnostic work-up has been completed.
- Abdominal aortic aneurysm: Patients suspected of having an abdominal aortic aneurysm should always be transported to an ED via ambulance as soon as possible. The clinician and staff members should prepare for resuscitative measures while awaiting the ambulance. This includes obtaining large-bore (18-gauge or larger) intravenous access and starting oxygen therapy.
- Myocardial infarction: Myocardial infarction should be ruled out in any patient older than 40 years who presents with isolated epigastric pain with no other obvious cause. Given that a simple electrocardiogram is not sufficient to do this, these patients should be referred to an ED, where serial electrocardiograms and cardiac enzyme tests can be ordered.
- Viral gastroenteritis: The diagnosis of viral gastroenteritis should be made only after all other life-threatening diagnoses are appropriately ruled out. It should never be made in the absence of associated diarrhea and/or vomiting. Vomiting alone should make the provider strongly question the diagnosis and continue to investigate, possibly for obstruction or appendicitis. At discharge, the patient should be given clear instructions regarding fluid intake and follow-up care.
- Bacterial gastroenteritis: The full spectrum of bacterial gastroenteritis goes far beyond the scope of this article. However, patients who present with both bloody diarrhea and abdominal pain should be transferred to an ED, where their condition can be stabilized if needed. This is especially true if vital signs show hemodynamic instability.
- Ischemic mesentery: The signs and symptoms of mesenteric ischemia can mimic other abdominal problems, with sudden onset of pain, pain that sometimes worsens with eating, and pain that is sometimes associated with bloody diarrhea. Clinicians should maintain a high index of suspicion when assessing patients older than 60 years or those who have risk factors such as atrial fibrillation, clotting disorders, or concurrent vasculitis. These patients need CT angiography and close monitoring in an ED.12
- Small and large bowel obstruction: If a bowel obstruction is confirmed via imaging, the patient should likely be transported to an ED. Some emergency-medicine providers may argue that partial obstructions can be managed on an outpatient basis, but this decision is best left to ED providers rather than attempted in the urgent care setting.
- Appendicitis: Appendicitis is an acute surgical emergency. If the clinician strongly suspects that appendicitis is present, the patient should be transported to an ED without delay, prior to imaging studies. If suspicion is relatively low and the patient’s pain level is tolerable, CT imaging with intravenous and oral contrast should be ordered immediately, and the patient should be instructed to proceed to an ED if the pain worsens.
- Diverticulitis: Although the standard of care calls for obtaining CT imaging of the abdomen, many patients who have had repeated episodes of diverticulitis are very aware of the symptomatology and can be treated with appropriate antibiotics, provided that they have no signs of critical illness and provided that appropriate follow-up care has been arranged. If the patient has never had diverticulitis, a CT scan with oral and intravenous contrast is warranted to confirm the diagnosis.
- Cholecystitis: In a patient in stable condition who does not need narcotic pain relief, the work-up for cholecystitis, which consists of right upper quadrant ultrasonography and metabolic laboratory testing, can be done on an outpatient basis. Once the diagnosis is made, however, this patient should either be admitted to a hospital surgical service or transferred to an ED, depending on what local institutional guidelines specify.
- Pancreatitis: Acute pancreatitis can range from mild discomfort to exquisitely painful. If tolerable, a CT scan of the abdomen should be ordered along with a serum lipase test. If pancreatitis is confirmed, the patient should either be referred to an ED or directly admitted to a hospital, depending on what institutional guidelines specify.
- Prostatitis: Outside of urosepsis, acute bacterial prostatitis can be treated on an outpatient basis with appropriate follow-up with urgent care or, preferably, primary care. Treatment for 6 weeks with Bactrim DS (trimethoprim-sulfamethoxazole) or ciprofloxacin is needed to adequately penetrate the prostate.
- Inguinal hernia: An incarcerated hernia or strangulated inguinal hernia can cause pain that radiates into the abdomen, and both are surgical emergencies. Transfer the patient to an ED if the presence of such a hernia is strongly suspected or is confirmed by ultrasonography or CT.
- Peptic ulcer: Diagnosis of a peptic ulcer is typically made by endoscopy and treated with proton pump inhibitors with or without antibiotics, depending on the cause. A bleeding ulcer, however, can cause serious complications, including anemia and peritonitis from perforation. Patients in whom peptic ulcer disease is suspected but who show no evidence of complications should be referred for outpatient treatment to a gastroenterologist and treated with proton pump inhibitors. Signs of peritonitis, anemia on a CBC count, or signs of bleeding on a CT scan should result in transfer to an ED.
- Constipation: The diagnosis of constipation should never be made in the urgent care setting unless all other possible causes of pain have been ruled out. In such a case, give clear follow-up instructions need and document them well. Use of bulk-forming laxatives or polyethylene glycol is safe. Other osmotic laxatives must be prescribed with caution because of the risk of dehydration.
Case Dispensation
The patient described in the beginning of this article was quickly triaged and roomed by a medical assistant. The physician assistant did a brief assessment of his appearance and vital signs. The patient was tachycardic, and his blood pressure was elevated. The physician assistant used this information, along with the patient’s description of the pain, to decide that the patient’s condition was serious. The physician assistant did a thorough abdominal examination and noted a left-of-midline pulsatile mass above the umbilicus. The area was tender to palpation. He immediately arranged to transfer the patient to an ED for CT angiography, which revealed a dissecting aorta.
Conclusion
Not every patient with abdominal pain will present with life-threatening signs and symptoms. Not every diagnosis will be clear or lifesaving. More often than not, the patient will be sent home and will make a full recovery. The keys to avoiding critical errors and detecting potentially life-threatening problems are obtaining a thorough medical history and conducting a detailed physical examination, supplementing with the appropriate diagnostic laboratory tests and imaging. Part 2 of this article will discuss the abdomen and pelvis in women and delve more deeply into discharge care and instructions.
Citation: Fischer TL. Abdominopelvic pain, part 1: approach to med in the urgent care setting. J Urgent Care Med. September 2016. Available at: https://www.jucm.com/abdominopelvic-pain-part-1-approach-men-urgent-care-setting/.
References
- National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. Atlanta, GA: Centers for Disease Control and Prevention [updated 2015 November 6; cited 2015 October 21]. Available from: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf
- Morton DA, Foreman K, Albertine KH. Overview of the abdomen, pelvis, and perineum. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011. Available from: http://accessmedicine.mhmedical.com/content.aspx?bookid=381&Sectionid=40140013. Accessed December 24, 2015.
- O’Brien M. Acute abdominal pain. In: Tintinalli JE, Stapczynski J, Ma O, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th edition. New York, NY: McGraw-Hill; 2011. http://accessmedicine.mhmedical.com/content.aspx?bookid=348&Sectionid=40381541. Accessed December 24, 2015.
- Bork S, Ditkoff J, Hang B. Nausea and vomiting. In: Tintinalli JE, Stapczynski J, Ma O, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th edition. New York, NY: McGraw-Hill; 2011. http://accessmedicine.mhmedical.com/content.aspx?bookid=348&Sectionid=40381542. Accessed December 24, 2015.
- Monneuse O, Abdalla S, Pilleul F, et al. Pain as the only consistent sign of acute appendicitis: lack of inflammatory signs does not exclude the diagnosis. World J Surg. 2010;34:210–215.
- Thomas I, Dixon J. Bradycardia in acute BMJ. 2004;328:451–453.
- Lee SL, Ho HS. Acute appendicitis: is there a difference between children and adults? Am J Surg. 2006;72:409–413.
- Roe J. Clinical assessment of acute cholecystitis in adults. Ann Emerg Med. 2006;48:101–103.
- Smith RC, Southwell-Keely J, Chesher D. Should serum pancreatic lipase replace serum amylase as a biomarker of acute pancreatitis? ANZ J Surg. 2005;75:399–404.
- Suri S, Gupta S, Sudhakar PJ, et al. Comparative evaluation of plain films, ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol. 1999;40:422–428.
- Jacobs DO. Diverticulitis. N Engl J Med. 2007;357:2057–2066.
- Stern SC, Cifu AS, Altkorn D. Abdominal pain. In: Stern SC, Cifu AS, Altkorn D, Symptom to Diagnosis: An Evidence-Based Guide. 3rd edition. New York, NY: McGraw-Hill; 2014. Available from: http://accessmedicine.mhmedical.com/content.aspx?bookid=1088&Sectionid=61696569. Accessed November 20, 2015.

